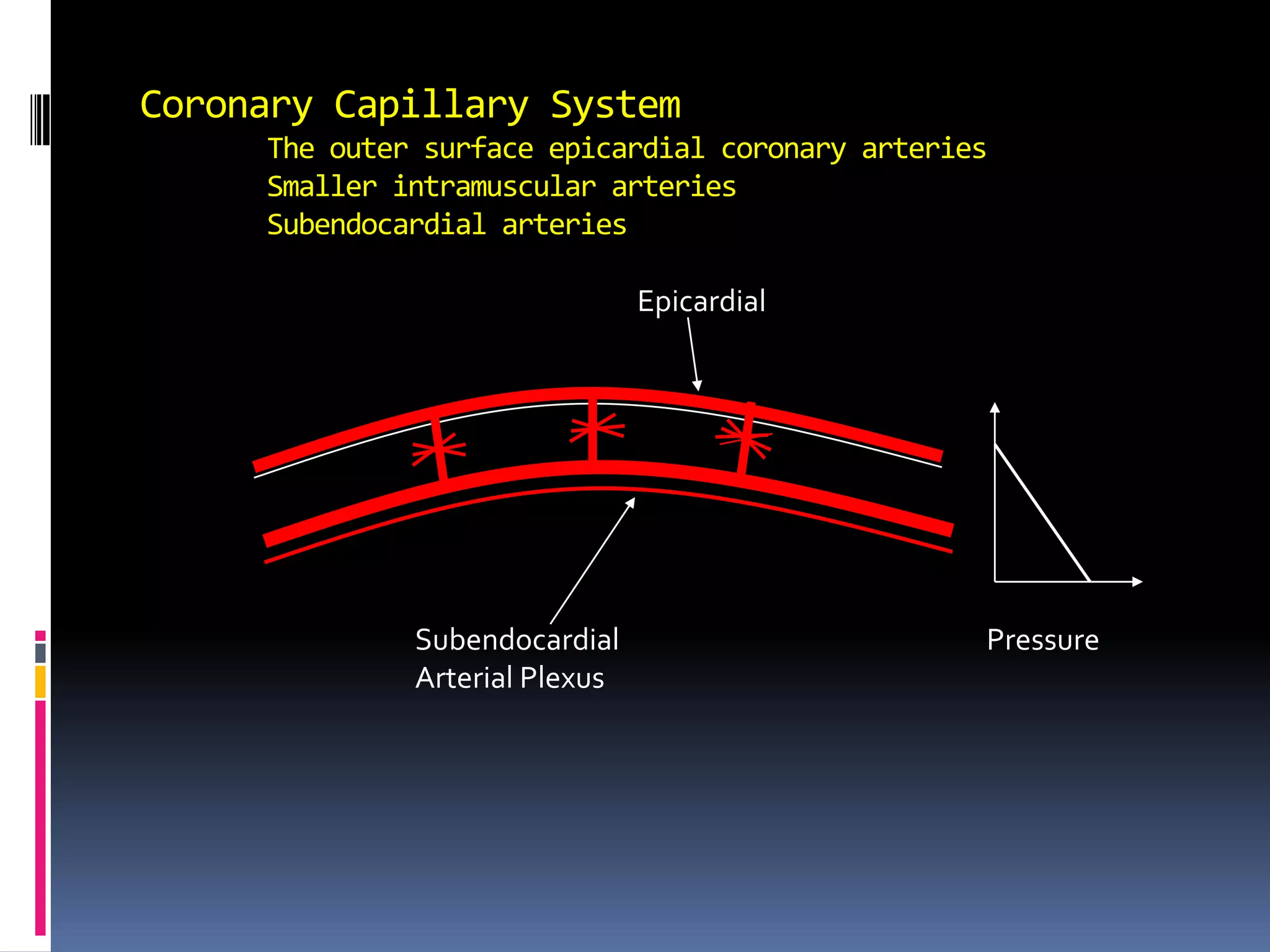
1. Coronary blood flow is regulated locally by the heart muscle in response to metabolic demand and oxygen needs. When the heart works harder, blood flow increases to supply more oxygen and nutrients.
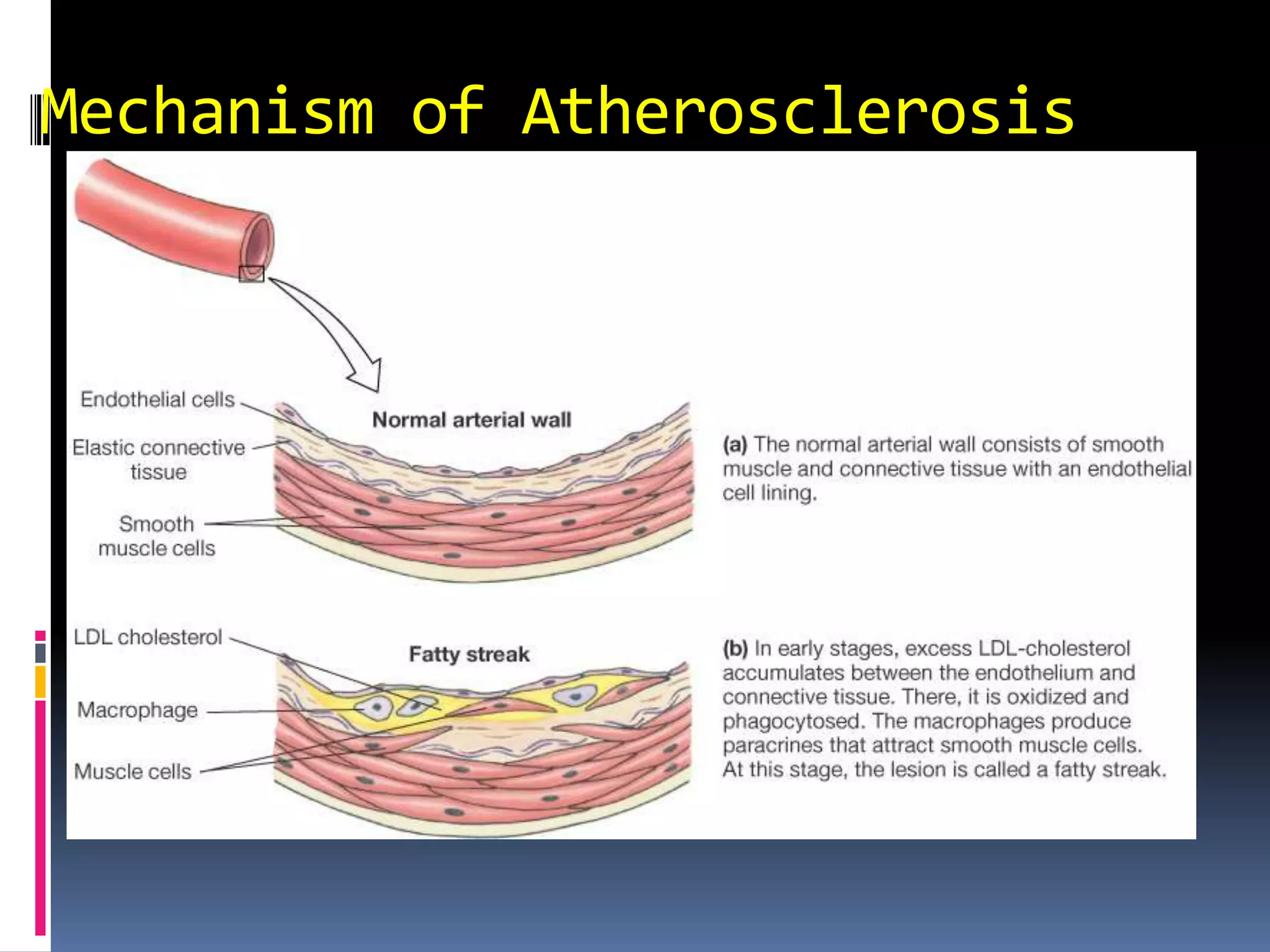
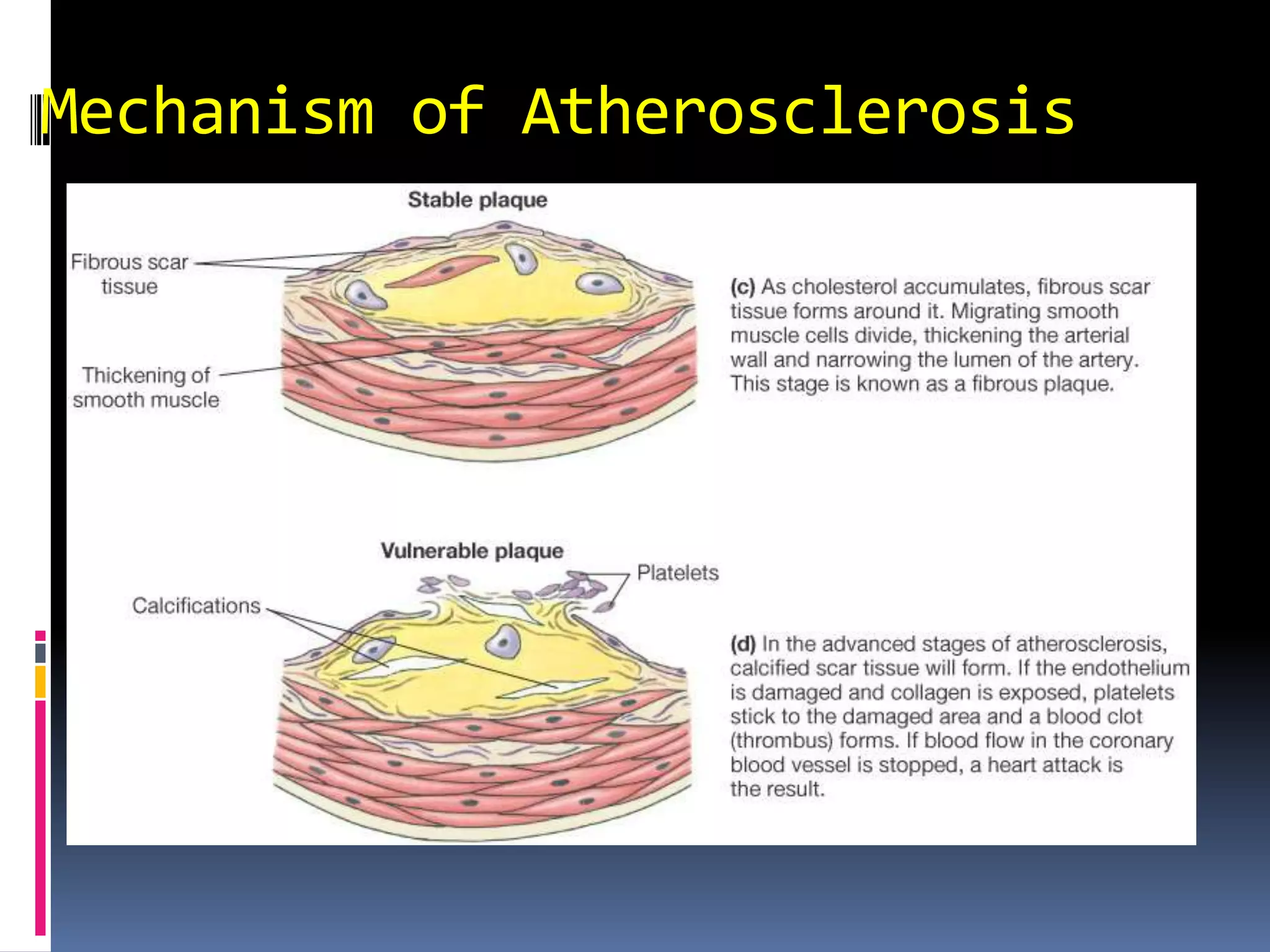
2. Atherosclerosis occurs when cholesterol builds up in artery walls, forming plaques that block coronary blood flow. This reduced flow can cause myocardial infarction (heart attack) if the flow is cut off to part of the heart muscle.
3. Cerebral blood flow is tightly regulated to maintain adequate oxygen and remove waste. It increases with higher carbon dioxide and hydrogen ion levels but is relatively unaffected by oxygen levels within normal ranges. Blood flow autoregulation keeps flow stable during changes in blood pressure.