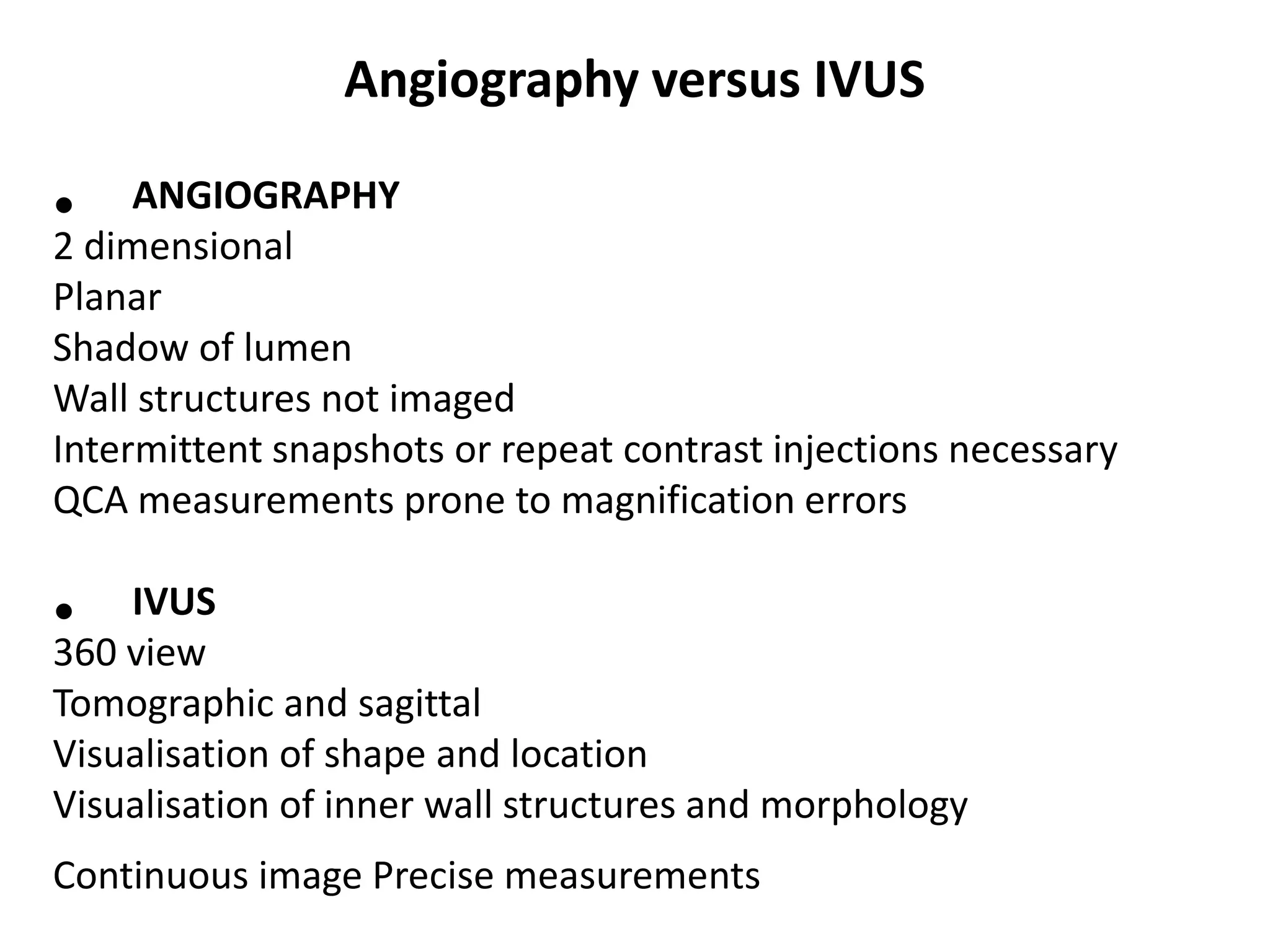
IVUS and OCT are intracoronary imaging modalities that provide information about coronary artery walls and atherosclerotic plaque beyond what can be seen through angiography alone. IVUS uses ultrasound to image plaque and vessel wall characteristics in 3D, while OCT has higher resolution but more limited depth, using near-infrared light. Both techniques can identify plaque morphology and composition, detect disease not seen on angiograms, and help assess stent results. IVUS is useful for pre-PCI decision making and vessel sizing while OCT can image plaque features at a higher resolution.