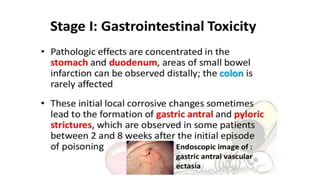
Iron is an essential element but can be toxic in high amounts. Iron poisoning most often occurs when children accidentally ingest iron supplements. Symptoms of iron toxicity can be severe and include vomiting, abdominal pain, shock, liver damage, and gastrointestinal bleeding and necrosis. Diagnosis involves measuring serum iron levels and a chelation challenge test. Treatment focuses on gastric lavage, administering charcoal or antacids, correcting dehydration and acidosis, and chelation therapy with desferrioxamine or deferiprone to remove excess iron from the body.