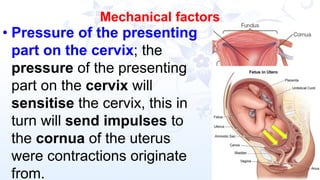
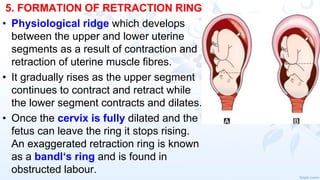
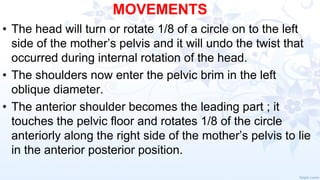
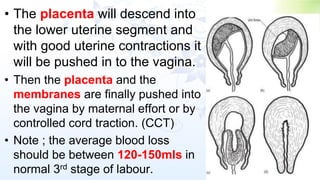
The document provides a comprehensive overview of normal labor, detailing definitions, stages, and physiological processes involved in childbirth. It emphasizes the role of skilled birth attendants, the factors influencing labor, and the signs indicating its onset. The information includes explanations of true versus false labor, the physiological changes during the stages of labor, and the management of women at each stage.