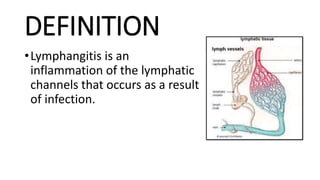
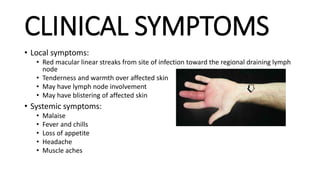
Lymphangitis is an inflammation of the lymphatic channels caused by bacterial infections like streptococci and staphylococcus. Risk factors include diabetes, immunodeficiency, and steroid use. Microorganisms enter through broken skin and travel along lymphatic vessels, causing red streaks. Symptoms are tender red lines spreading from the infection site towards lymph nodes, with fever and aches. Diagnosis is clinical but may include blood tests and imaging. Treatment involves antibiotics, rest, elevation, and incision/drainage of abscesses. Prognosis is good with proper antibiotics but morbidity relates to underlying infection.
Lymphedema is fluid accumulation caused by lymphatic system failure. It can