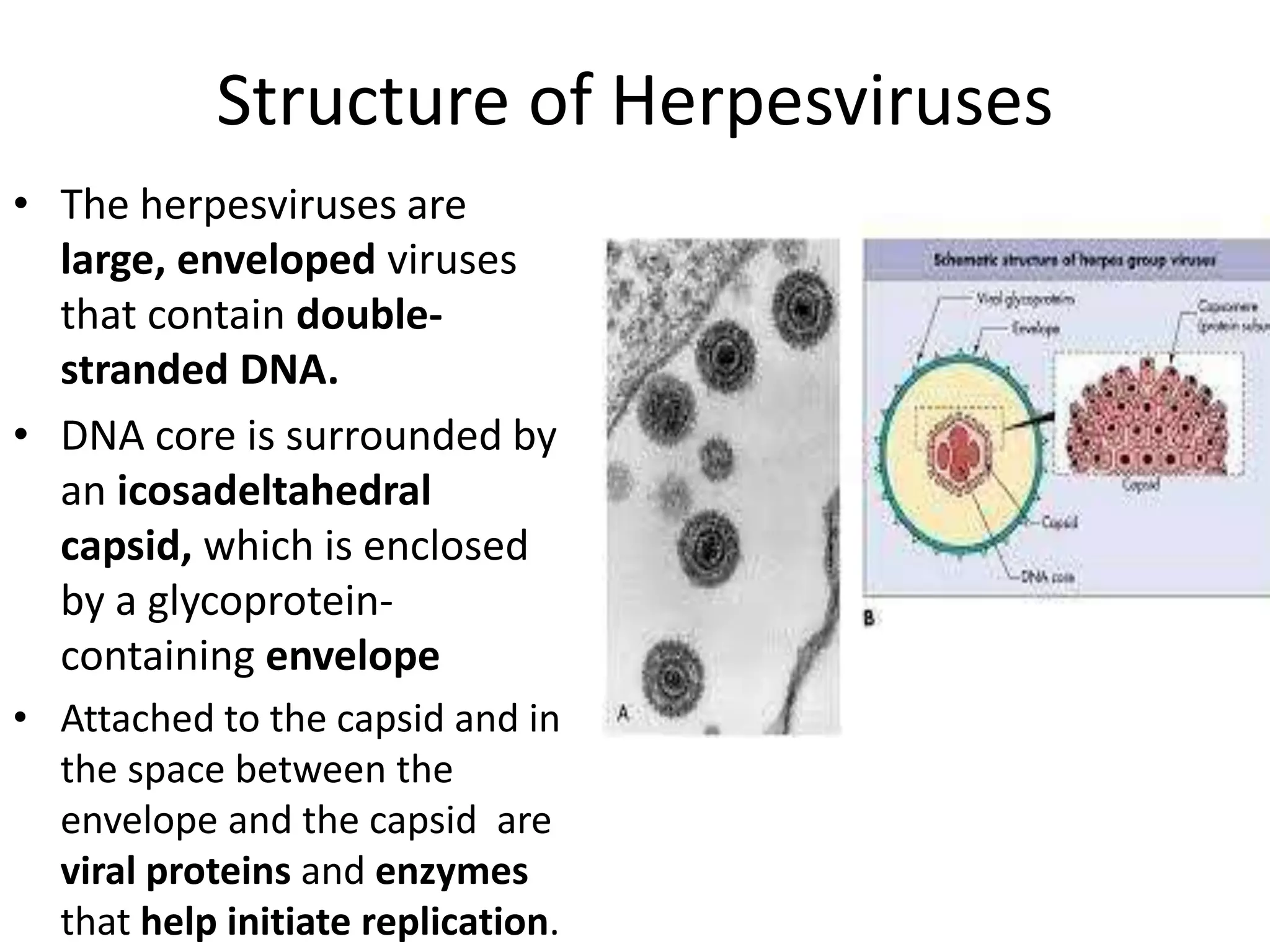
This document discusses several human herpesviruses:
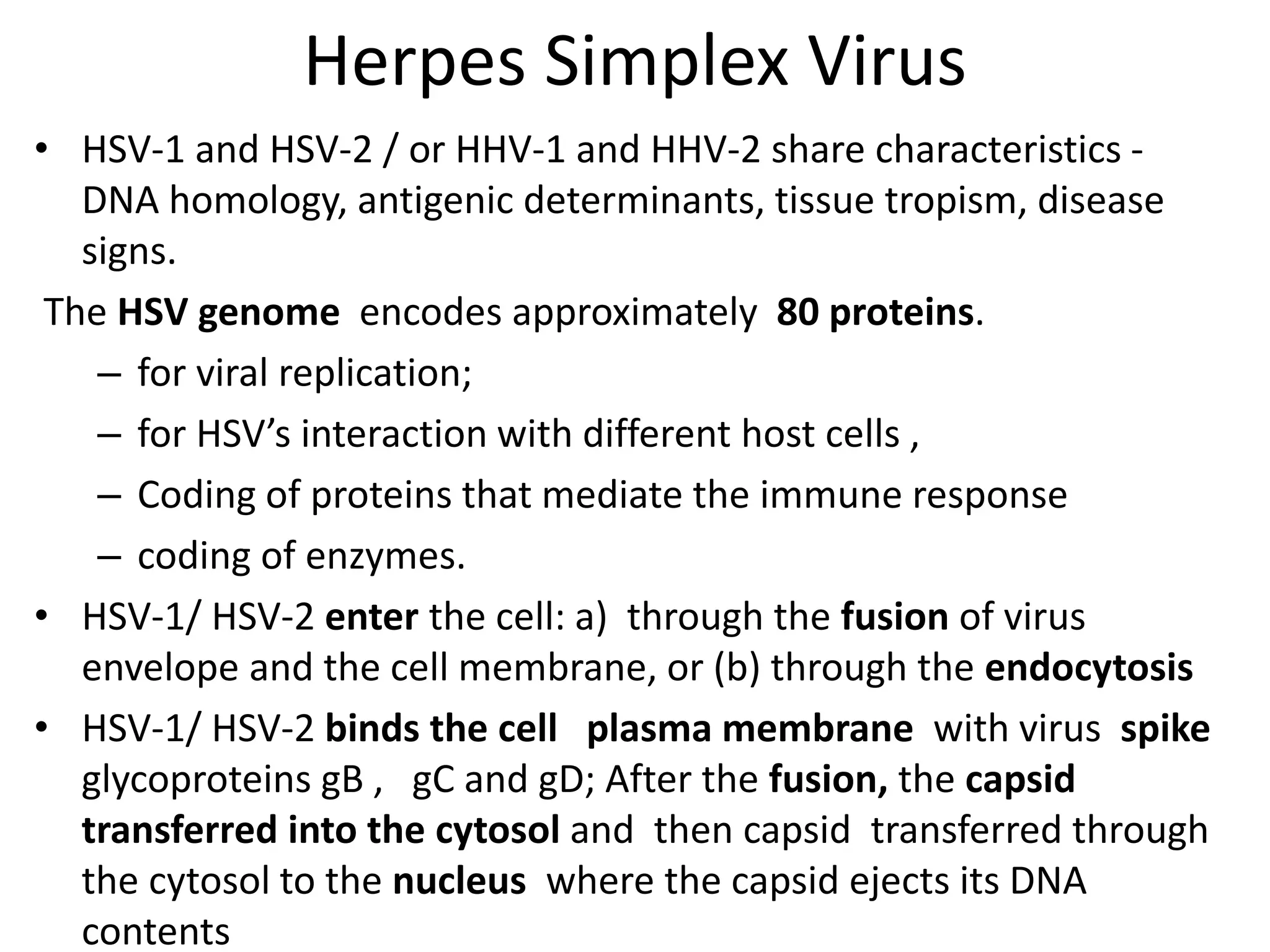
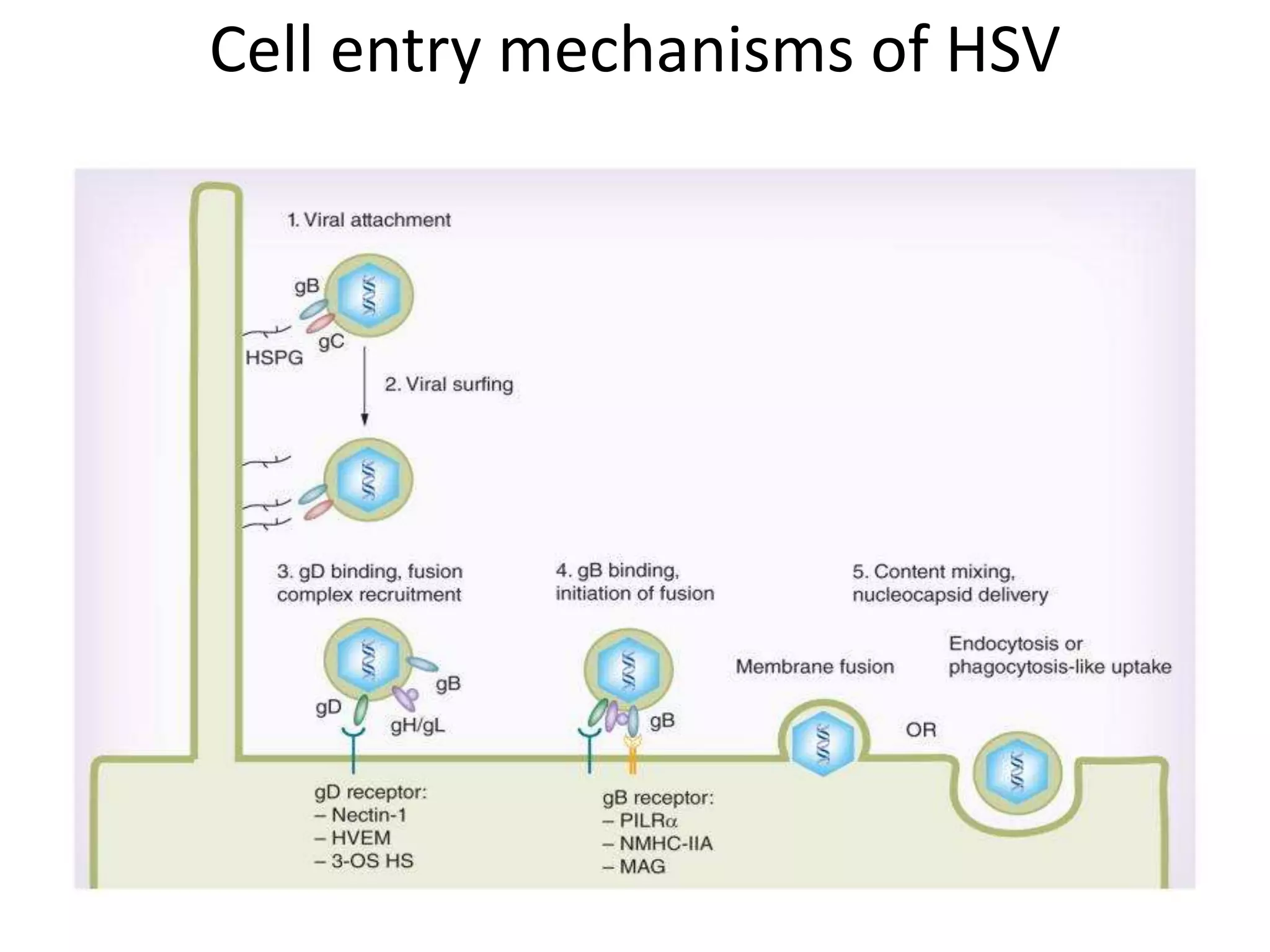
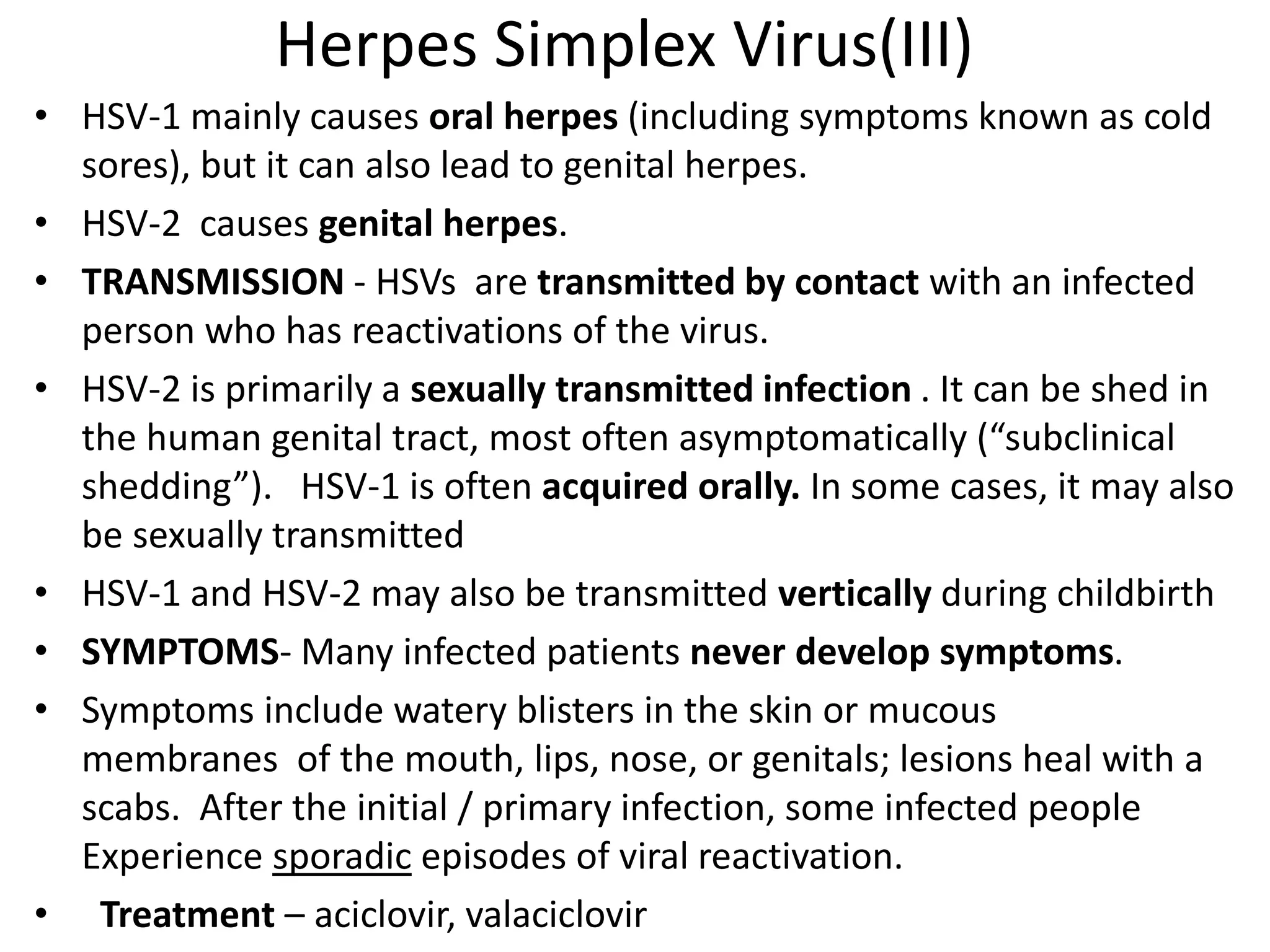
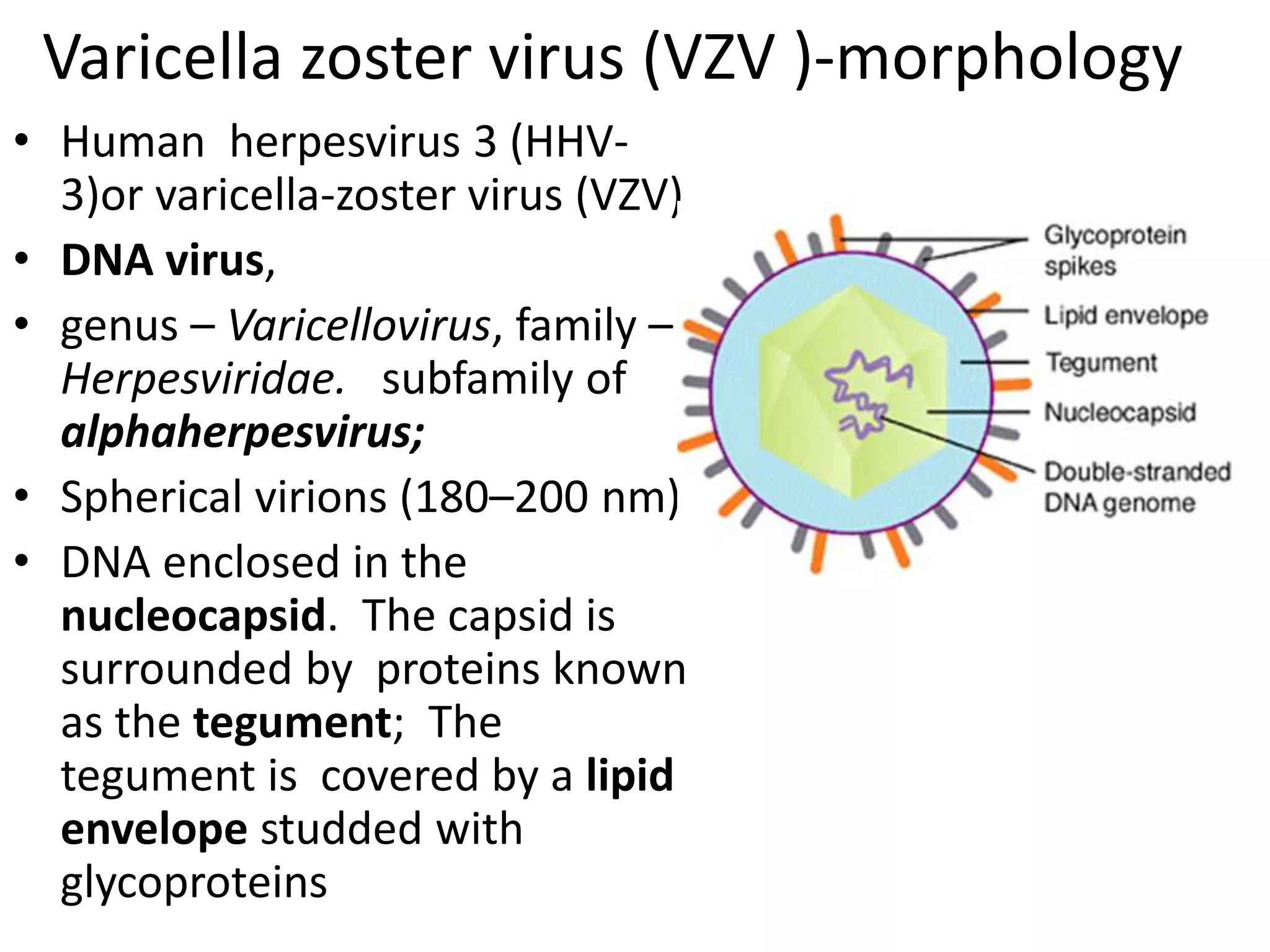
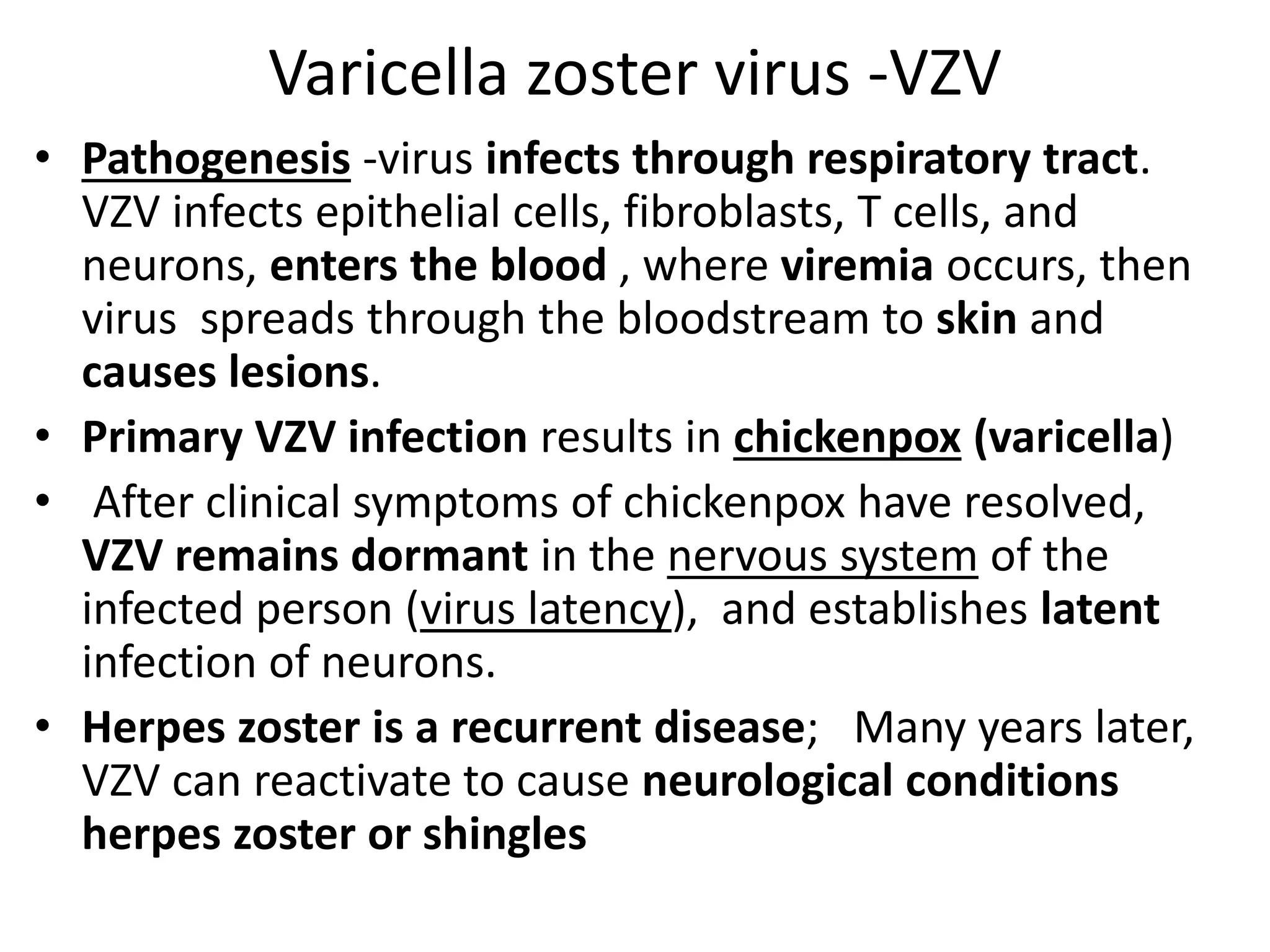
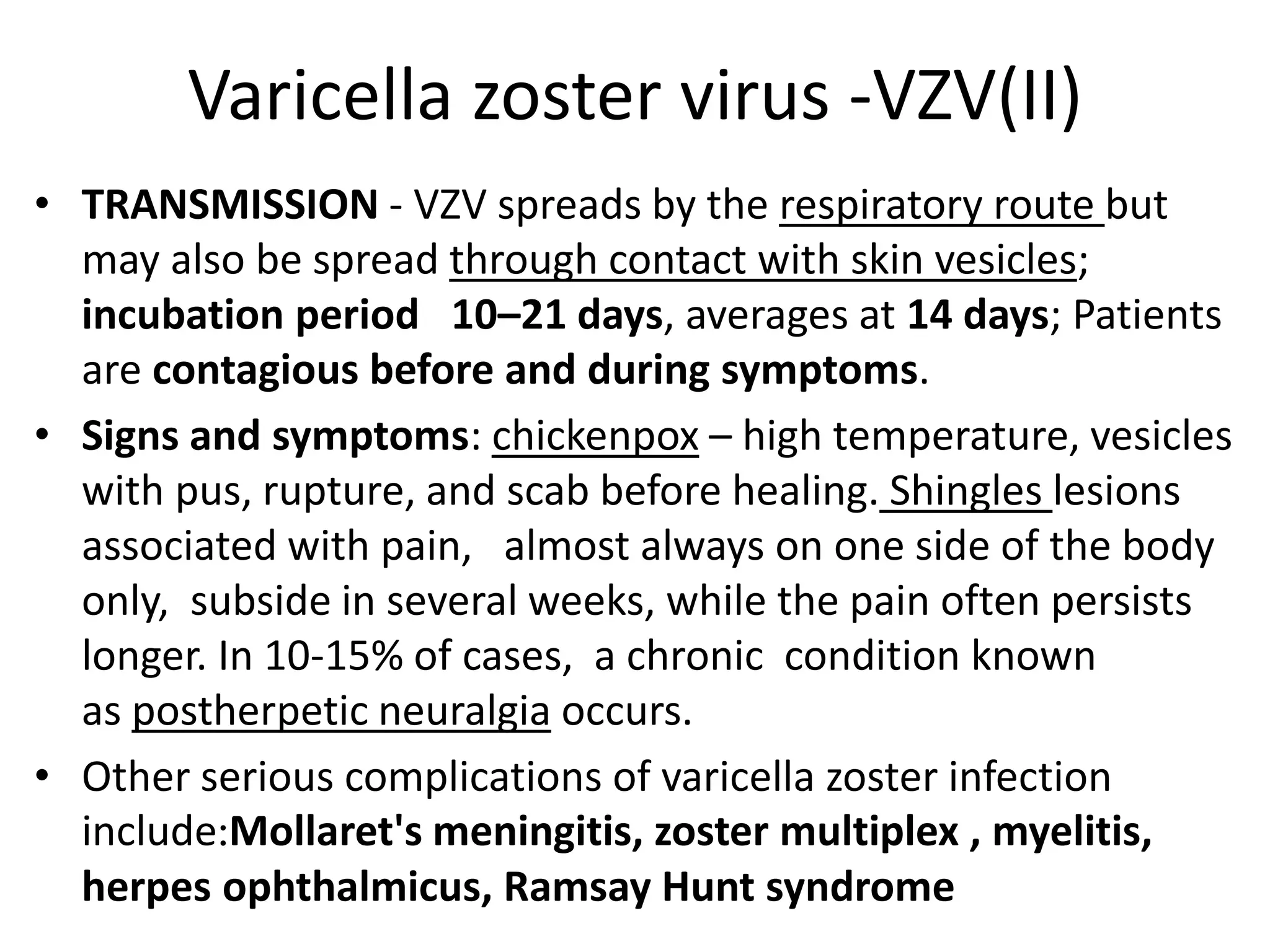
- Herpes simplex viruses 1 and 2 cause oral and genital herpes. Varicella zoster virus causes chickenpox and shingles.
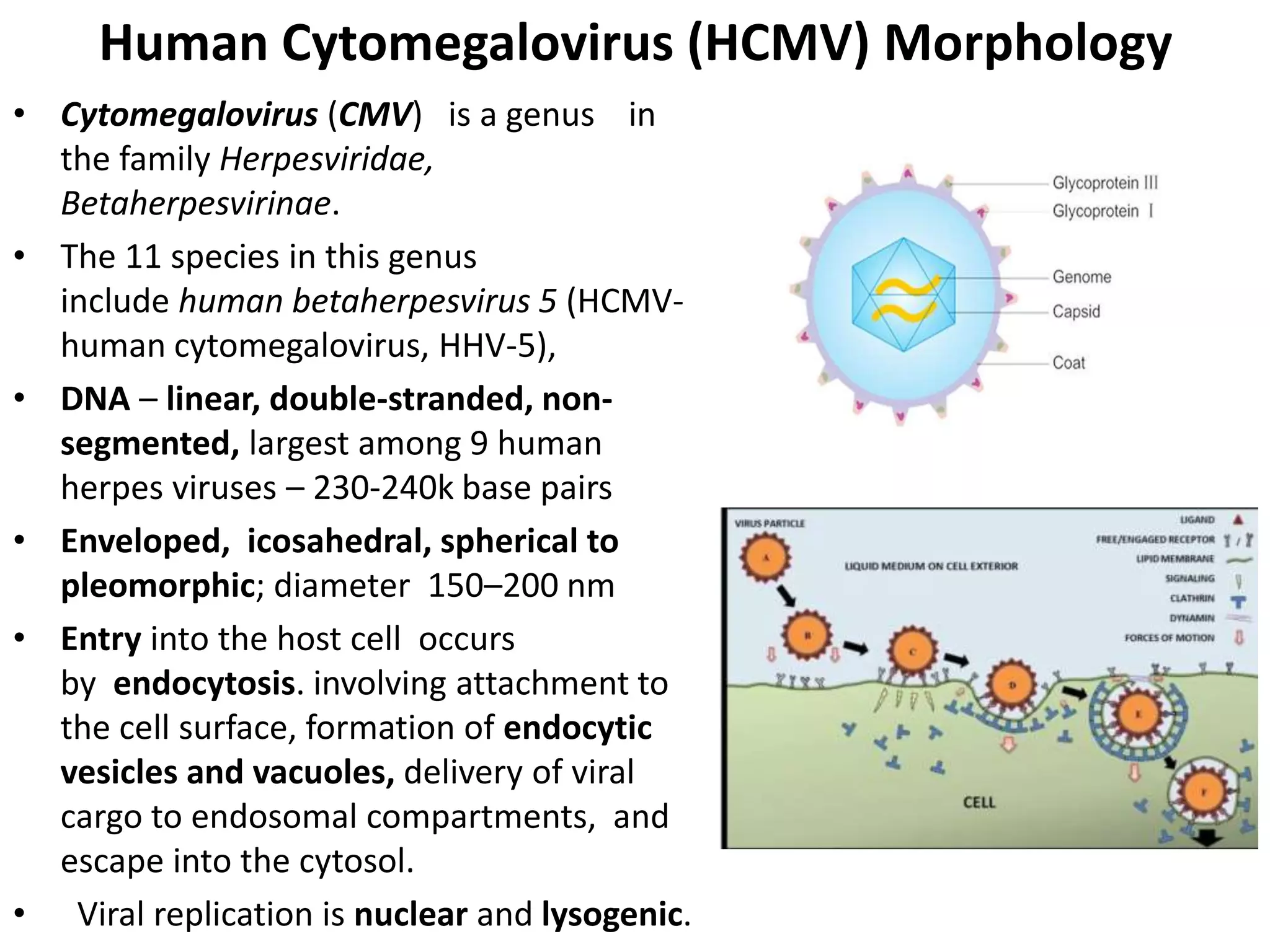
- Cytomegalovirus commonly infects people without symptoms but can cause disease in immunosuppressed individuals. It is a major cause of birth defects.
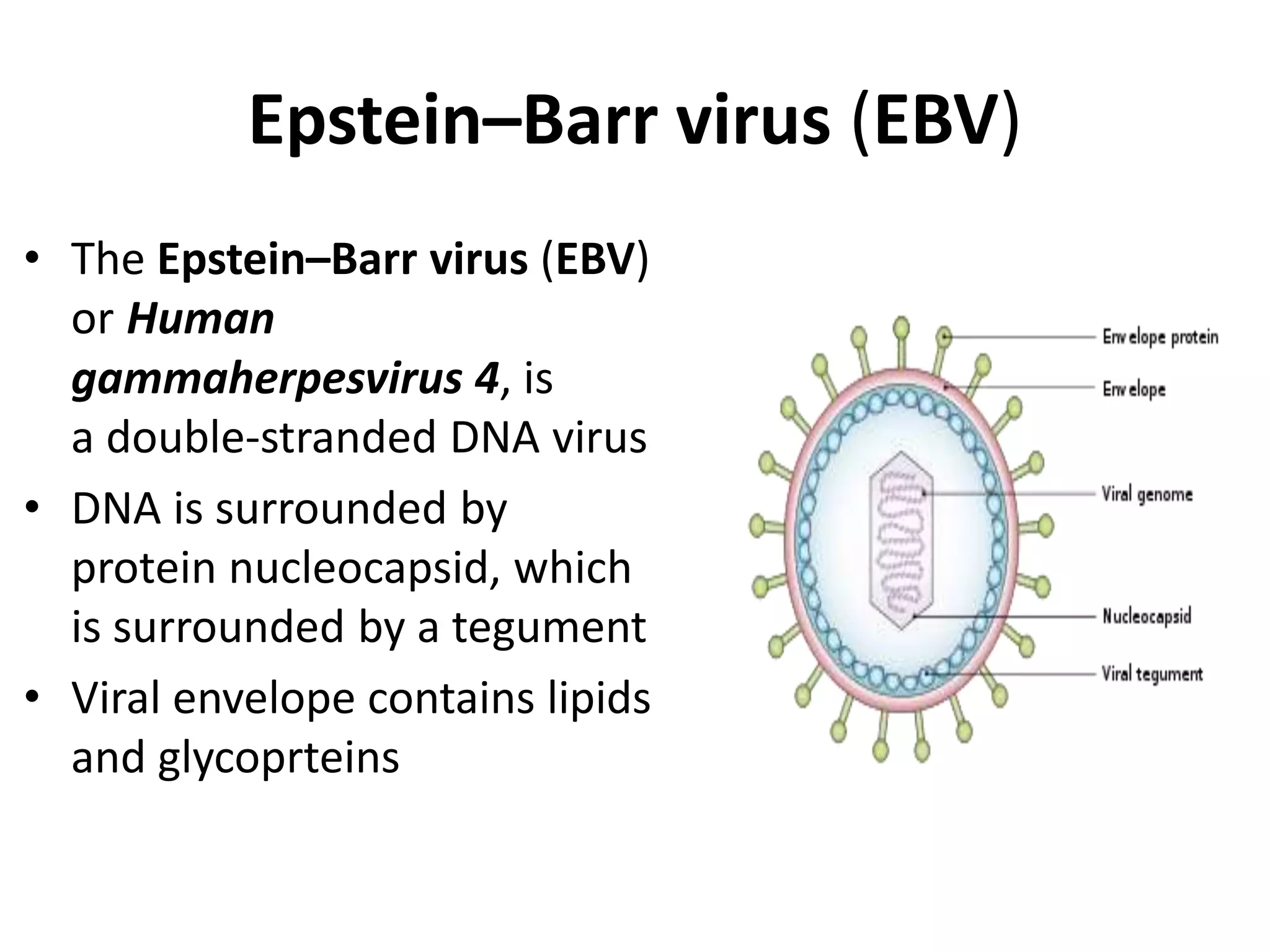
- Epstein-Barr virus causes infectious mononucleosis and has been linked to cancers. It is commonly spread through saliva.
- Herpes B virus in monkeys can cause severe encephalitis in humans through bites or scratches and requires protective equipment to prevent transmission.