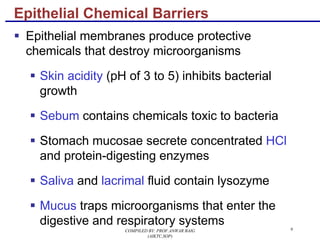
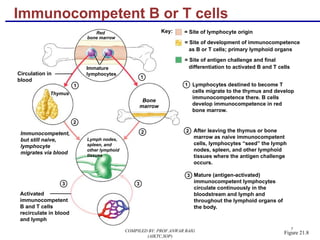
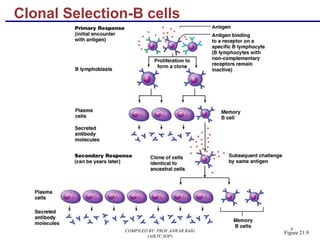
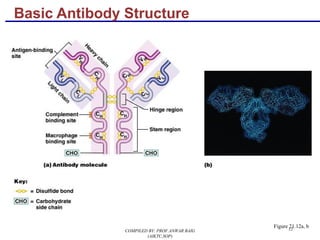
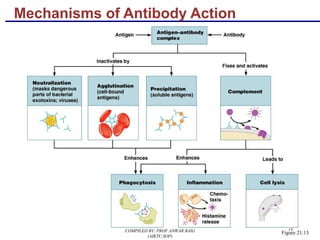
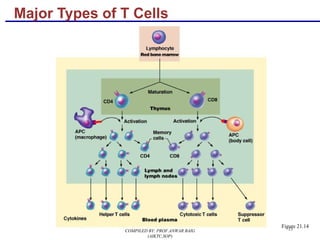
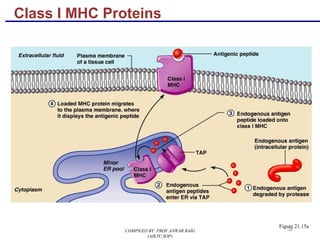
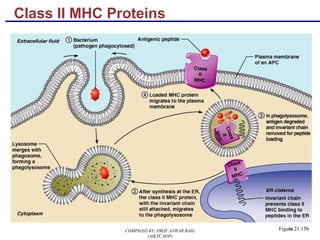
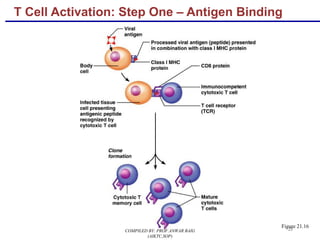
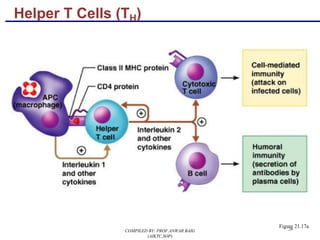
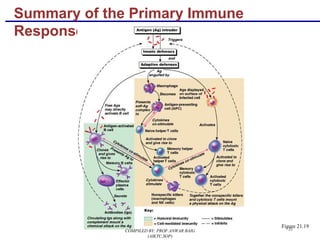
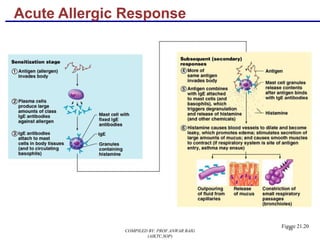
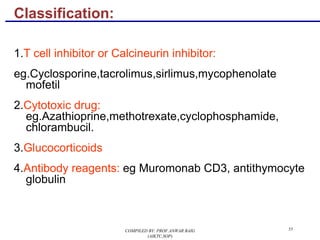
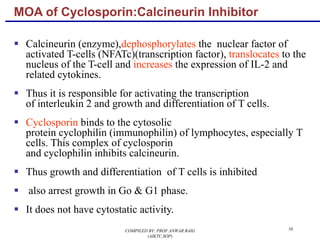
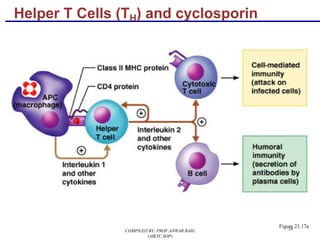
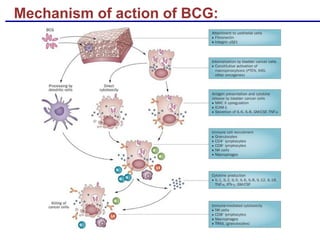
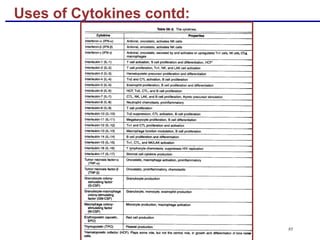
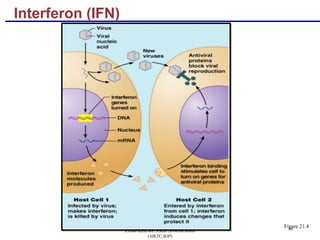
The document provides an overview of immunology and the immune system. It discusses the innate and adaptive immune systems, including barriers, cells, antibodies, and cytokines involved. It also covers immunological concepts like antigen presentation, T cell and B cell activation, immunological memory, immunodeficiencies, autoimmunity, and hypersensitivities. The document is a compilation on immunology created by Prof. Anwar Baig for students.