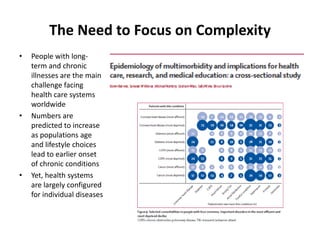
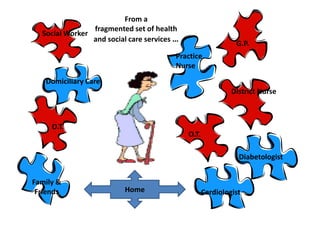
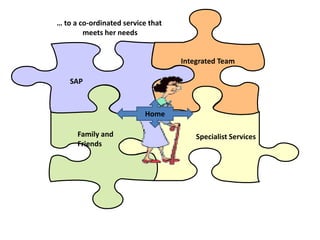
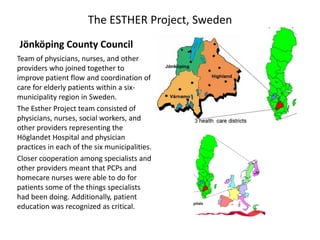
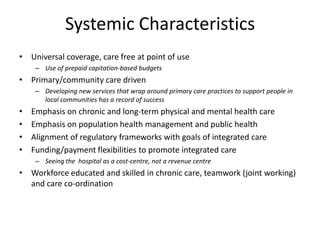
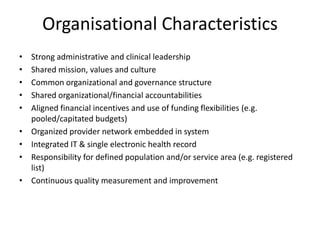
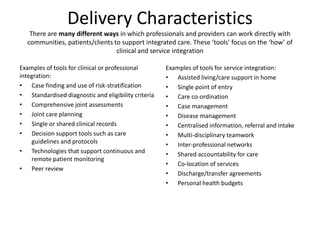
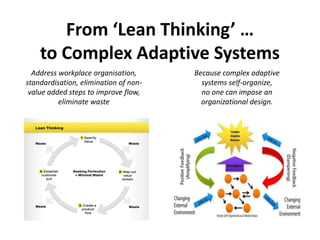
This document discusses innovative approaches to healthcare design for patients with complex needs. It argues that integrated care models are needed to address the growing challenges posed by aging populations with multiple chronic conditions. Successful integrated care models coordinate services around patient needs, rather than individual diseases. They feature elements like population-based approaches, multidisciplinary teams, and flexibility in funding and regulations. While lean thinking aims to streamline care, complex patients require systems that can adapt dynamically to changing needs through features like case management and care coordination between specialized and community-based providers.