Photodynamic therapy (PDT) involves using a photosensitizing drug and a light source to damage cancer or abnormal tissues. The photosensitizing drug is administered and absorbed by tissues, then activated by exposure to a specific wavelength of light, which causes the drug to produce reactive oxygen species that destroy the targeted cells. PDT can be used to treat a variety of cancers and pre-cancerous conditions depending on the photosensitizing drug and light source used. It offers advantages such as precision targeting and minimal scarring or invasiveness compared to other treatments.
![• Photodynamic therapy (PDT) is the
treatment that use light to damage
cancer or abnormal tissue[1].
• It requires a light source, combine with a
drug that makes the tissues light
sensitive which is known as a
photosensitizer[1].
• A photosensitizer drug is given to the
patient orally, IV, topically (treat skin
lesion) a few hours to days prior to the
light exposure, but the drugs is not
activated until it is exposed to a
particular lesser light[1].
INTRODUCTION](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-3-320.jpg)
![• PDT is generally not use to treat large
tumors, because the light cannot reach the
necessary depth to treat those tumors[1].
• Different photosensitizers are activated by
the different wavelength of light[1];
therefore defending on the area of the
body to be treated, there are different
types of photosensitizing drugs and
different wavelength of light that can be
use[1].
INTRODUCTION CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-4-320.jpg)
![• The procedure was invented by a German
physician known as Friedrich Meyer-Betz
in 1913 the procedure was called
photoradiation therapy (PRT) which is
done by the injection of porphyrin and
exposing the patient to light[2].
BRIEF HISTORY.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-5-320.jpg)
![BRIEF HISTORY CONT.
Friedrich, injected himself with
porphyrin in 1913[2].](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-6-320.jpg)
![• It was John Toth wrote the first white
paper renaming the therapy as
“Photodynamic Therapy” (PDT)[2].
• PDT received even a greater interest as a
result of Thomas Dougherty helping
expand clinical trial and forming the
international photodynamic Association,
in 1986[2].
BRIEF HISTORY CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-7-320.jpg)
![• Photodynamic therapy is the treatment
that uses special drugs, called
photosensitizing agent, along with light to
kill cancer cells[1].
• It also known as photoradiation therapy,
phototherapy, photochmotherapy[1].
DEFINITION.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-8-320.jpg)
![DEFINITION CONT.
Treatment of cancer using
PDT[2].](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-9-320.jpg)
![PDT equipment includes:
• PDT machine
• Light source
• Bed
• Electrical source[2].
EQUIPMENT](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-10-320.jpg)
![EQUIPMENT CONT.
PDT
machine
and some
of its
component
[2].](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-11-320.jpg)

![EQUIPMENT CONT.
Different colors of lesser
with different wavelength
used for PDT[2].](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-13-320.jpg)
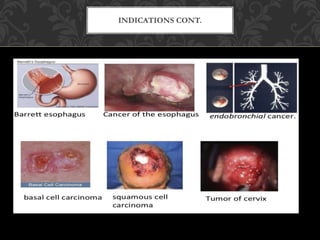
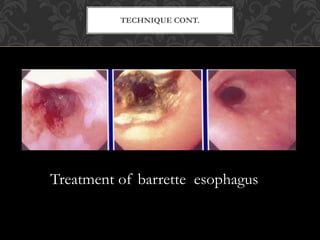
![• Generic Name: porfimer
• Trade Name: photofrin
• Using porfimer to treat :
• Cancer of the esophagus
• Relieve some tumors that are totally blocking the
esophagus
• Barrett esophagus,
• Endobranchial cancer
• Some skin cancers such as: nasal cell carcinoma and
some squamous cell carcinoma
• Some tumors of the vagina, vulva, and cervix that
can be reach by the activating light[3].
INDICATIONS](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-14-320.jpg)
![• Porfimer sodium is NOT recommended
for patients with:
• A fistula
• A tumor that is spreading into a major
blood vessels, Enlarged veins in the
stomach or ulcer in the esophagus[3].
CONTRAINDICATIONS.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-16-320.jpg)
![The major possible side effects from the
porfimer sodium are :
• Photosensitivity reaction
• Swelling in the treated area, swelling may
cause pain or trouble in swallowing and
breathing[3].
COMPLICATIONS.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-17-320.jpg)
![• First, the porfimer sodium is given through
vein.
• It travels through the bloodstream and
absorbed by all cell in the body both normal
and cancer cells.
• The normal cells get rid of the porfimer
sodium over couple of days.
• But a lot of the drugs stay in the cancer cells
and in normal skin cells.
• Porfimer sodium must be activated turn on
with the light[3].
TECHNIQUE](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-18-320.jpg)
![• The activation is done about 2-3 days after
the injection of the drug
• This gives the normal cells a chance to get
rid of the drug.
• The operator direct a red lesser light at the
area of cancer cells using thing fiber optic
glass strand.
• The laser used is a lower-power light so it
does not burn, it causes little or no pain[3].
TECHNIQUE CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-19-320.jpg)
![• The light is applied for 5-40mins, depending
on the size of the tumor.
• Any dead tissue left in the treated area is
removed about 4-5days later during
endoscopy or bronchoscopy.
• The treatment can be repeated if needed[3].
TECHNIQUE CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-20-320.jpg)
![Using Aminolevulinic acid :
• Generic name: ALA; Aminolevulinate;
delta-Aminolevulinic acid
• Trade Names: Aladerm; kerastick;
levulan kerastick
• Aminolevulinic acid is a drug that is put
right on the skin. It is used to treat
actinic keratosis
• Mycosis fungoides[4].
INDICATIONS .](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-22-320.jpg)

![Aminolevulinic acid is NOT recommended
for patients with skin sensitivity to blue
light[4].
CONTRAINDICATIONS.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-24-320.jpg)
![• Reactions caused by the light can show up
on the skin where the drug is applied.
• It usually involve redness and a tingling or
burning sensation
• Sunscreen will not protect the skin from
photosensitivity reactions.
• The treated skin will likely turn red and may
swell after treatment
• The skin may also be itchy or change colour
after treatment[4].
COMPLICATIONS.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-25-320.jpg)
![• Aminolevulinic acid is a solution that is
applied directly to the lesion or spot on the
face or scalp.
• About 14 to 15 hours after the drug is
applied or the next day the operator expose
the area being treated to a blue light for
about 15min
• During the therapy both the patient and
operator most wear a protective eyewear[4].
TECHNIQUE.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-26-320.jpg)
![• The treated area may get red and scale
and crust for up to 4 weeks before
healing.
• If the lesion does not completely treated
the treatment can be repeated 8 weeks
from the initial treatment[4].
TECHNIQUE CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-27-320.jpg)

![• Using visudyne
• Generic Name: benzoporphyrin
• Trade Name: verteporfin
• For treatment of ;
• Presumed ocular histoplasmosis
• Due to age related macular
degeneration[3].
INDICATIONS](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-29-320.jpg)
![• Extravasation produce severe pain,
inflammation, swelling or discoloration
• Visual disturbance[3].
COMPLICATIONS](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-30-320.jpg)
![• Administer by IV infusion using an
appropriate syringe pump and line filter a
pore size of 0.22-1.2mcm
• Protect the dilute solution from the bright
light during the administration.
• Avoid contact contact with eye and skin
during the preparation and administration
• The drug is activated by low-intensity laser
light[4].
TECHNIQUE](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-31-320.jpg)
![• The photosensitizer moves from ground
state to an excited singlet state and an
excited triplet state[2]
• Molecular oxygen is present at its ground
triplet state when the photosensitizer and
oxygen molecule are in proximity, an
energy transfer can take that place that
allows the photosensitizer to relax to its
ground state[2].
MECHANISM OF ACTION](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-32-320.jpg)
![• This may create an excited singlet state
oxygen molecule[2].
• Since singlet oxygen is highly reactive
and cytotoxic, the tumor cells are
destroyed[2].
MECHANISM OF ACTION CONT.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-33-320.jpg)
![MECHANISM OF ACTION CONT.
The above diagram shows how
photosensitizer get rid of the cancer
cells[2].](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-34-320.jpg)
![• Its has no long-time side effect when used
properly.
• It is less invasive than surgery.
• It usually takes only a short time and is most
often done as an outpatient.
• It can be targeted very precisely.
• It can be repeated many times at the same site.
• There is little or no scaring after the site heals.
• It often cost less than other cancer
treatments[5].
ADVANTAGES.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-35-320.jpg)
![• It can only treat areas where light can reach.
• It can not be used to treat large cancers.
• Photosensitivity reactions[5].
LIMITATIONS..](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-36-320.jpg)
![• Studies are now being done to test the use
of PDT for several type of cancers and pre-
cancerous conditions, including cancers of
the: skin, cervix, bladder, prostate, bile duct,
pancreas, stomach, brain, larynx[5].
• Newer photosensitizing drugs now being
studied and it may have more advantages
over the current ones, example is
photochlor- a 2nd generation
photosensitizer[5].
CONCLUSION.](https://image.slidesharecdn.com/pdt-technique-200416101052/85/Photodynamic-therapy-technique-37-320.jpg)