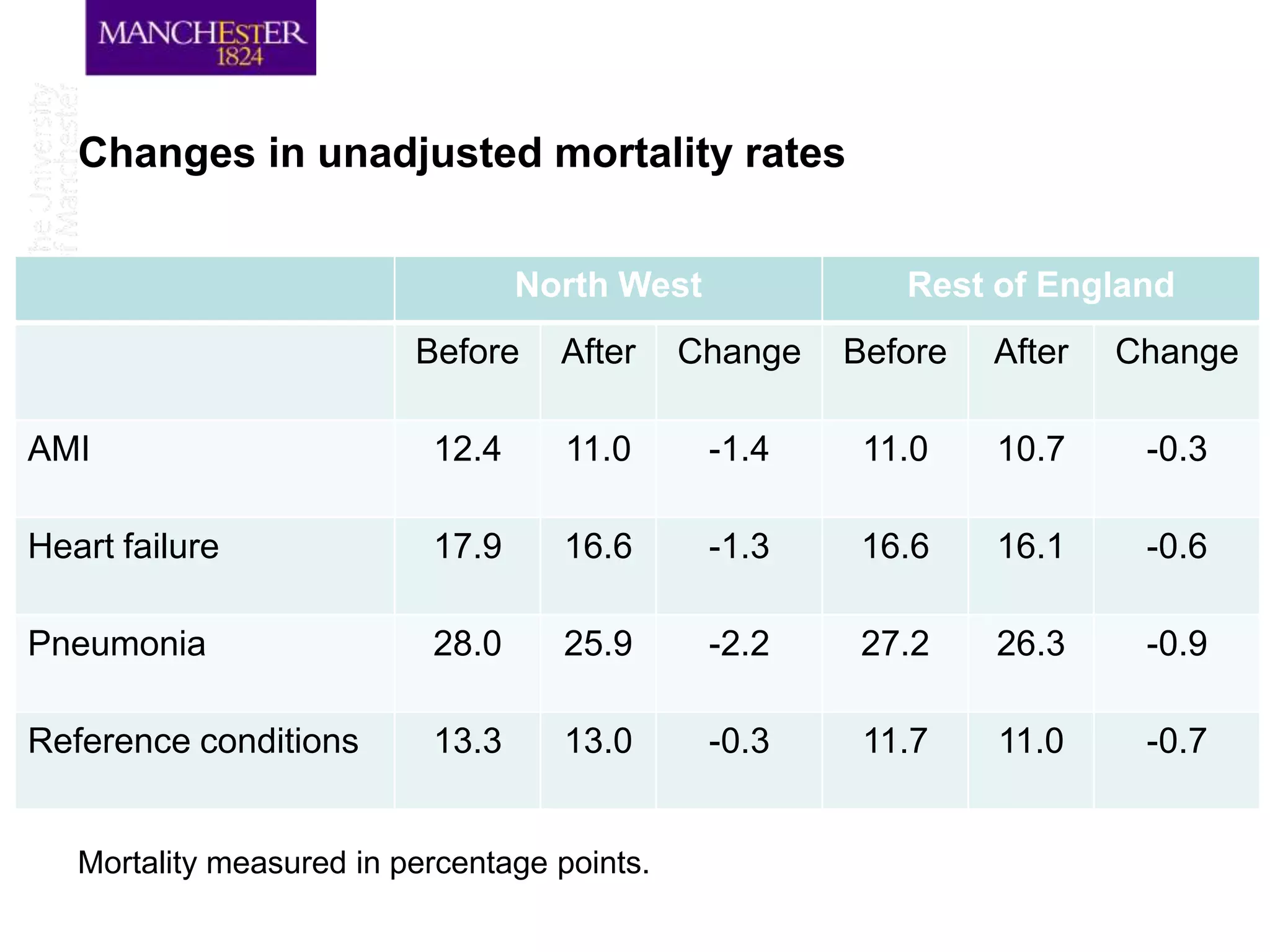
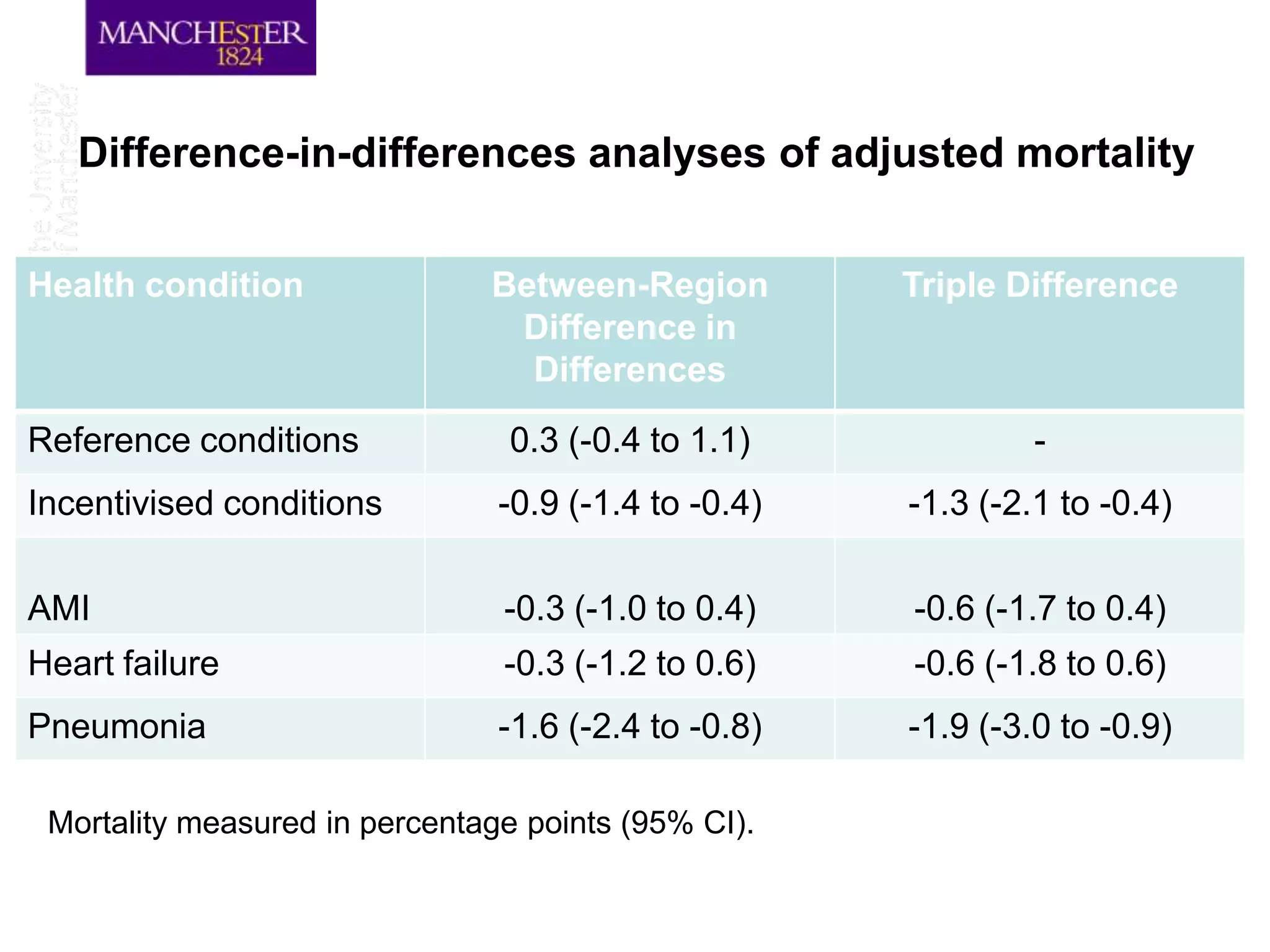
The document discusses a hospital pay-for-performance (P4P) scheme implemented in England, which aimed to improve healthcare outcomes by linking provider payments to quality indicators. An evaluation showed that this initiative resulted in a significant reduction in mortality rates by 1.3 percentage points over 18 months, equating to approximately 890 fewer deaths among patients with specific incentivized conditions. Overall, the scheme demonstrated cost-effectiveness and highlights the potential for P4P models to improve healthcare quality when designed and implemented effectively.