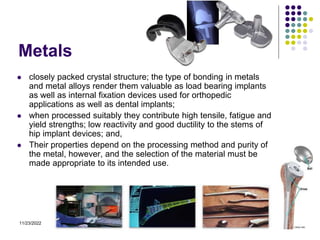
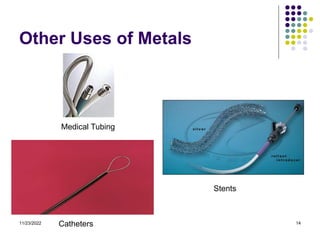
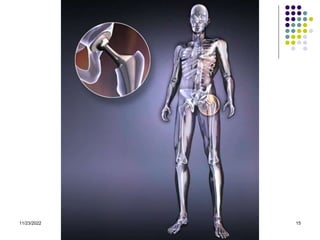
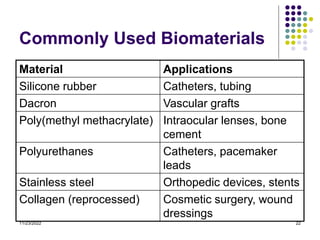
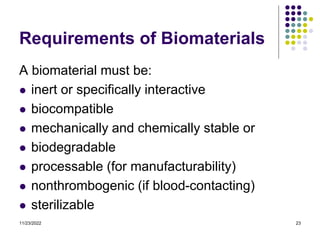
This document discusses different types of biomaterials used in medicine. It covers ceramics, metals, polymers, and composites. Ceramics are inorganic compounds formed at high temperatures and used in applications like hip and dental implants. Metals are useful for load bearing implants due to their strength but can cause stress shielding. Polymers are flexible materials made of repeating units useful for applications like catheters. Composites combine materials like polymers and ceramics to get desired properties. The document also discusses requirements for biomaterials and progress in the field.
![11/23/2022 7
Ceramics
Inorganic compounds that contain metallic and non-metallic
elements, for which inter-atomic bonding is ionic or covalent, and
which are generally formed at high temperatures.
Derivation: From the Greek word "keramos" meaning the art and
science of making and using solid articles formed by the action of
heat on earthy raw materials.
Most ceramics occur as minerals:
(1) The abundance of elements and geochemical characteristics of
the earth’s crust govern mineral types.
(2) Composition of Earth’s Crust: [84% = O + Si + Al]
O = 50% Fe = 5% K = 2.5%
Si = 26% Ca = 3% Mg = 2%
Al = 8% Na = 2.5% H = 1%](https://image.slidesharecdn.com/introtobiomaterials-221123011805-bc3f3a3f/85/Intro-to-biomaterials-ppt-7-320.jpg)