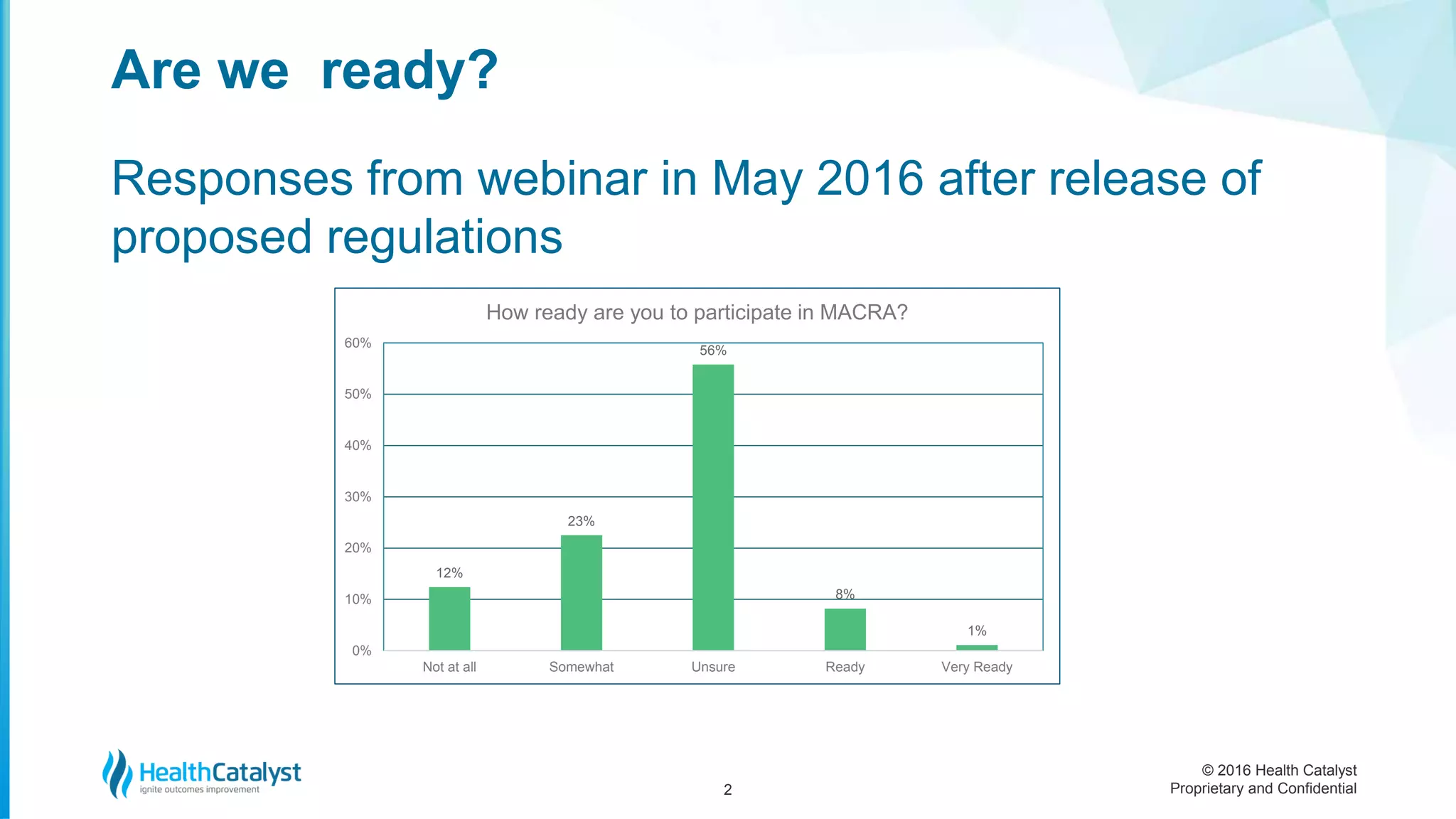
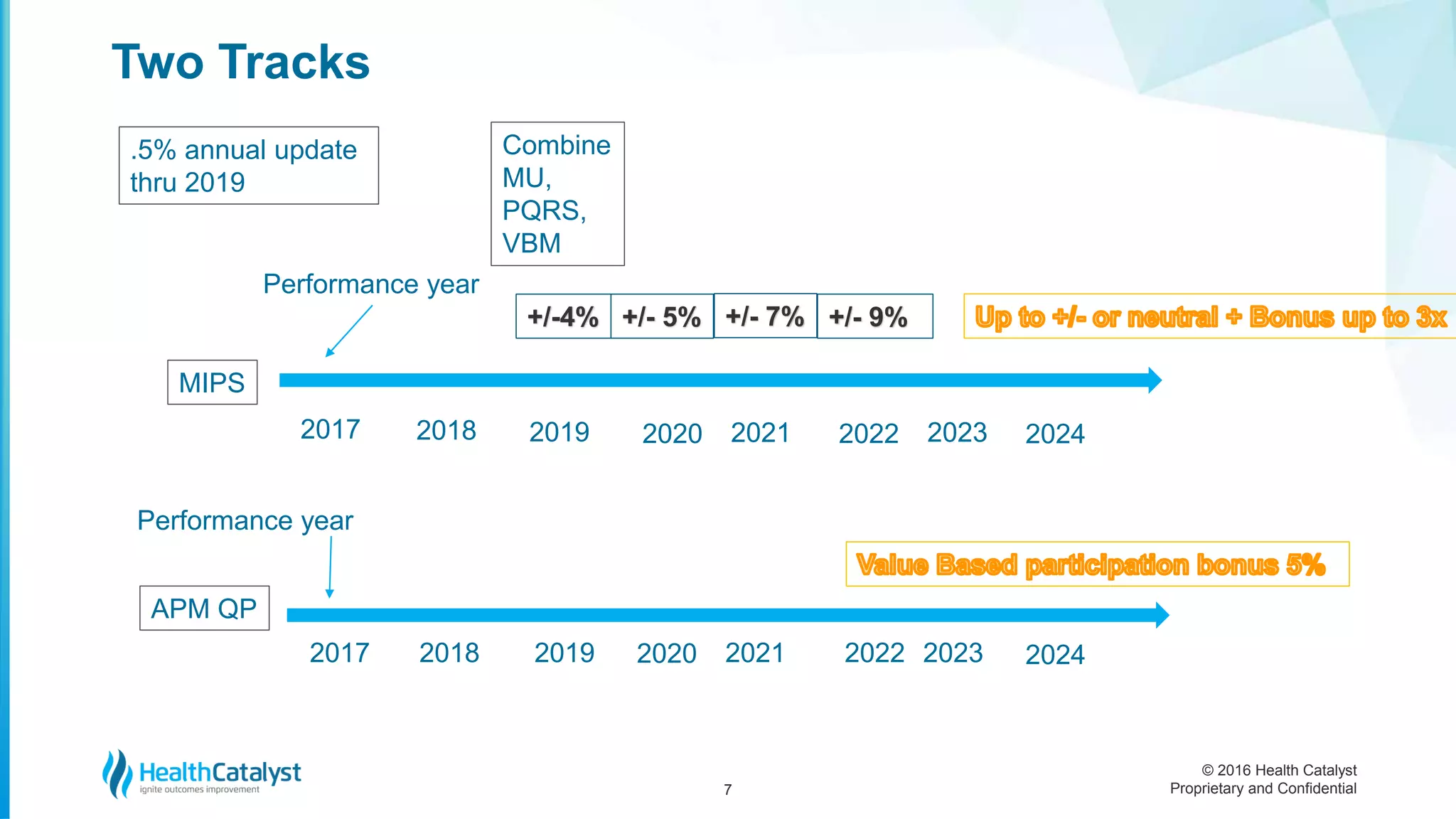
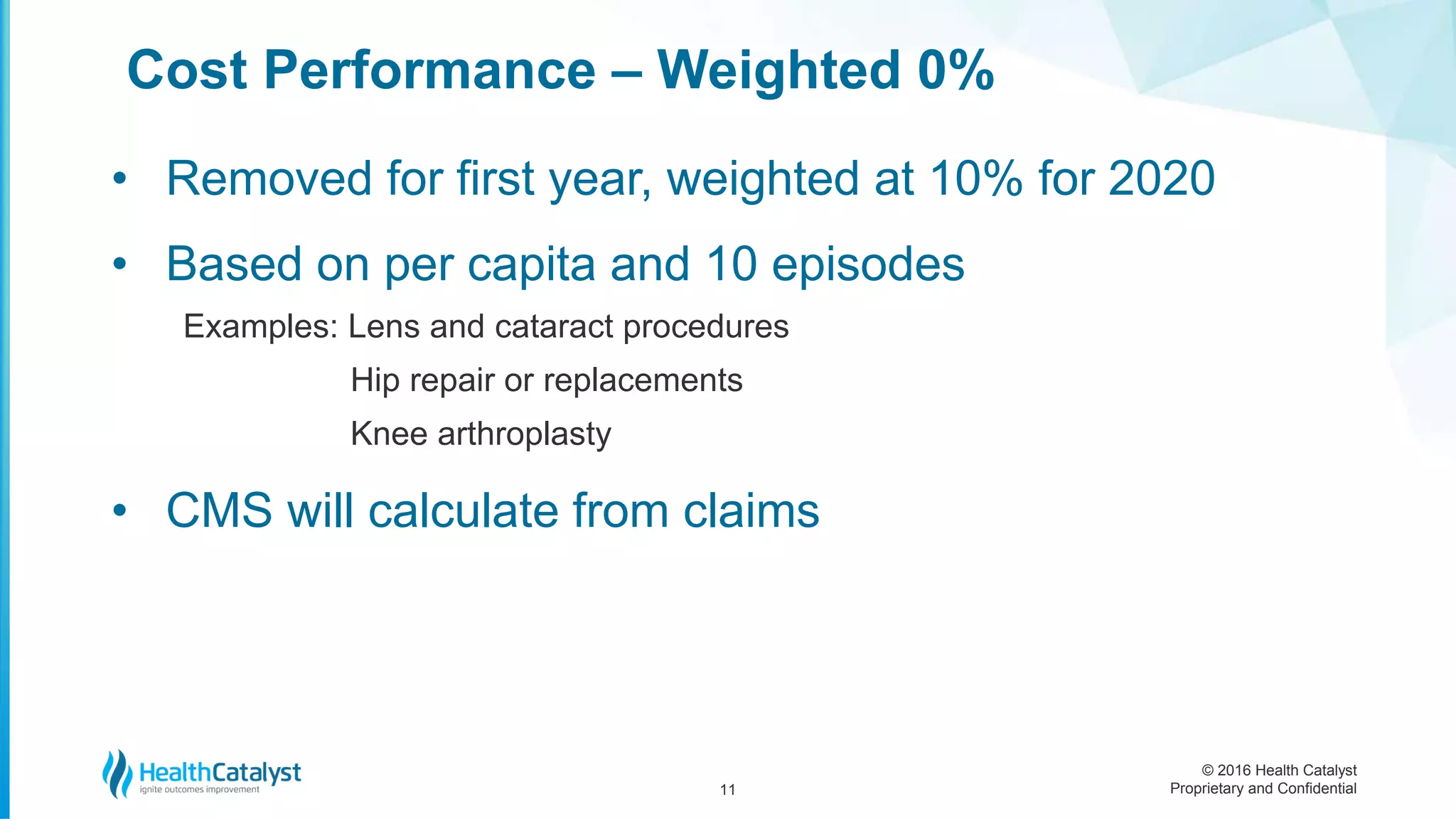
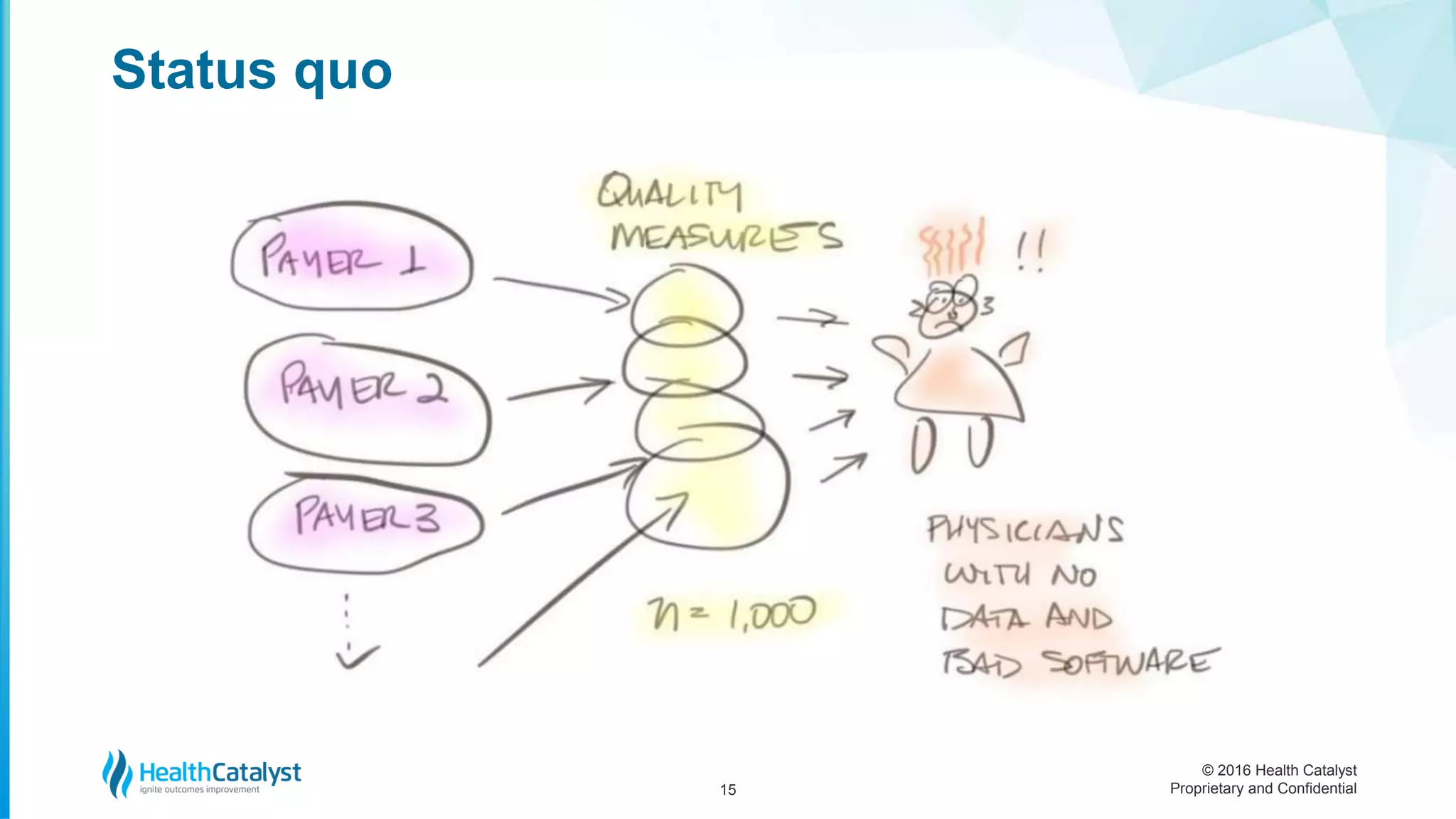
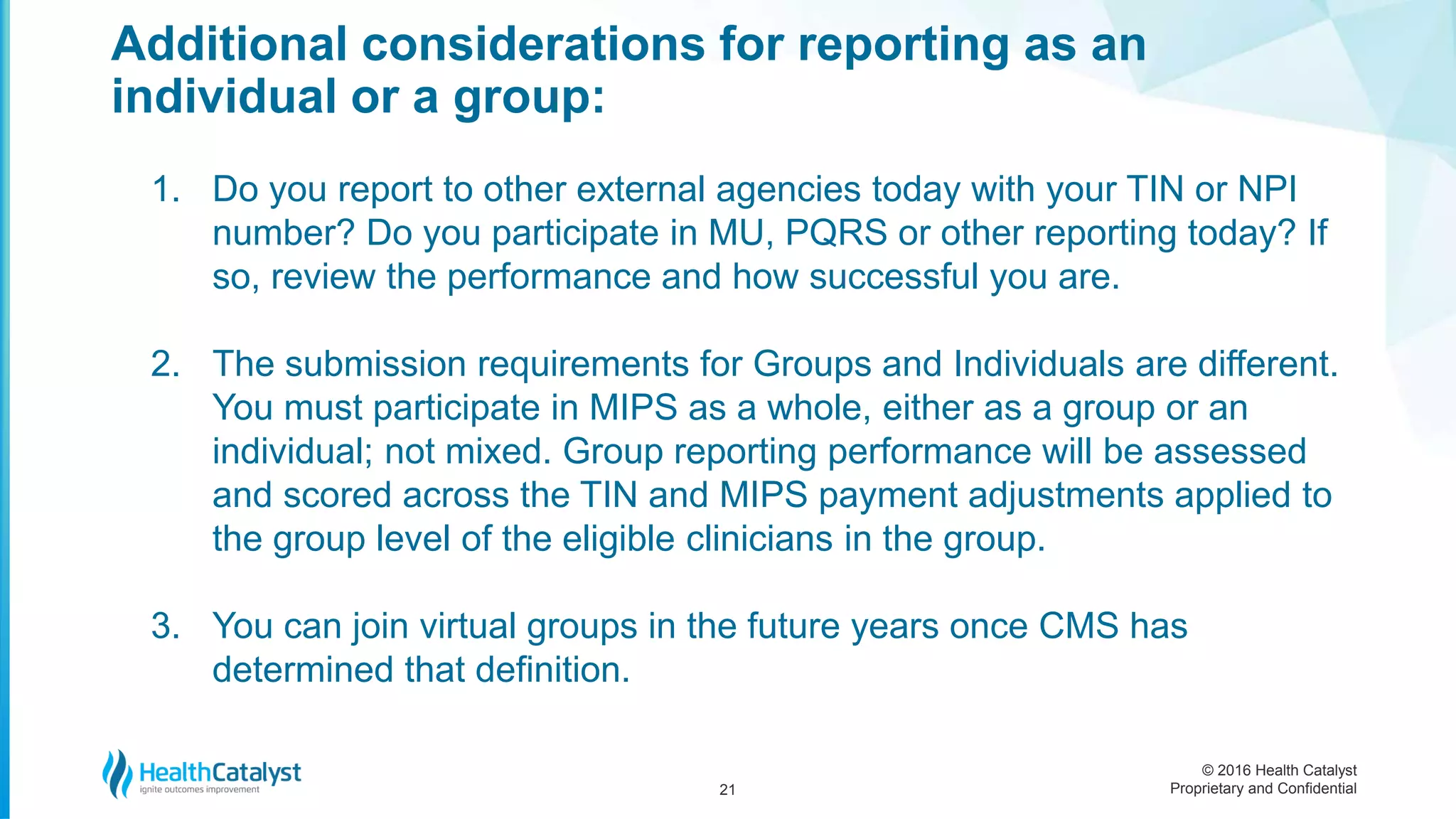
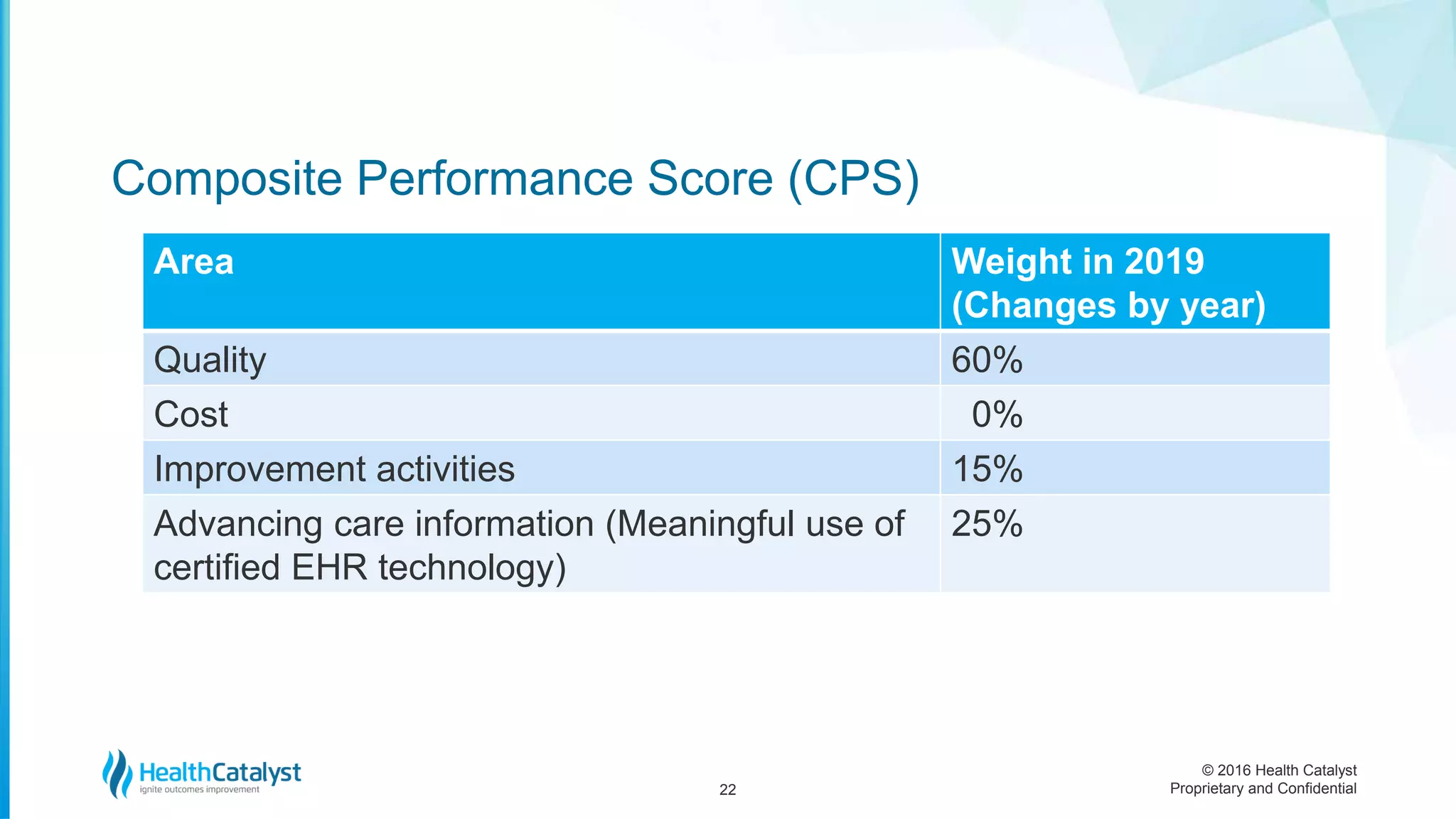
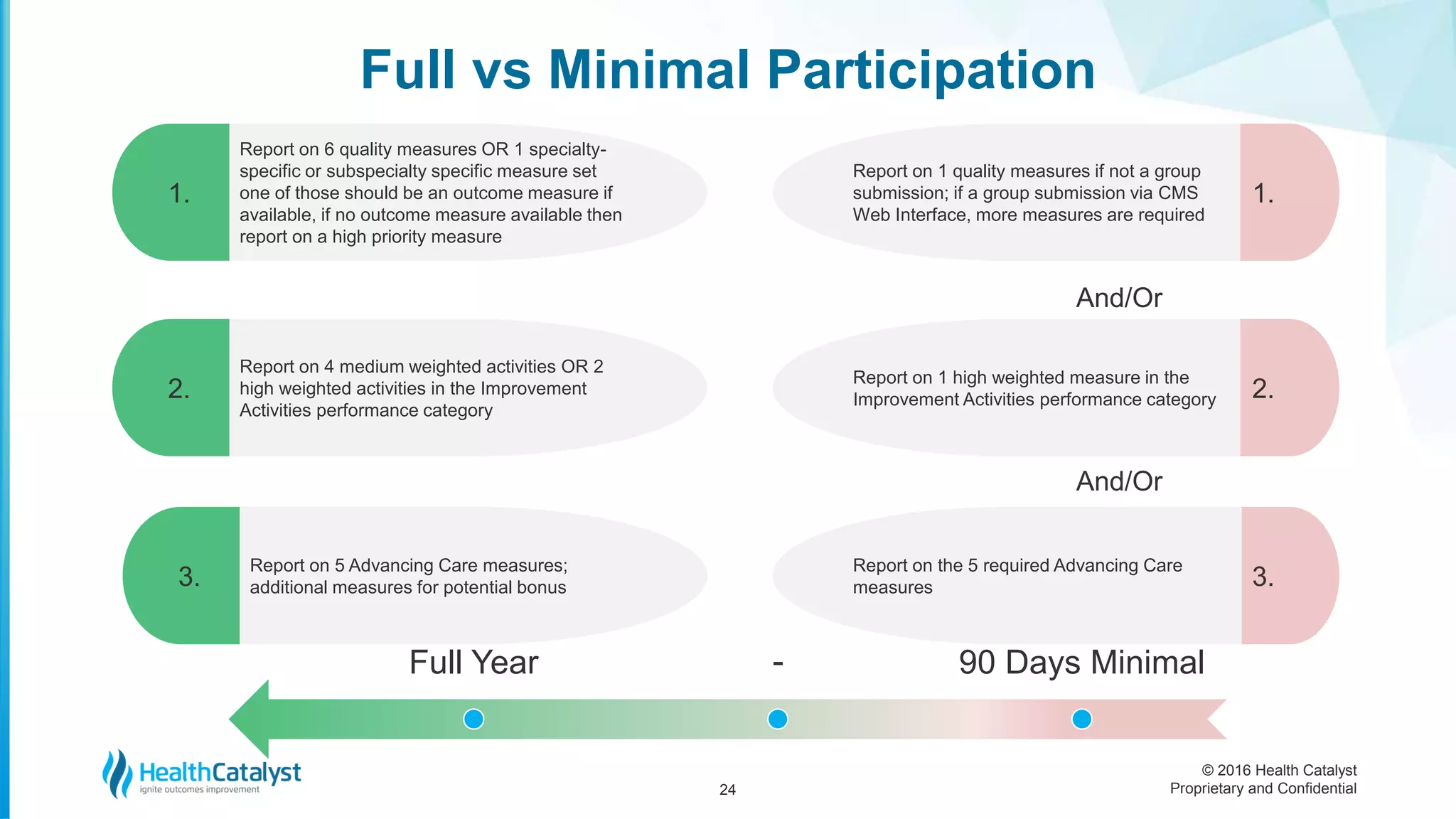
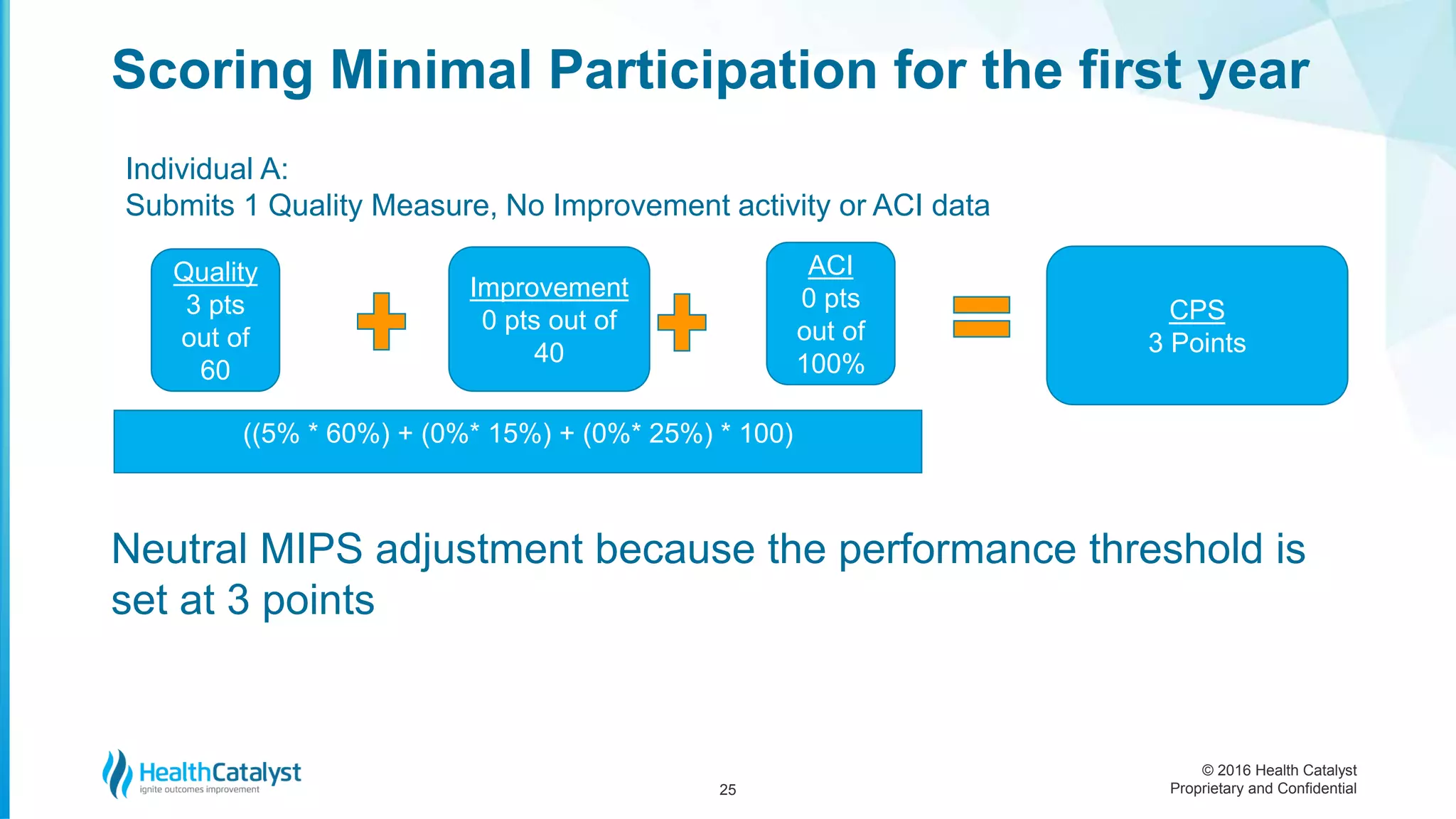
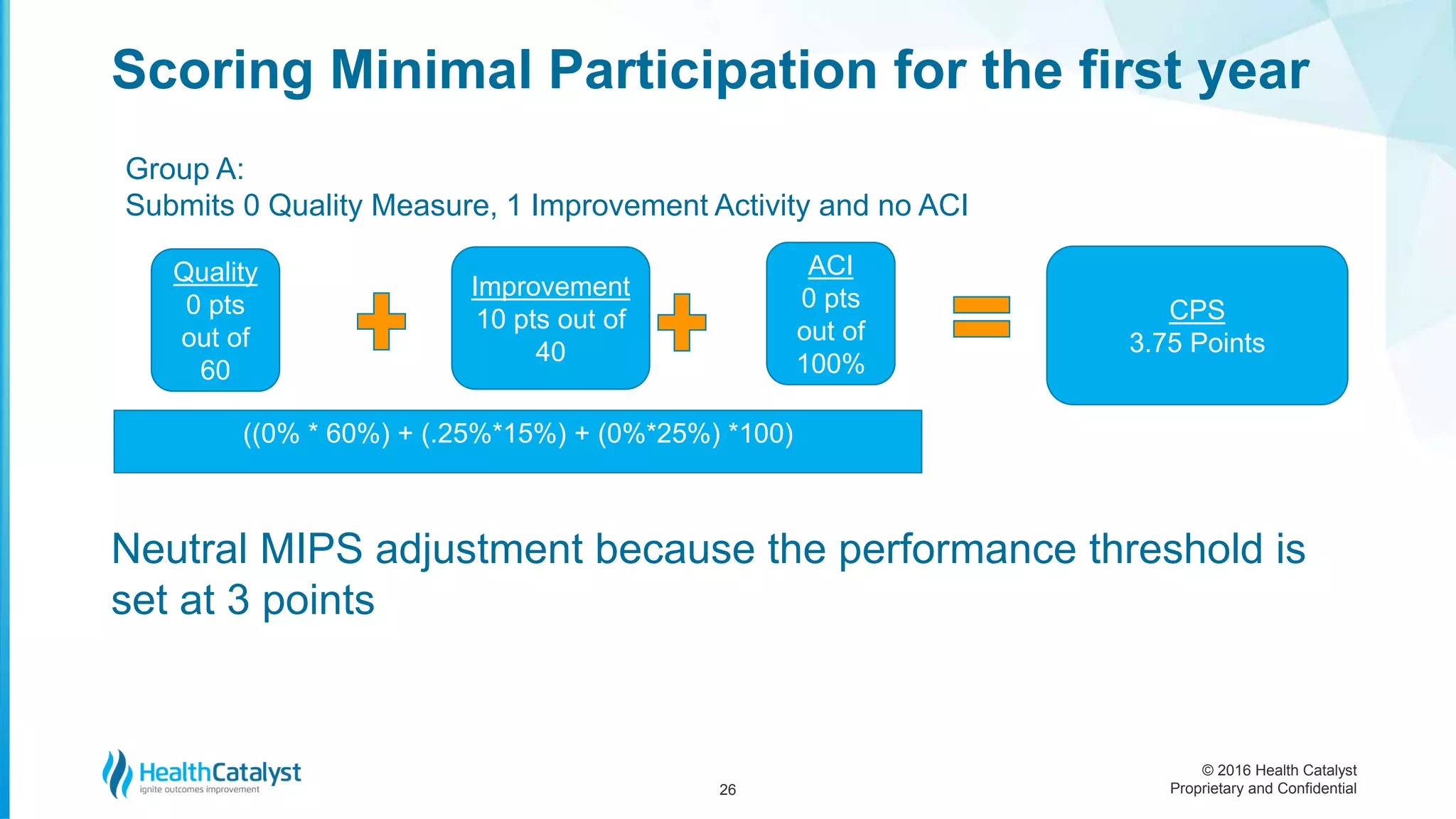
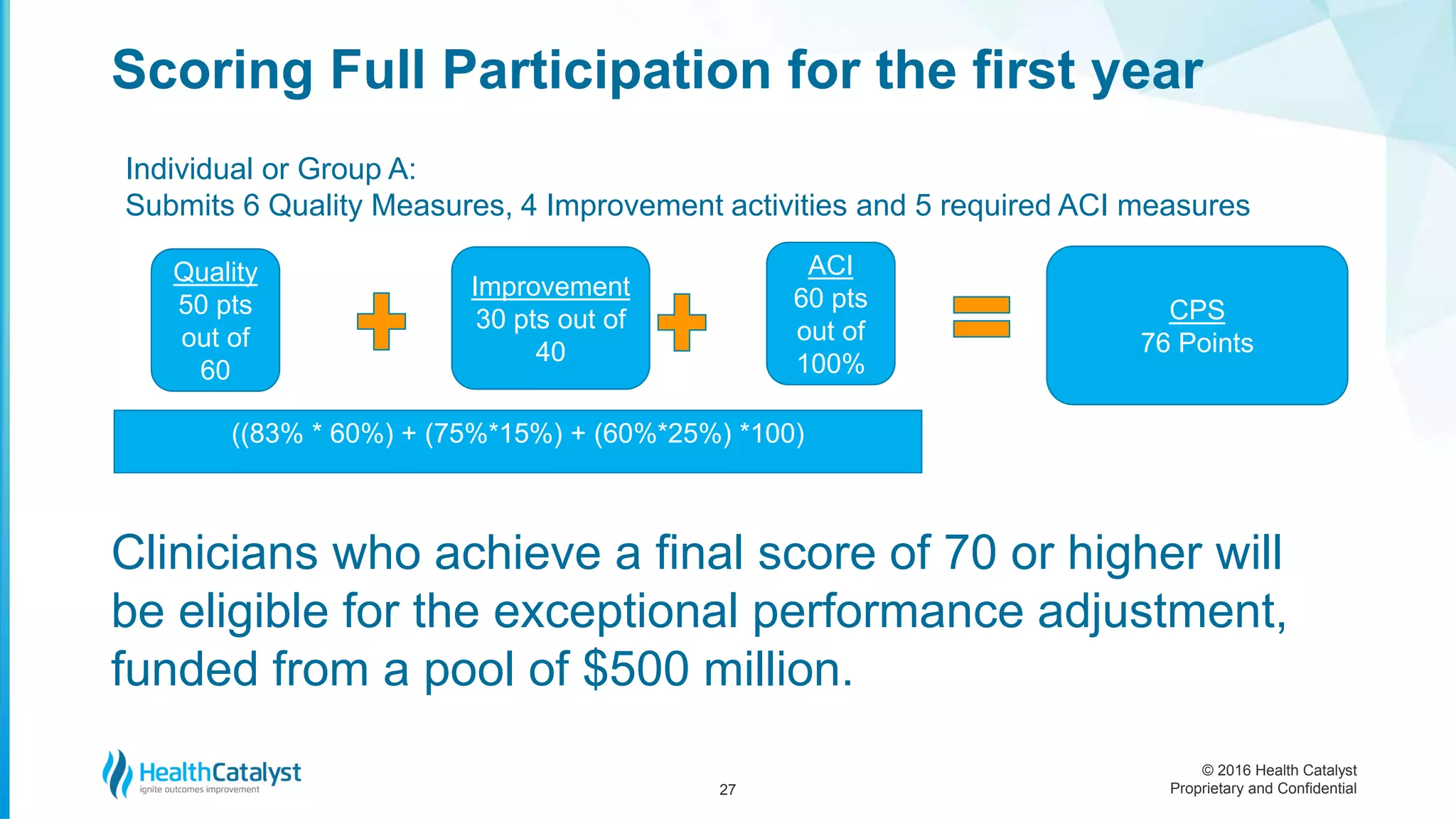
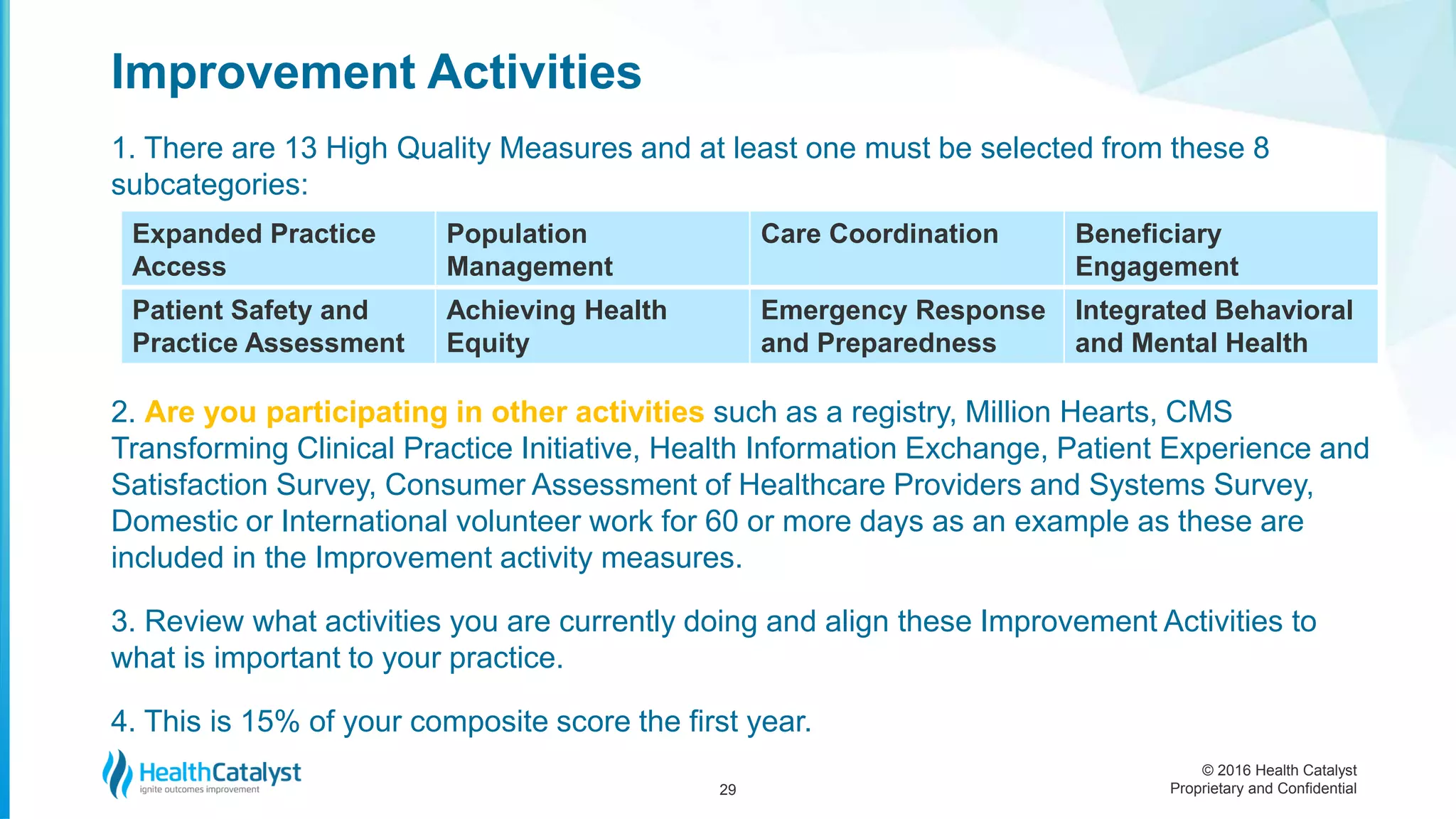
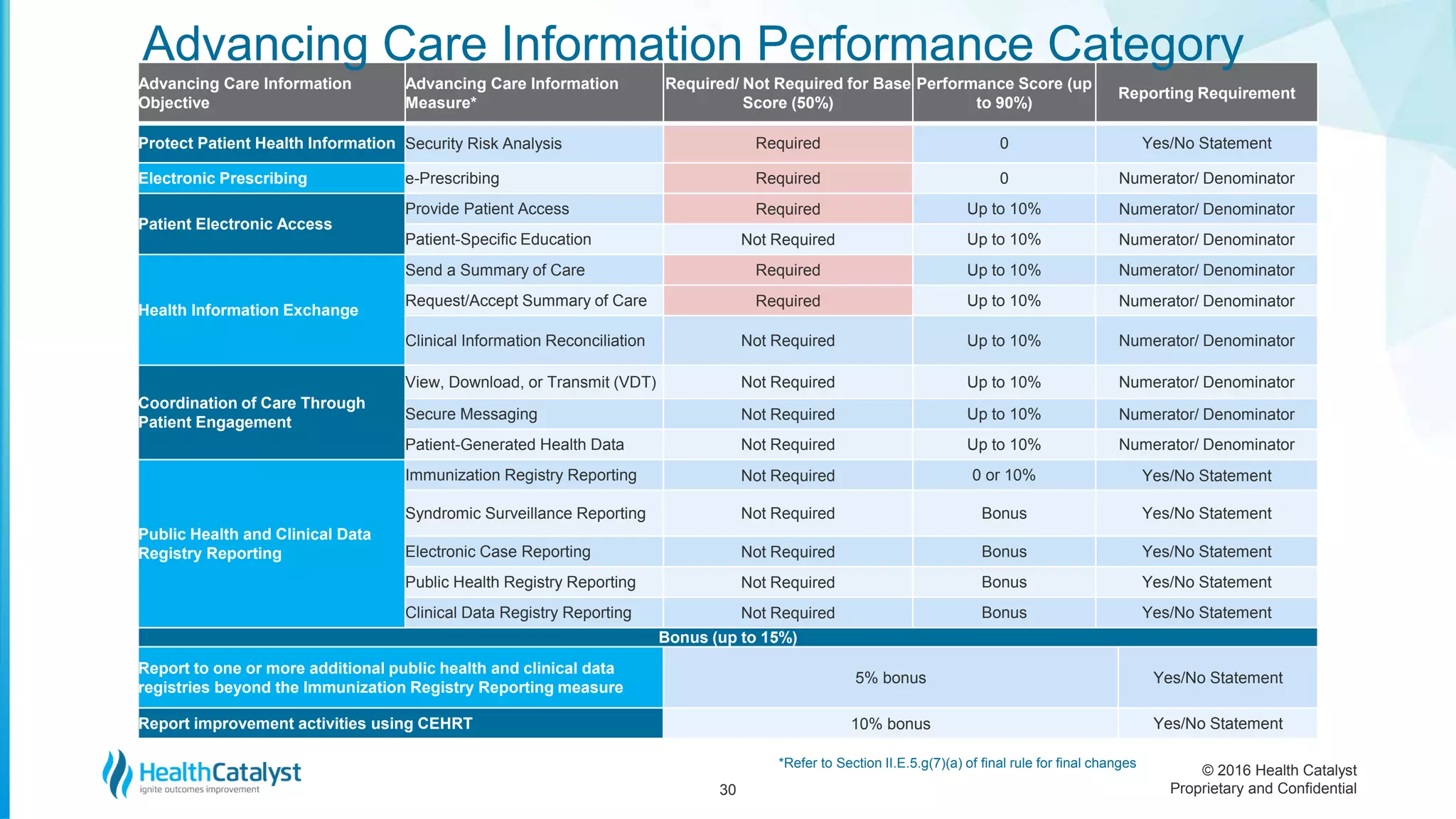
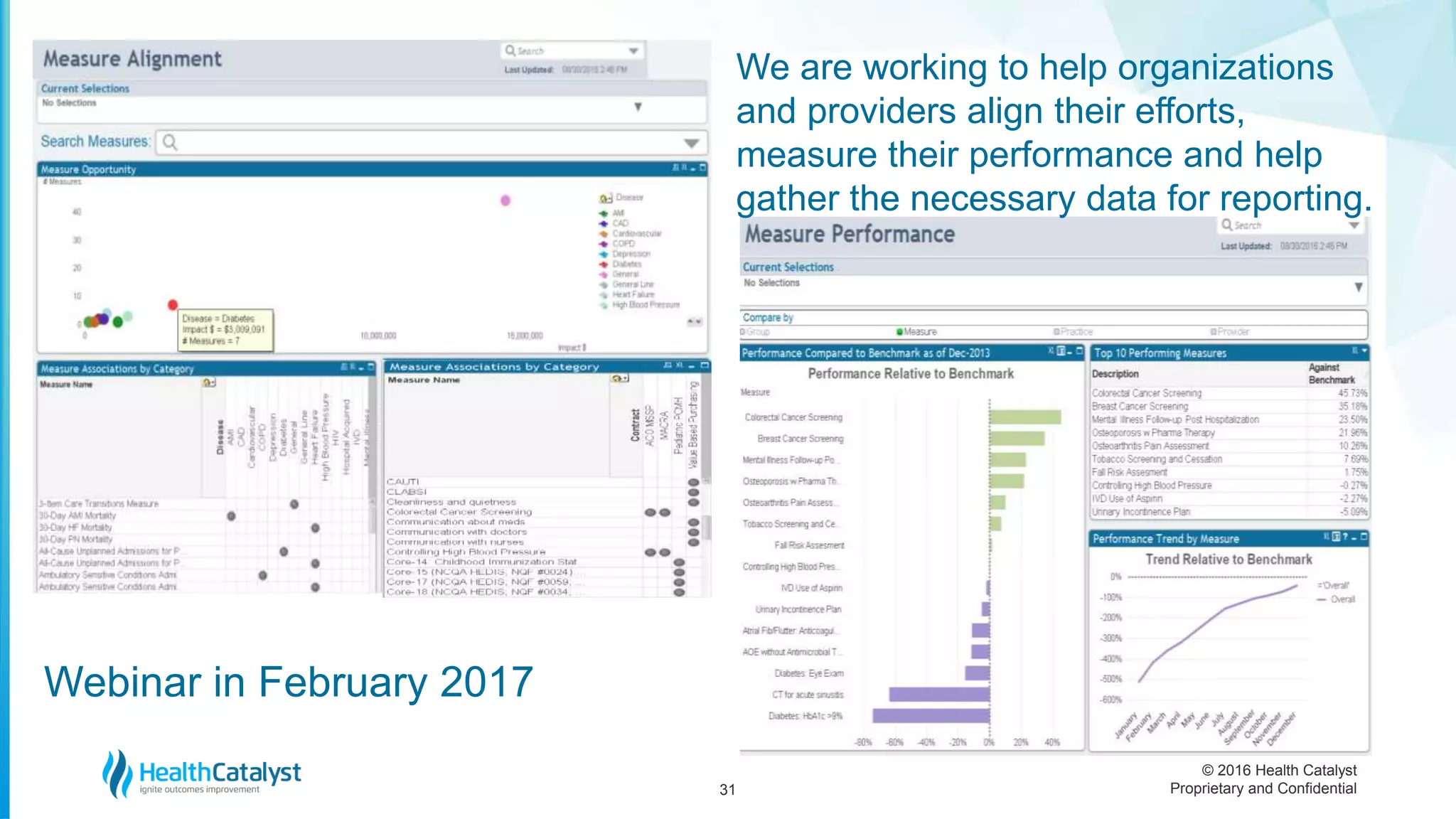
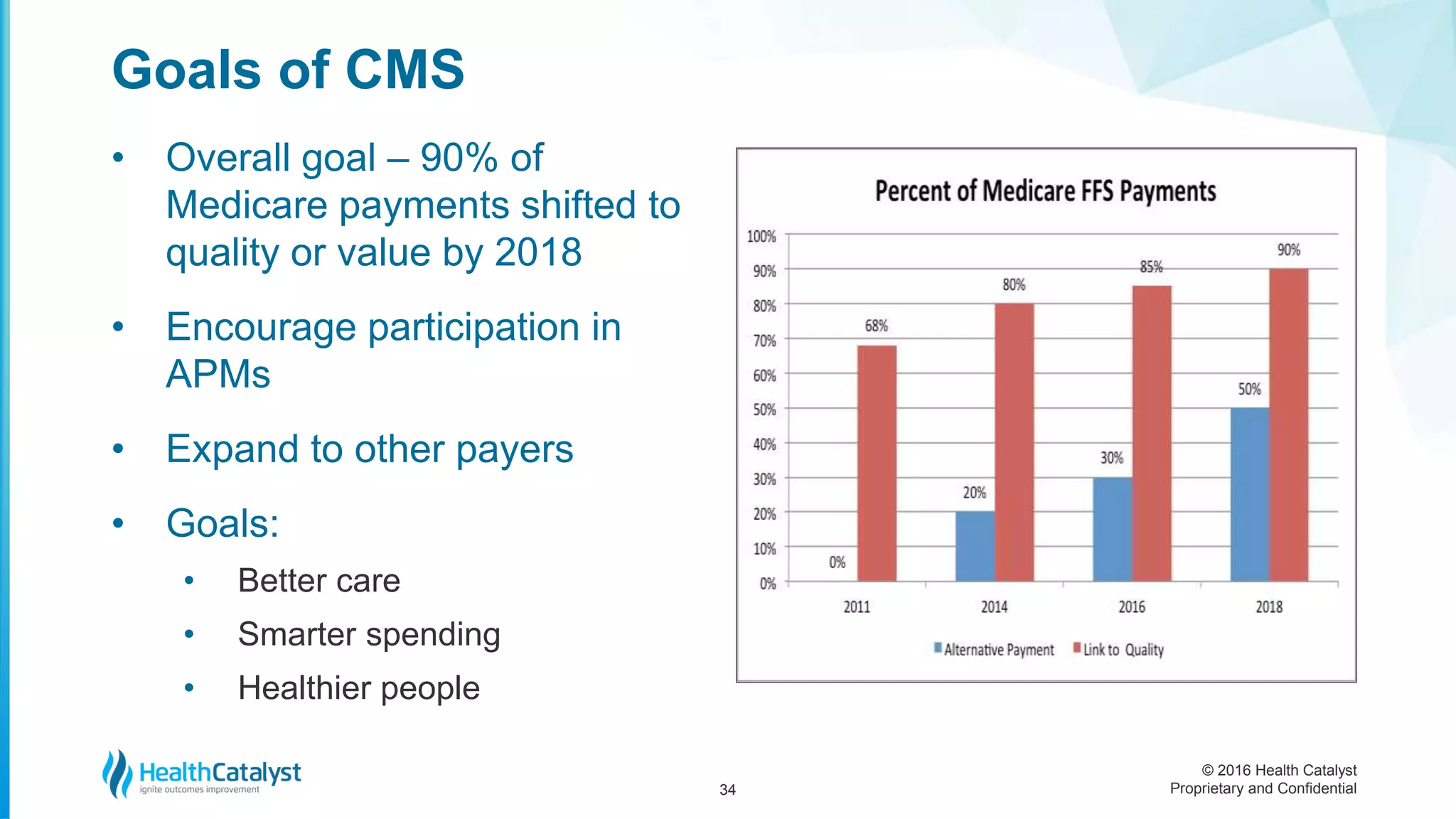
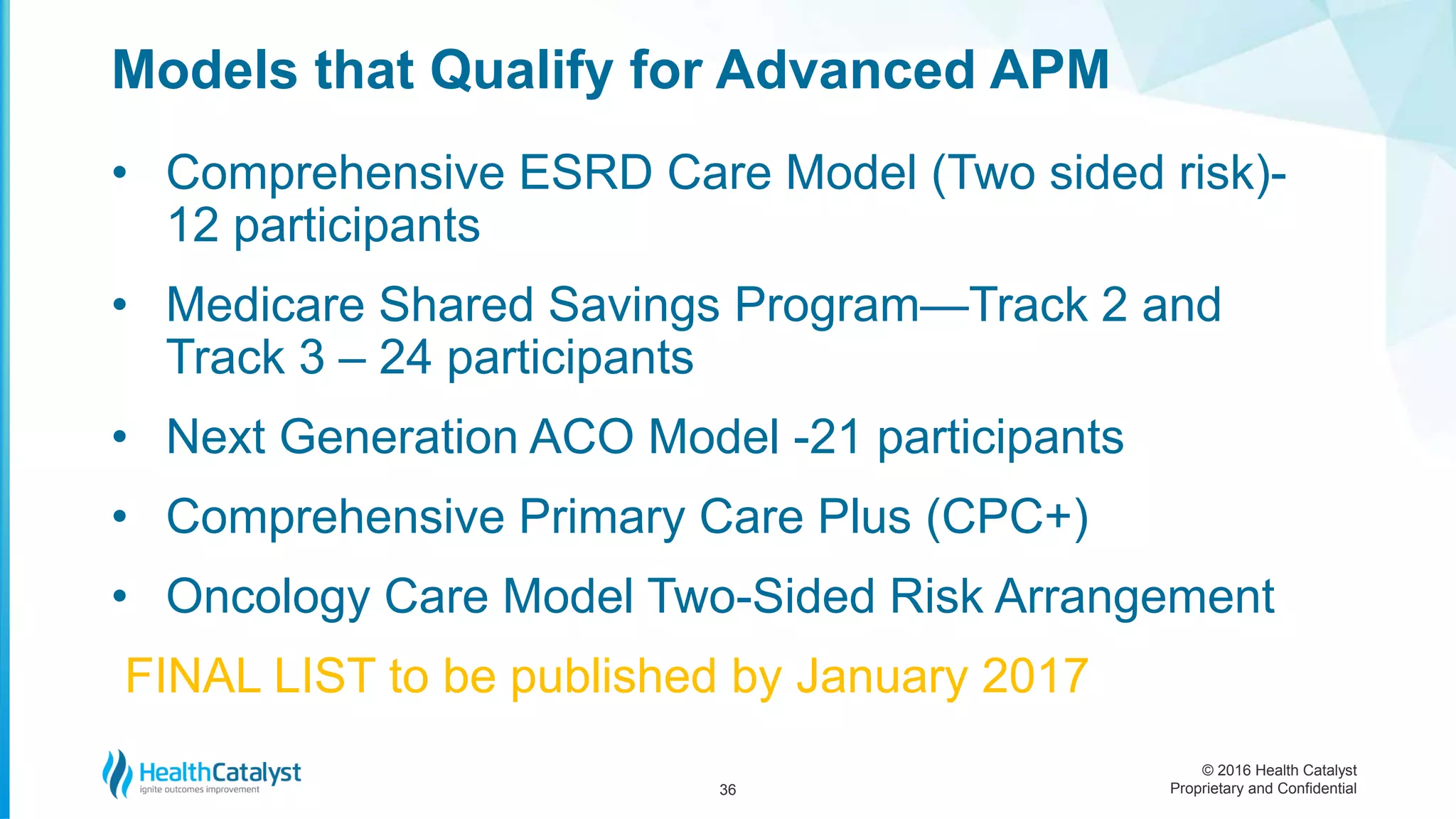
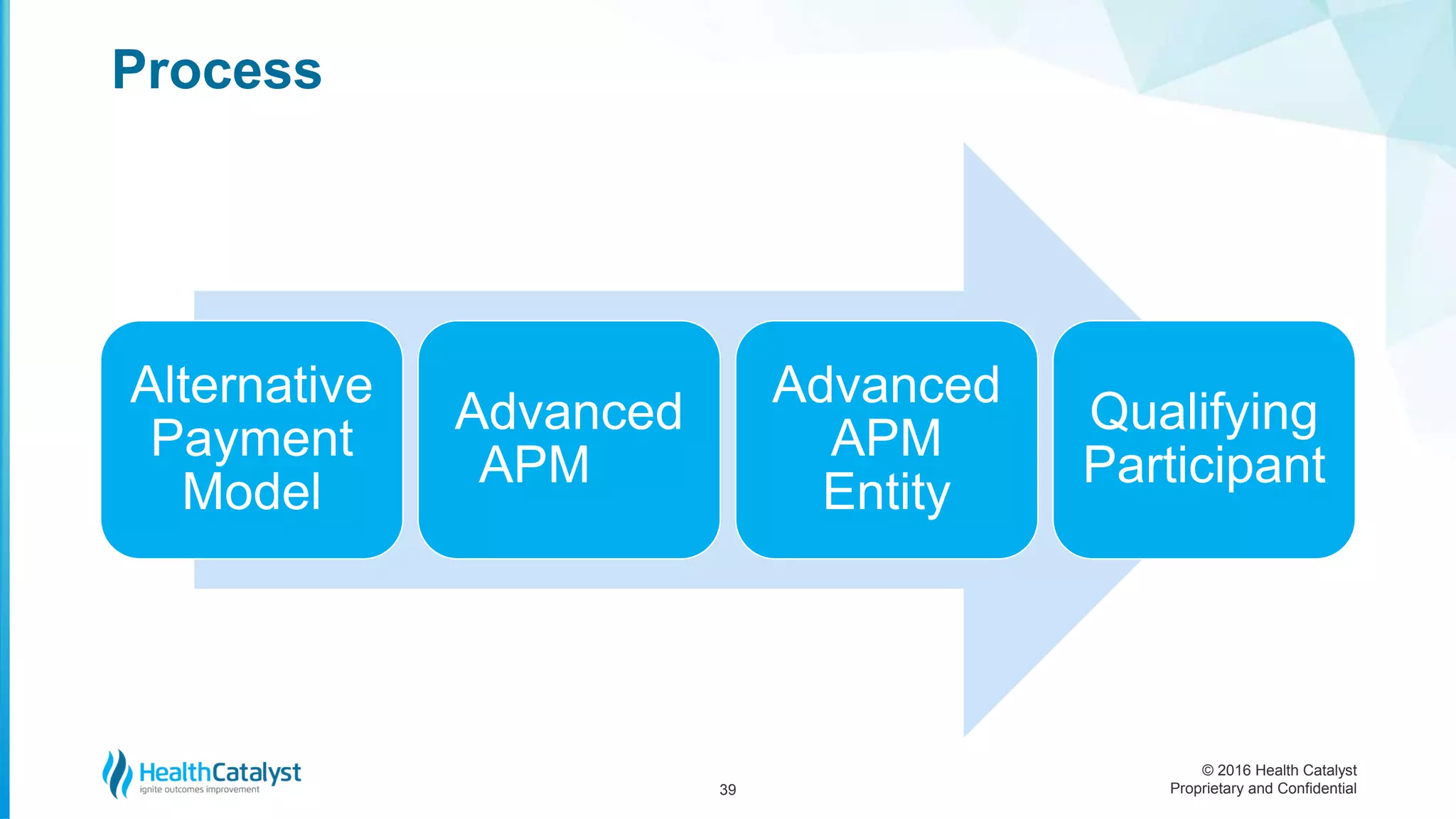
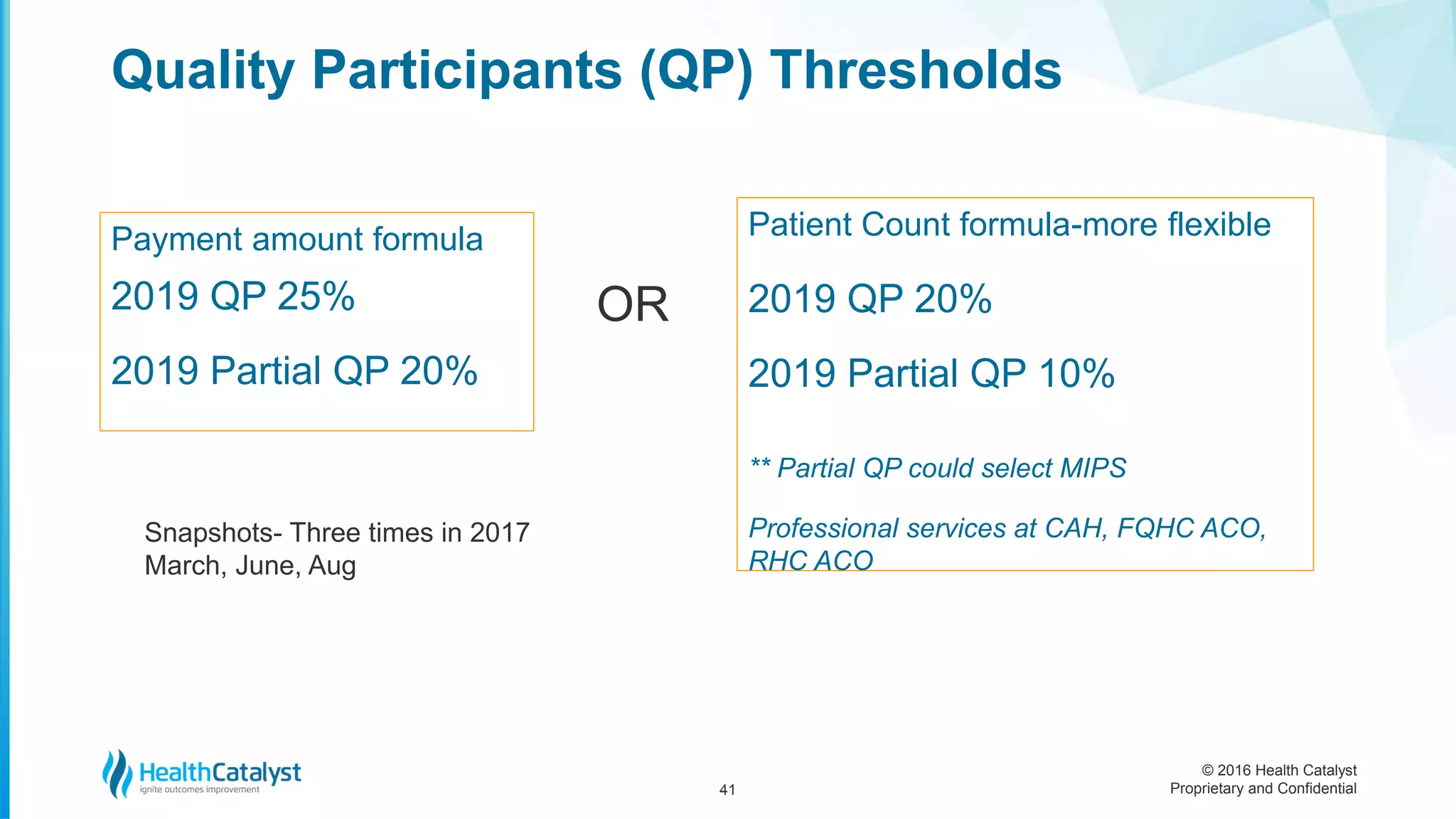
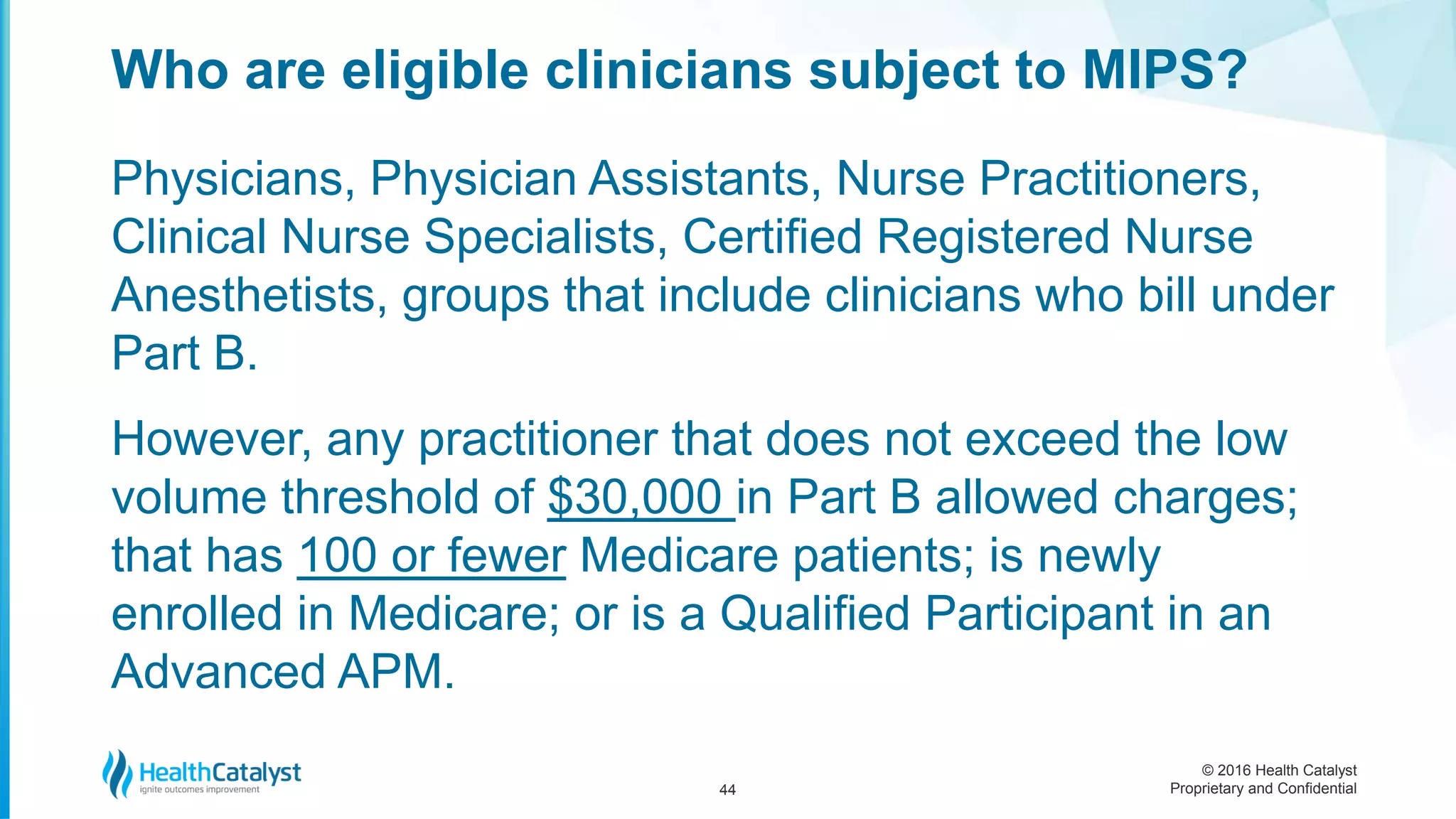
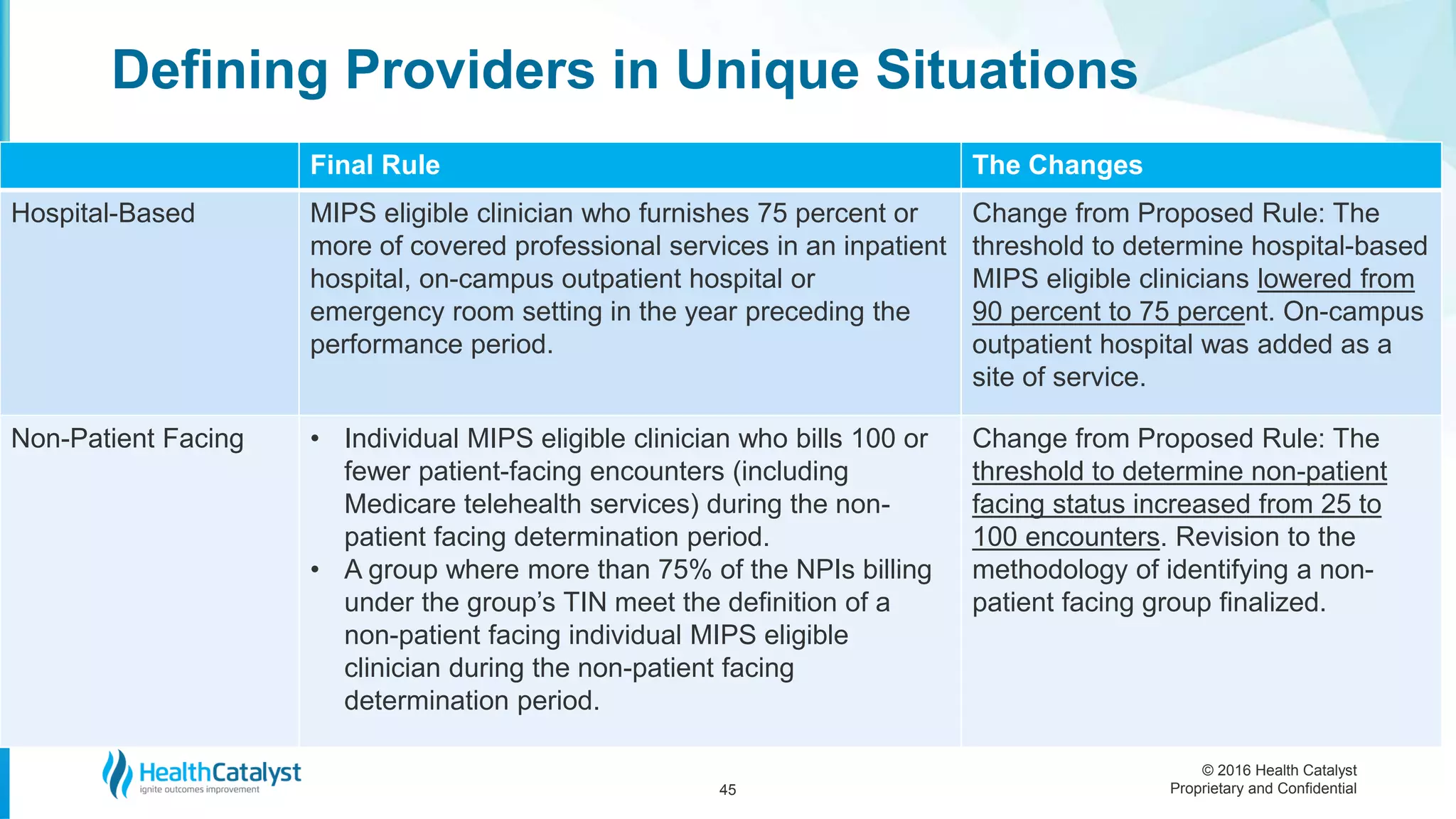
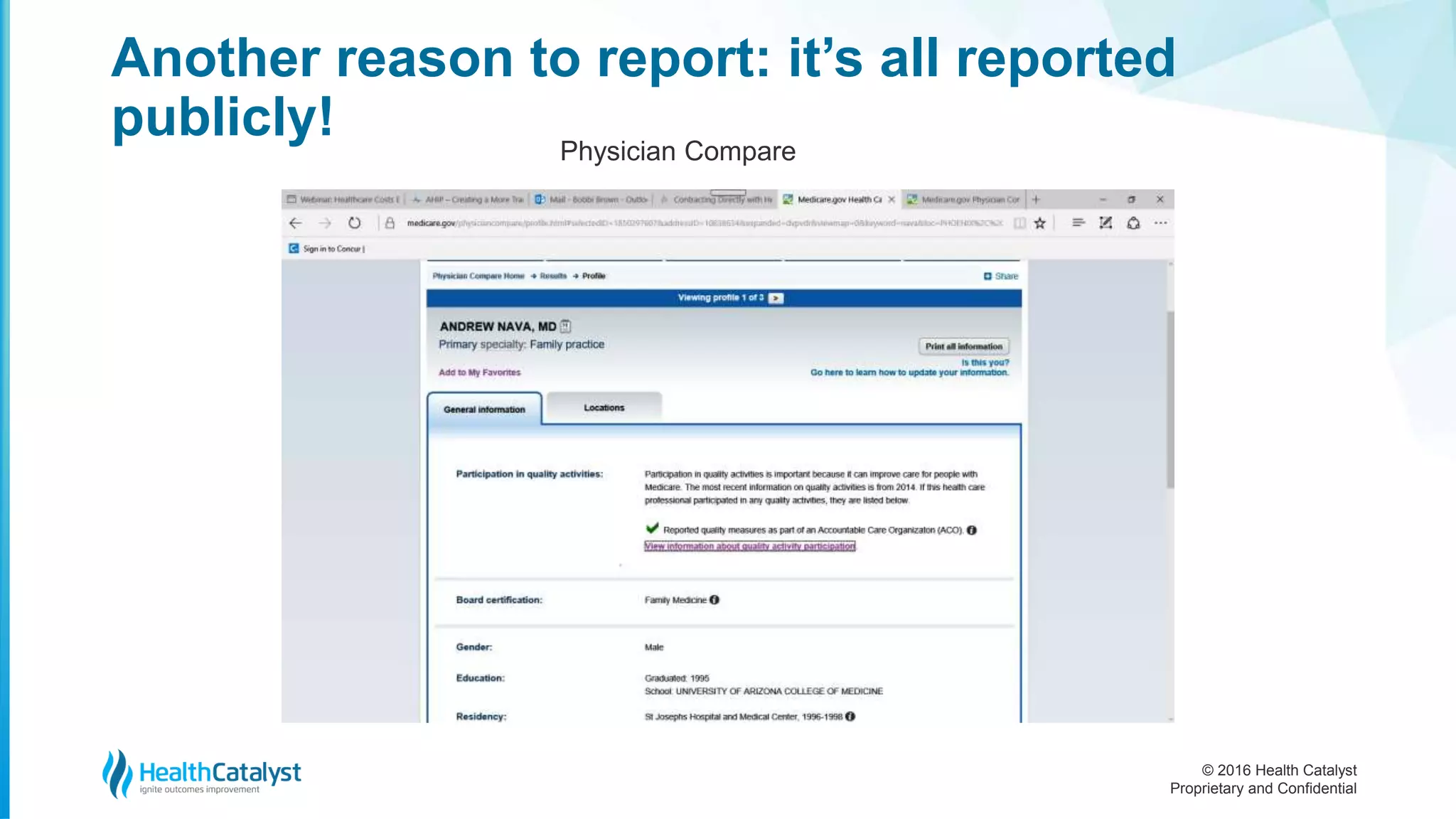
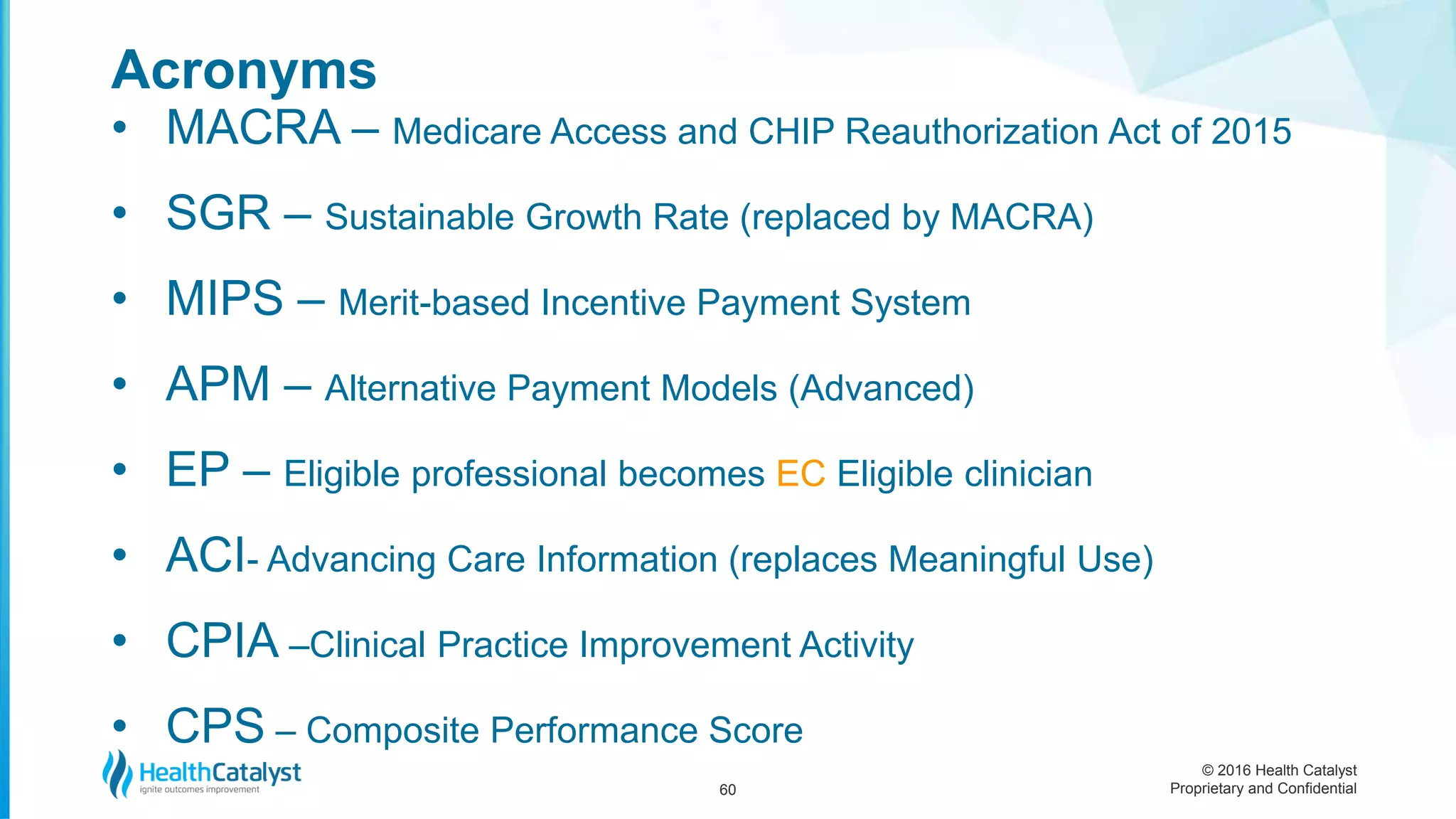
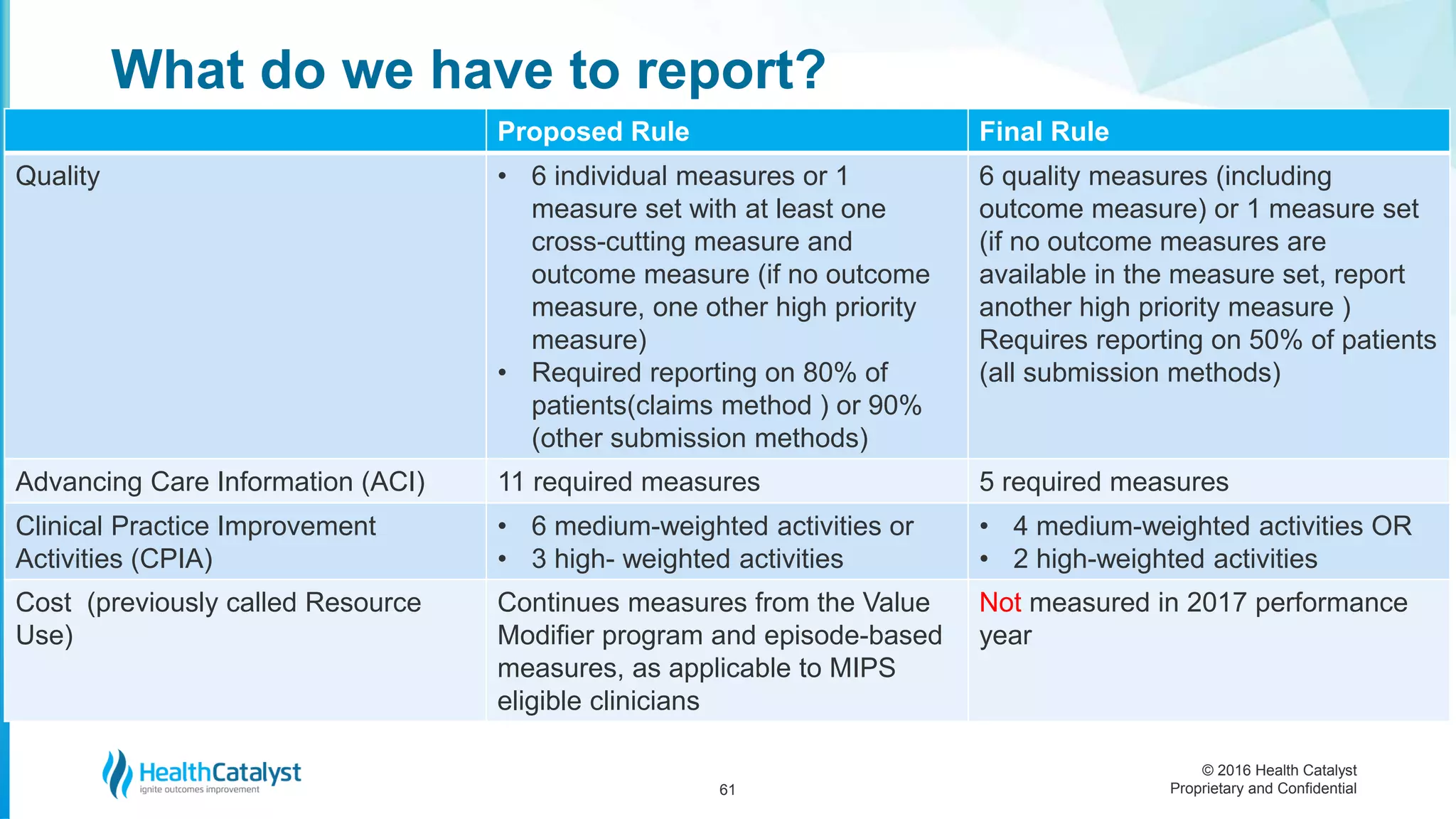
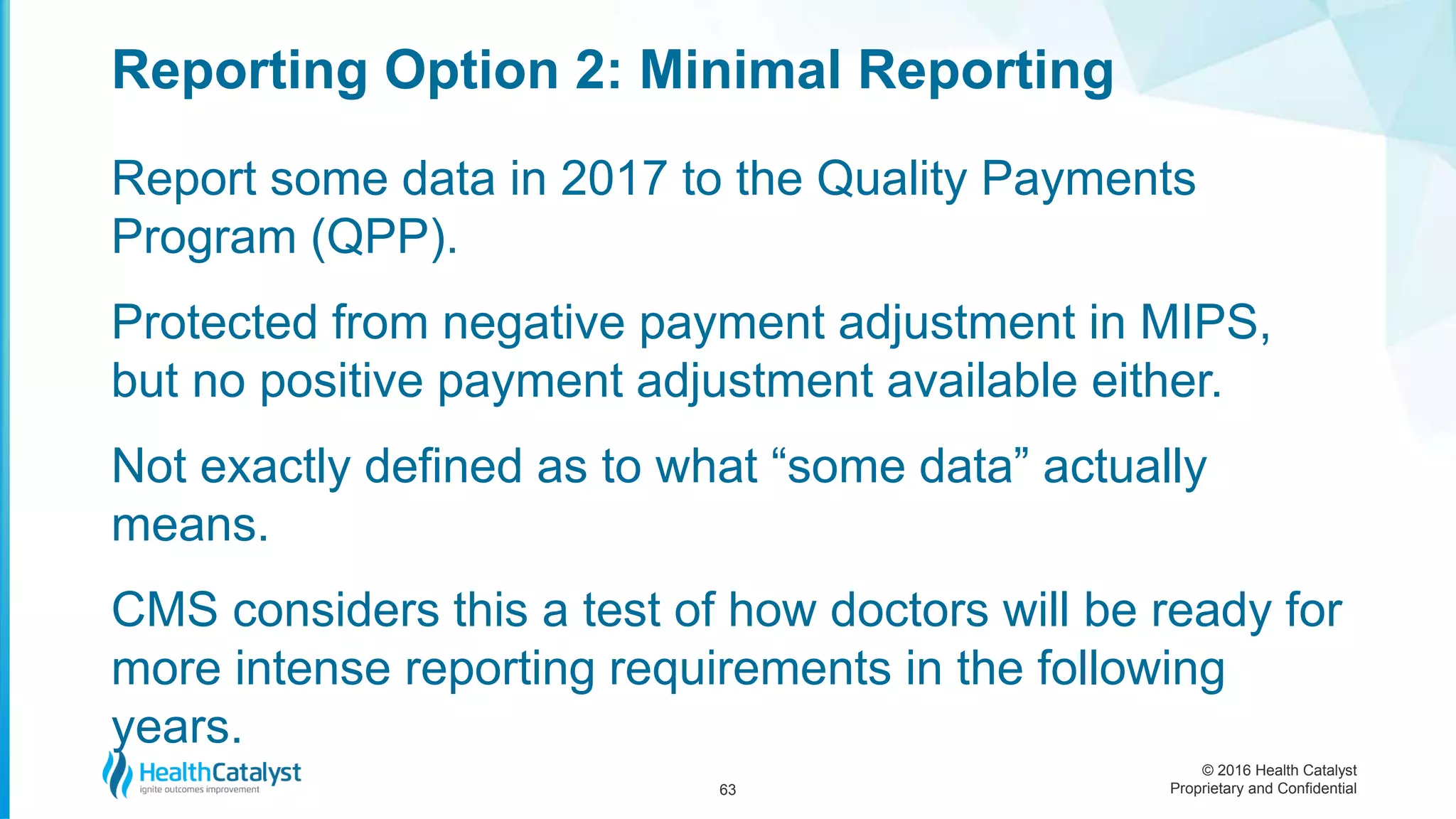
The document addresses the implementation of the MACRA and the new Quality Payment Program, outlining the transition to a performance-based payment system for Medicare doctors. It discusses the goals of improving patient care, reducing provider burden, and incentivizing quality outcomes through new tracks for participation. Key details include timelines for reporting, eligibility criteria, composite performance scoring, and the implications of choosing between Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs).