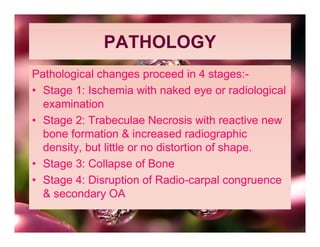
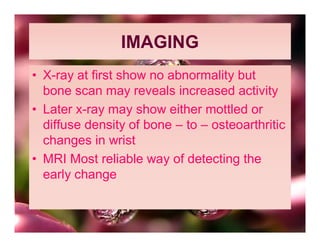
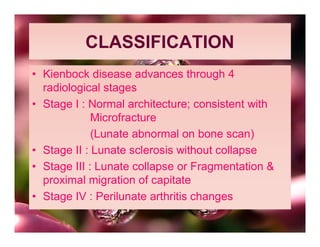
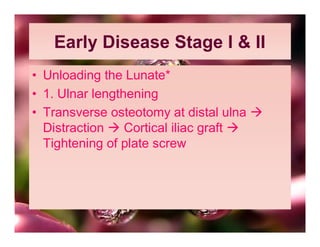
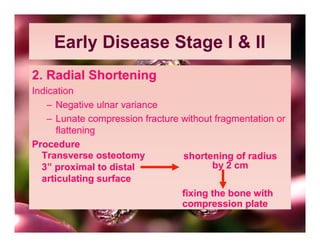
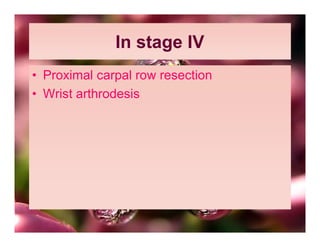
This document discusses Kienböck disease, an avascular necrosis of the lunate bone in the wrist. It begins by defining the disease and its discovery. The cause is unknown but is thought to be due to repetitive trauma causing microfractures. Those with an ulnar minus variance are at higher risk. It predominantly affects young men unilaterally in their dominant wrist. Imaging shows progressive sclerosis, fragmentation, and collapse of the lunate bone leading to wrist arthritis. Treatment involves casting for early stages or surgical options like ulnar lengthening, radial shortening, prosthesis, fusions, or resections depending on the stage of disease.