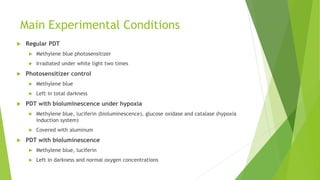
This document summarizes a student project that aims to improve photodynamic therapy (PDT) for cancer treatment. The student hypothesizes that inducing hypoxic conditions in tumor cells will decrease the effectiveness of a photosensitizer and bioluminescent reagent in PDT. In experiments, the student cultures tumor cells under normal and hypoxic conditions with different PDT treatments and measures cell viability. The results show that bioluminescence was not an effective light source due to poor absorption overlap with the photosensitizer. Further work is needed to optimize photosensitizers and light sources to overcome limitations of conventional PDT.