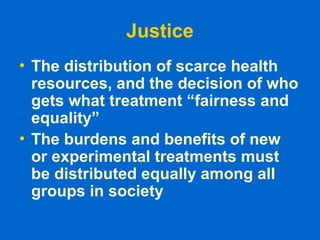
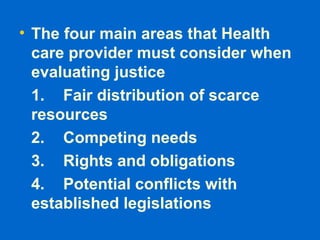
The document provides an introduction to medical ethics, emphasizing that ethics is distinct from feelings, religion, laws, and science. It outlines four basic principles of medical ethics: autonomy, beneficence, non maleficence, and justice, highlighting the physician's duty to respect patient autonomy while also considering their well-being and societal responsibilities. Additionally, it addresses the implications of these principles in clinical practice, particularly regarding decision-making and the allocation of health resources.