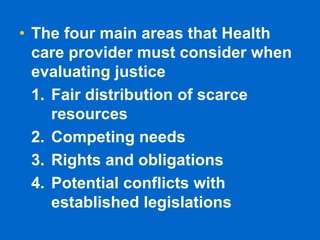
Medical ethics are based on moral principles of determining what is good, bad, right and wrong. They are not the same as feelings, religion, laws, or social norms. The four basic principles of medical ethics are autonomy, beneficence, non-maleficence, and justice. Autonomy refers to a patient's freedom to make their own healthcare decisions. Beneficence means acting in the patient's best interest by providing treatment intended to do good. Non-maleficence is the idea of "first, do no harm" and ensuring procedures do not harm patients. Justice concerns the fair distribution of scarce health resources.