The document discusses adaptive immunity. It describes:
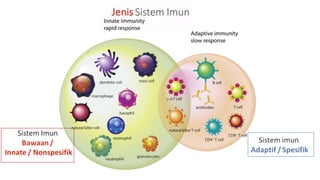
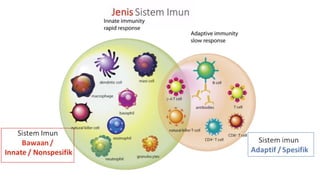
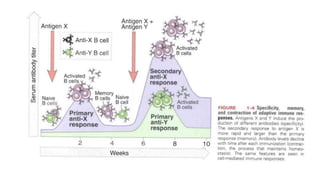
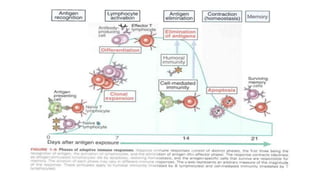
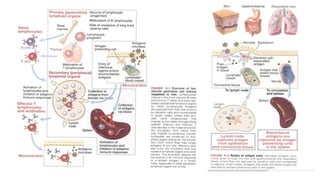
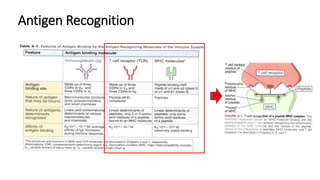
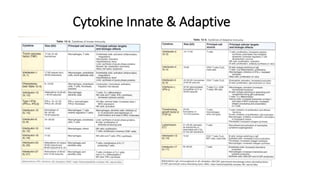
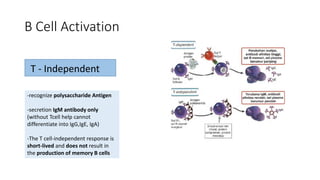
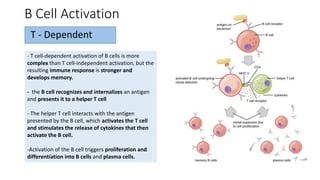
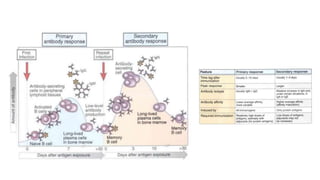
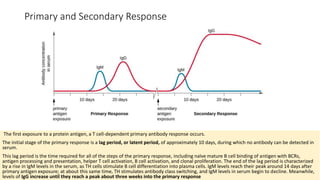
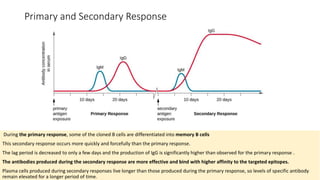
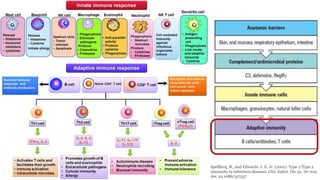
1. Adaptive immunity is stimulated by exposure to infectious agents and increases in magnitude and defensive capabilities with each successive exposure. It can recognize and react to a large number of substances.
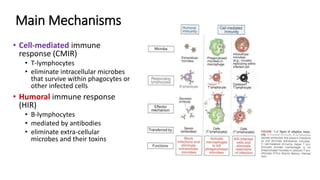
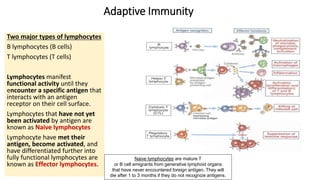
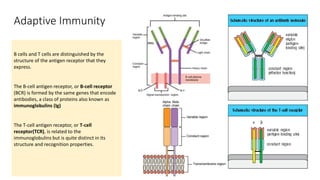
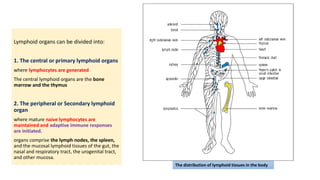
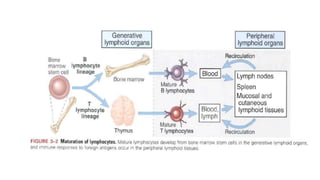
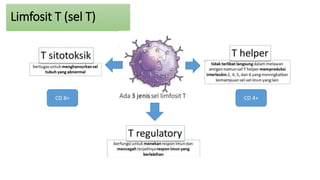
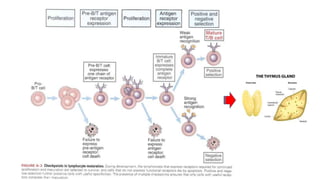
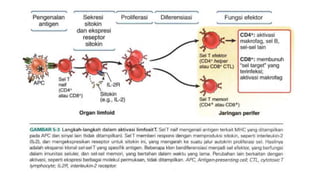
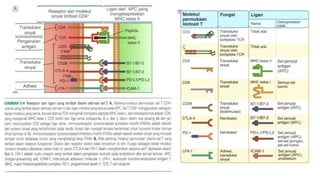
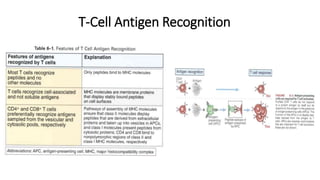
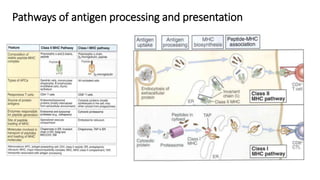
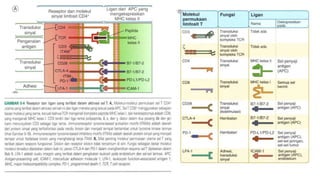
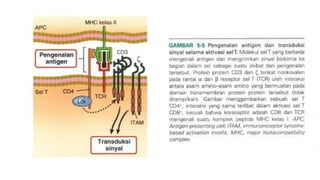
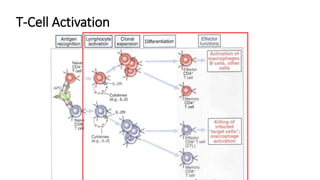
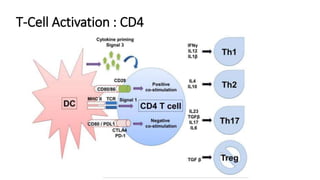
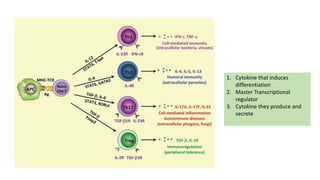
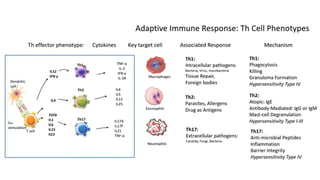
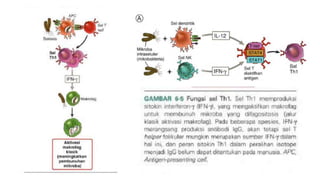
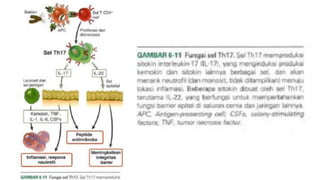
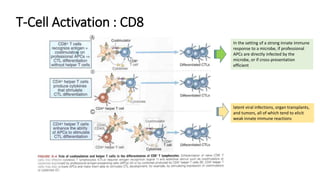
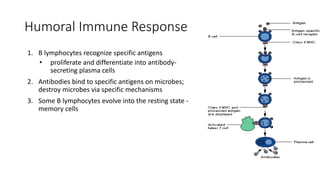
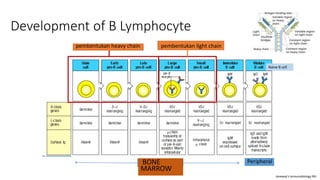
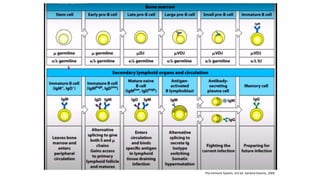
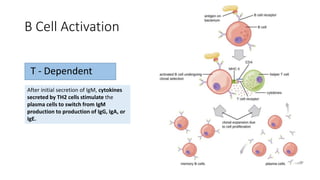
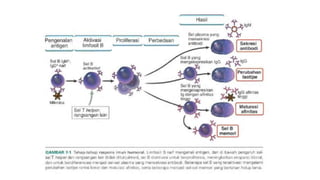
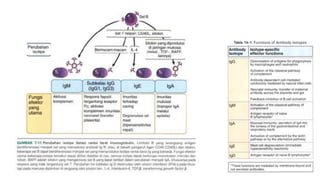
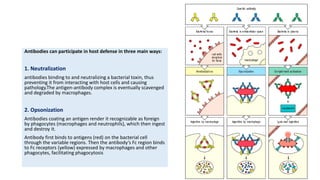
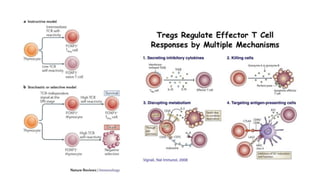
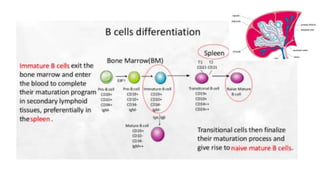
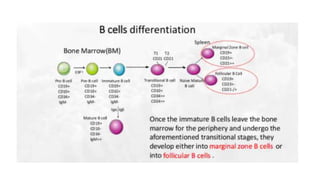
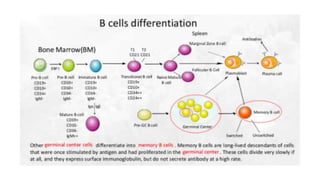
2. The two major types of lymphocytes involved in adaptive immunity are B lymphocytes (B cells) and T lymphocytes (T cells). B cells produce antibodies while T cells mediate cell-mediated immune responses.
3. Adaptive immunity provides the body with immunological memory, allowing faster and stronger responses upon second or subsequent exposures to the same pathogens.