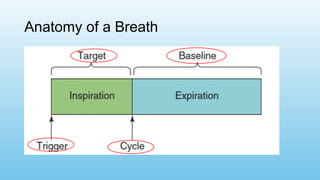
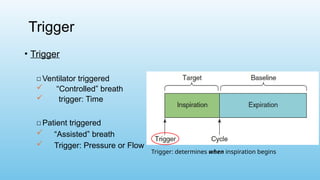
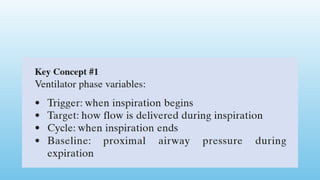
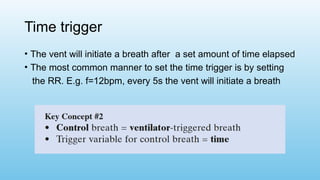
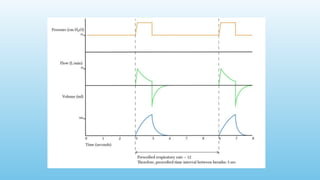
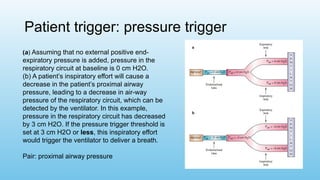
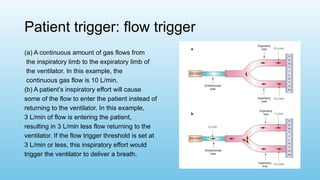
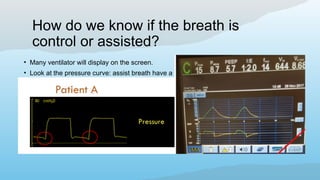
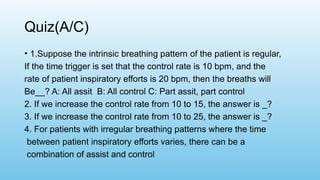
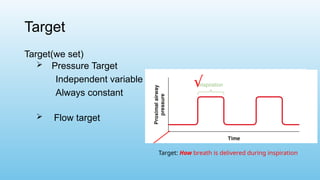
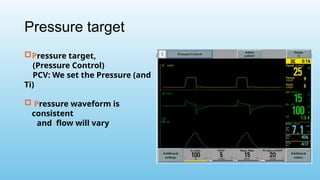
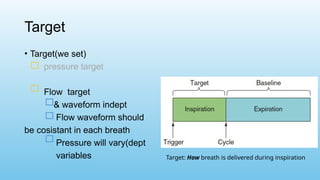
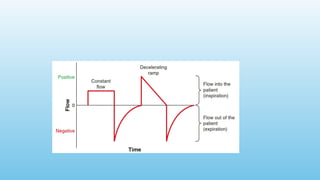
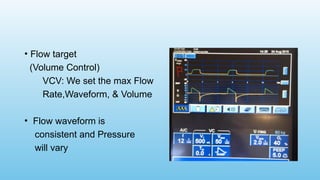
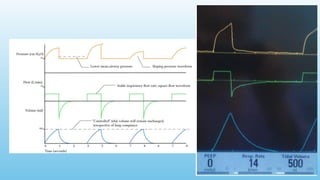
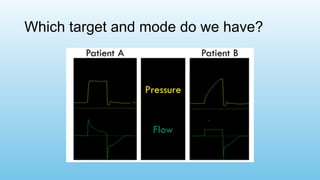
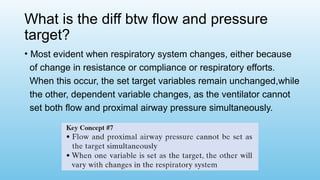
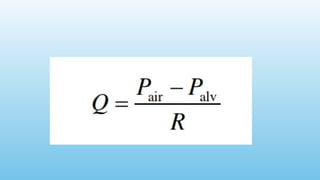
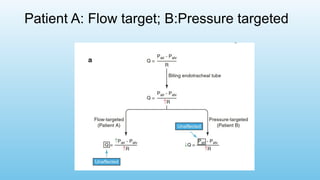
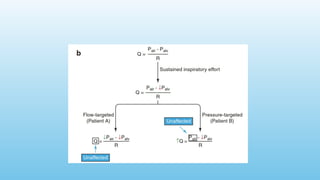
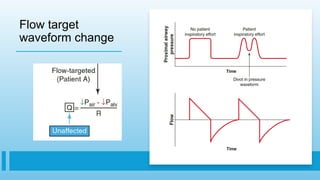
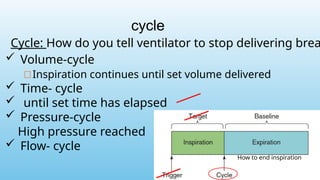
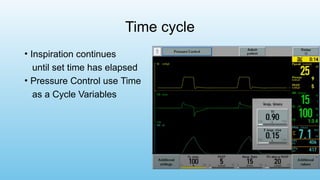
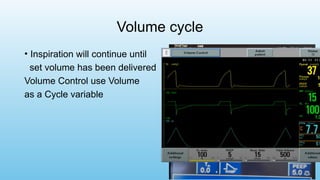
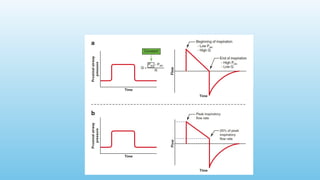
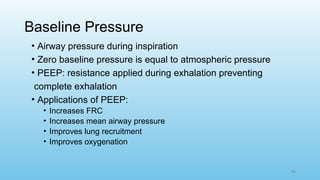
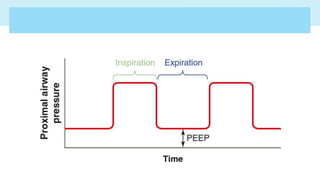
The document outlines the basics of mechanical ventilation, detailing the anatomy of a breath, including the phases of triggering, controlling flow, and determining how breaths are cycled and expired. It discusses different triggering methods—time, pressure, and flow—and emphasizes the importance of assist-control modes in facilitating patient-ventilator interaction. Additionally, it covers the implications of different pressure and flow targets, how they affect ventilatory mechanics, and their relevance in various clinical scenarios.