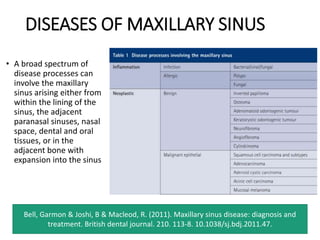
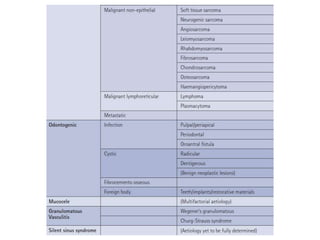
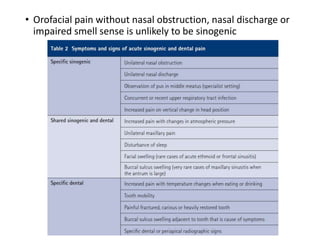
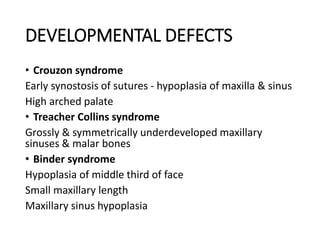
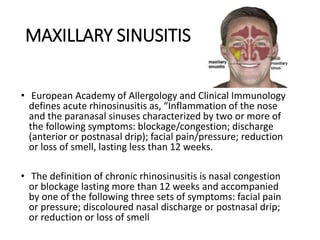
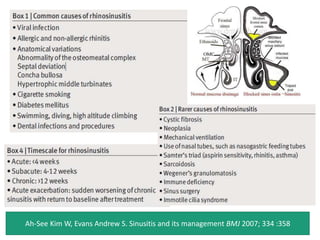
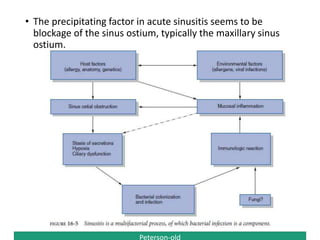
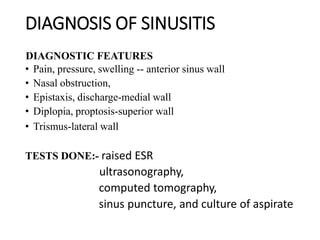
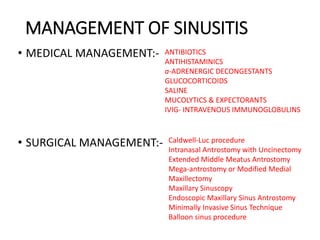
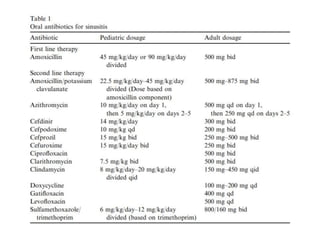
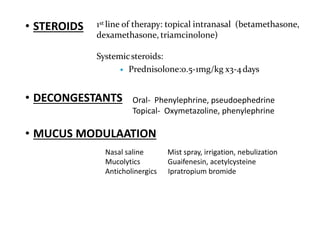
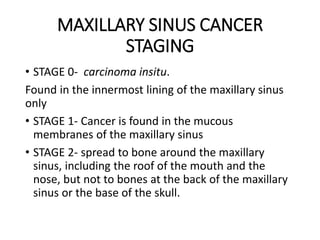
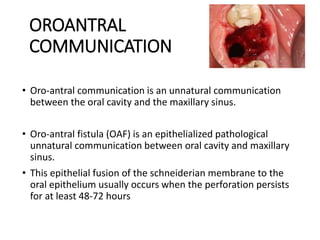
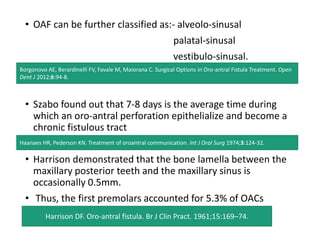
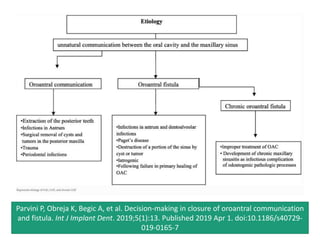
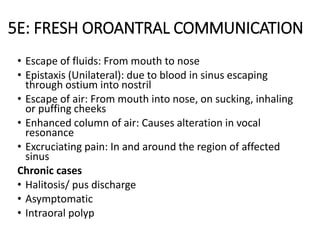
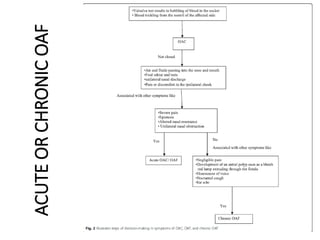
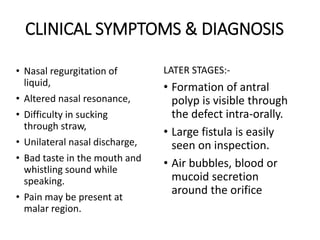
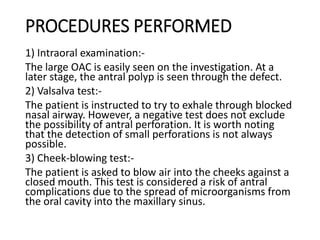
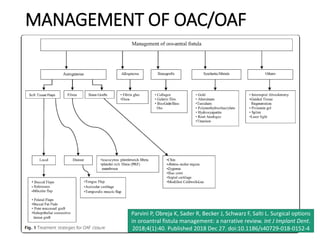
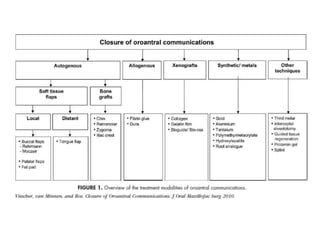
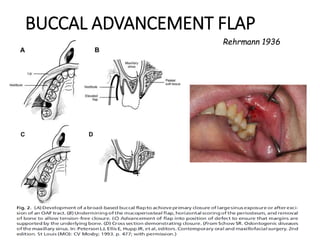
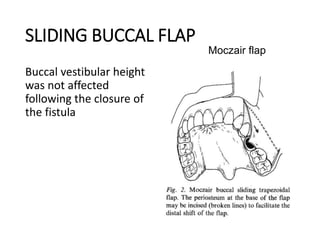
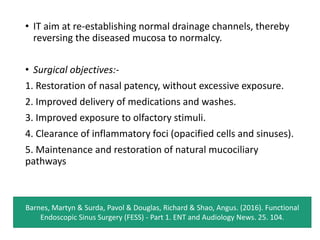
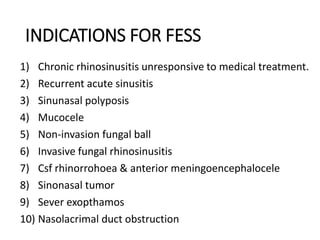
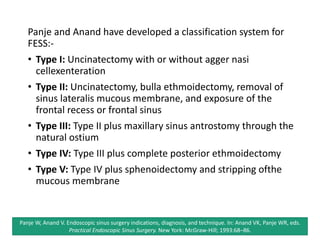
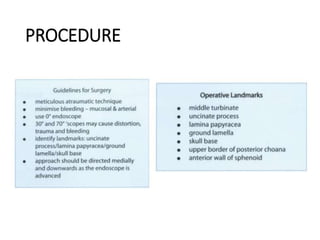
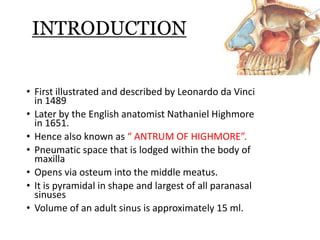
The document provides an extensive overview of the maxillary sinus, covering its embryology, anatomy, drainage, and various diseases, including maxillary sinusitis and fungal infections. It discusses the developmental changes of the maxillary sinus, its anatomical relationships with surrounding structures, and the clinical implications of infections and tumors. Management strategies for sinusitis, tumors, and complications such as oroantral communications are also explored, along with descriptions of diagnostic and surgical interventions.

![APPLIED ASPECT OF MAXILLARY
SINUS
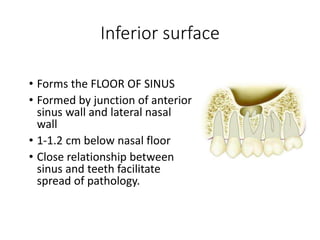
• Floor of sinus: Close relation to root apices
Facilitates spread of infection from teeth
[Endo – antral syndrome, Selden (1974)]
Oroantral Fistula formation.
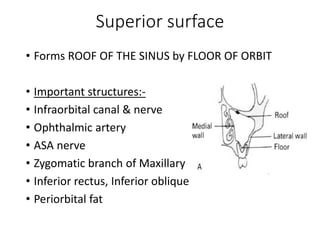
•Superior wall: vulnerable to trauma, Erosion by
tumor
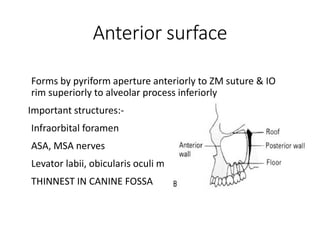
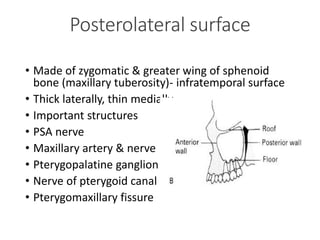
•Posterolateral wall: borders Pterygopalatine fossa,
Infratemporal fossa](https://image.slidesharecdn.com/mymaxillarysinus-200808111450/85/Maxillary-sinus-by-Dr-Shivani-Taank-20-320.jpg)