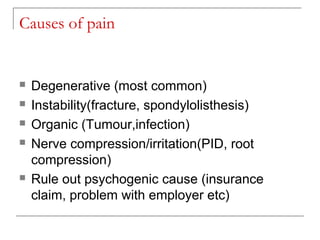
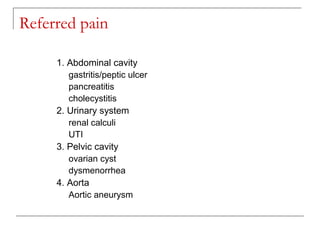
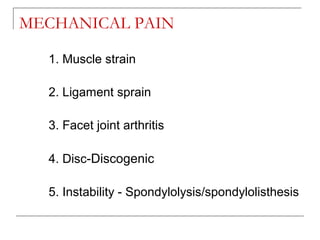
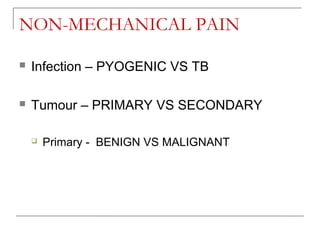
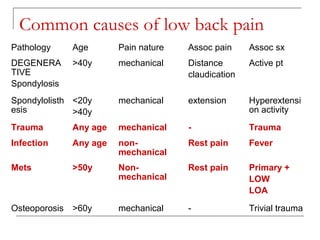
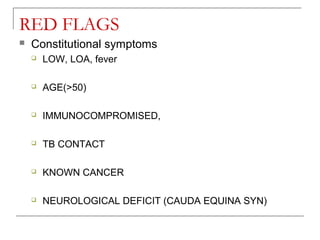
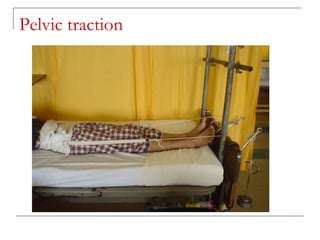
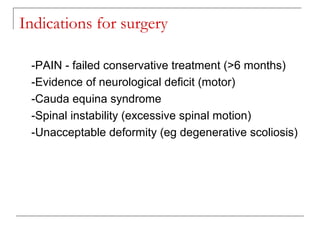
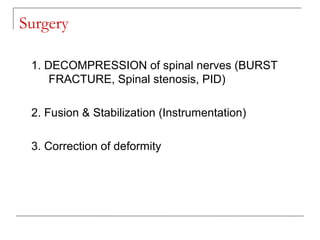
Low back pain is very common, especially among those over age 45. Most cases resolve with conservative treatment within 3 months, while 5-10% may require surgery. The lumbar spine is most prone to degeneration and pain due to its mobility. Common causes of low back pain include degeneration, instability, infection, nerve compression, and psychological factors. Pain can be mechanical, non-mechanical, referred, or radicular in nature. Conservative treatments include rest, physiotherapy, medication, and injections while surgery is indicated for cases of neurological deficit, instability, or unacceptable deformity.