The document discusses value-driven healthcare in Medicaid and outlines several strategies and initiatives to improve quality of care, including:
1) Using evidence-based practices and quality measurement, health IT, and partnerships to ensure safe, effective, timely and equitable care.
2) Promoting transparency of quality and price information to support value-based payment models.
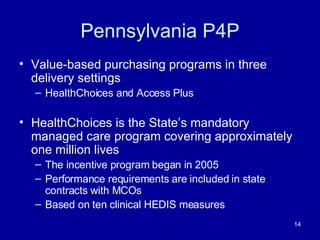
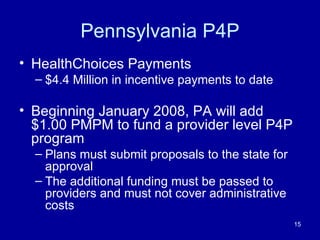
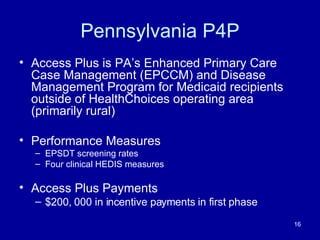
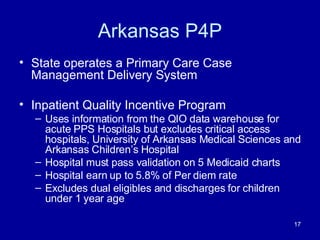
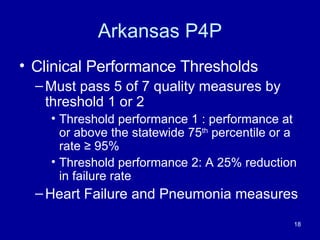
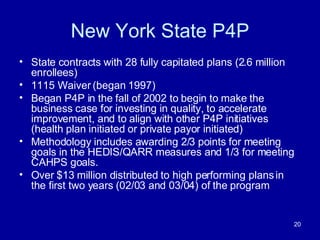
3) Providing incentives for high-quality, high-value care through pay-for-performance programs and other initiatives.
4) Collaborating across states and with CMS to share best practices around quality improvement, health IT adoption, and value-based purchasing.