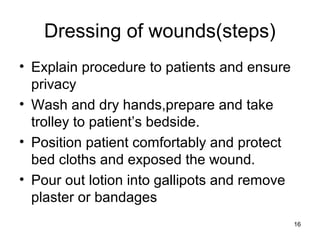
This document provides guidance on wound management and dressing for patients with Buruli ulcer wounds. It discusses the different types of wounds including intentional surgical wounds and accidental wounds caused by injury or disease. It describes the various presentations of Buruli ulcer wounds from clean to infected. The essential steps for wound dressing are outlined, including explaining the procedure, preparing materials, removing the old dressing gently, cleaning the wound, applying a new sterile dressing, and documenting findings. Proper wound management and dressing is important for Buruli ulcer patients to monitor the wound and prevent further infection.