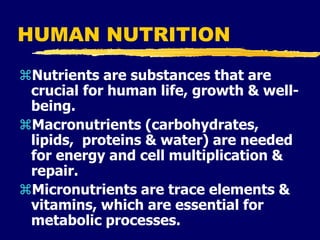
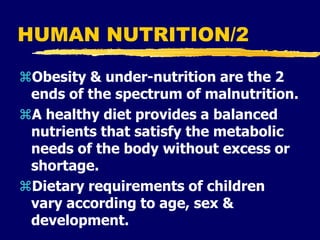
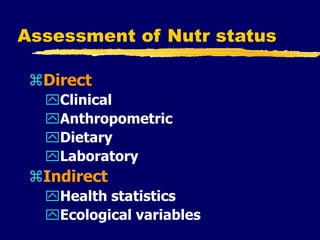
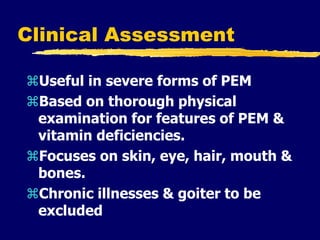
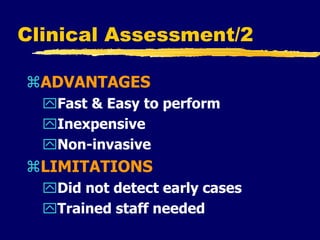
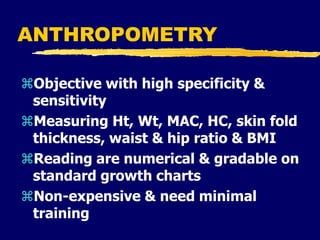
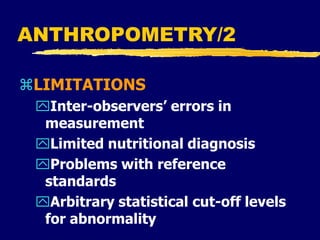
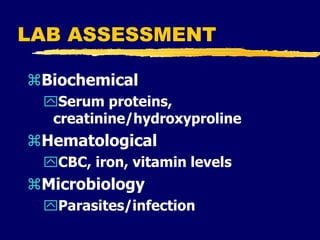
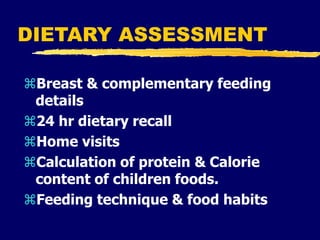
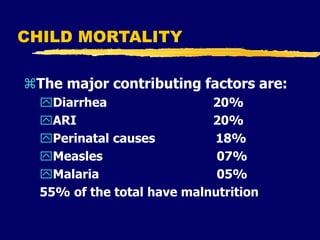
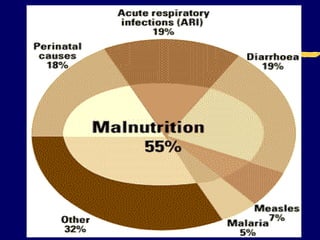
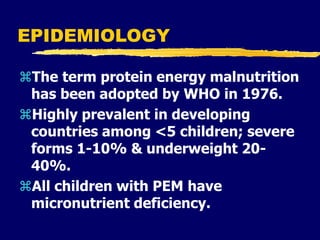
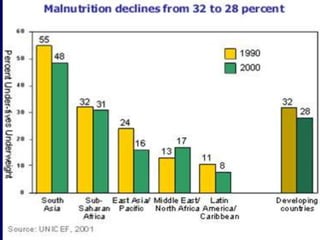
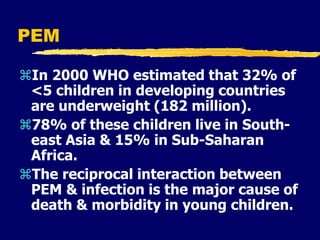
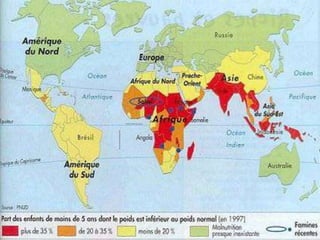
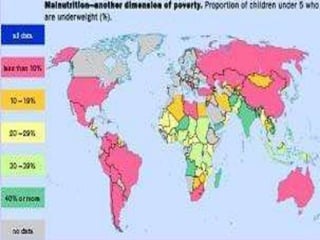
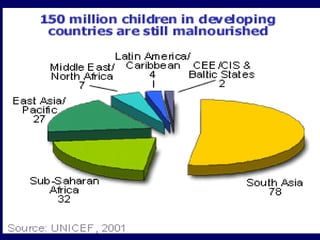
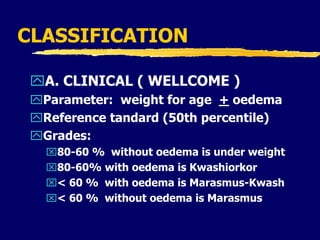
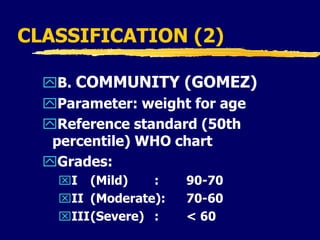
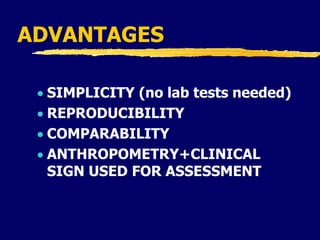
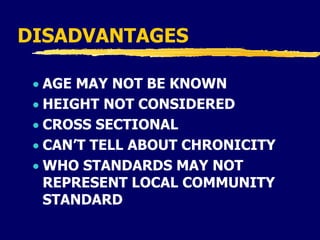
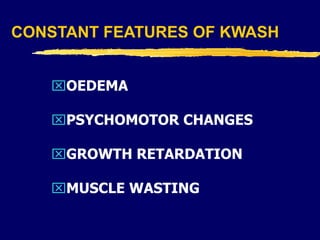
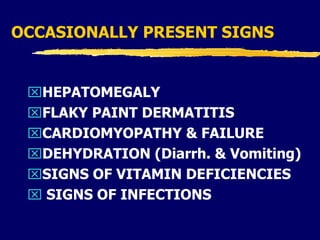
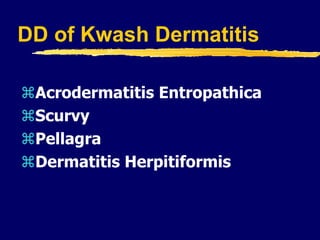
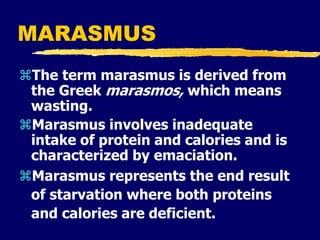
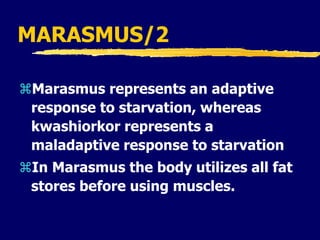
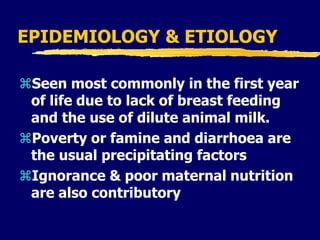
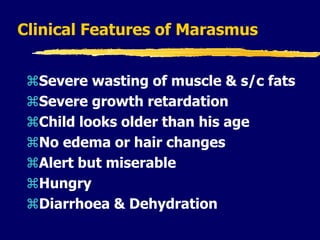
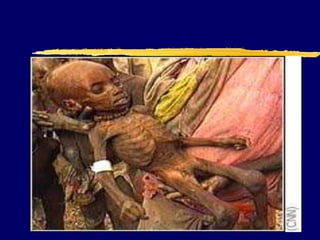
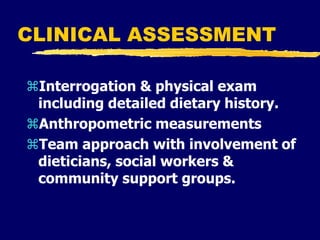
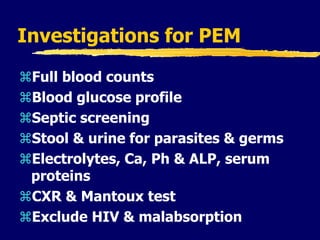
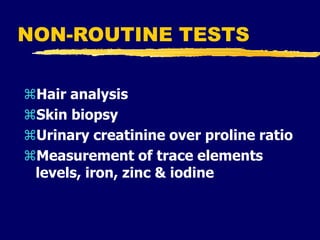
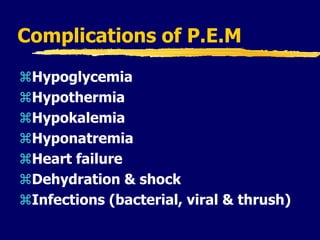
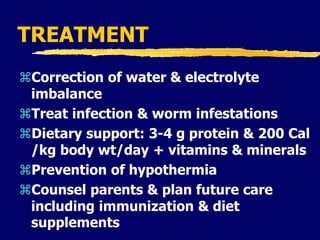
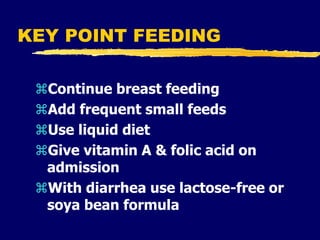
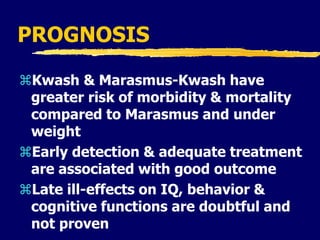
This document discusses protein energy malnutrition (PEM). It defines PEM and describes its causes as lack of food, inadequate breastfeeding, infections, and diarrhea. Clinical features of kwashiorkor and marasmus are provided. Kwashiorkor is characterized by edema, skin changes, and psychomotor retardation. Marasmus involves severe wasting without edema. Assessment methods like clinical exam, anthropometry, and laboratory tests are outlined. Treatment focuses on rehydration, nutrition, and managing infections. Early detection and management are important for improving prognosis of PEM.