Genital ulcers can be caused by infections such as herpes simplex virus, syphilis, chancroid, and lymphogranuloma venereum or by non-infectious causes. Clinical diagnosis of the cause is difficult so tests for syphilis, herpes simplex virus, and chancroid should be considered in all patients. Treatment depends on the suspected cause but herpes simplex virus is usually treated with oral acyclovir and syphilis with intramuscular penicillin G benzathine.




![American Family Physician
during labor.44 Suppressive therapy reduces the risk
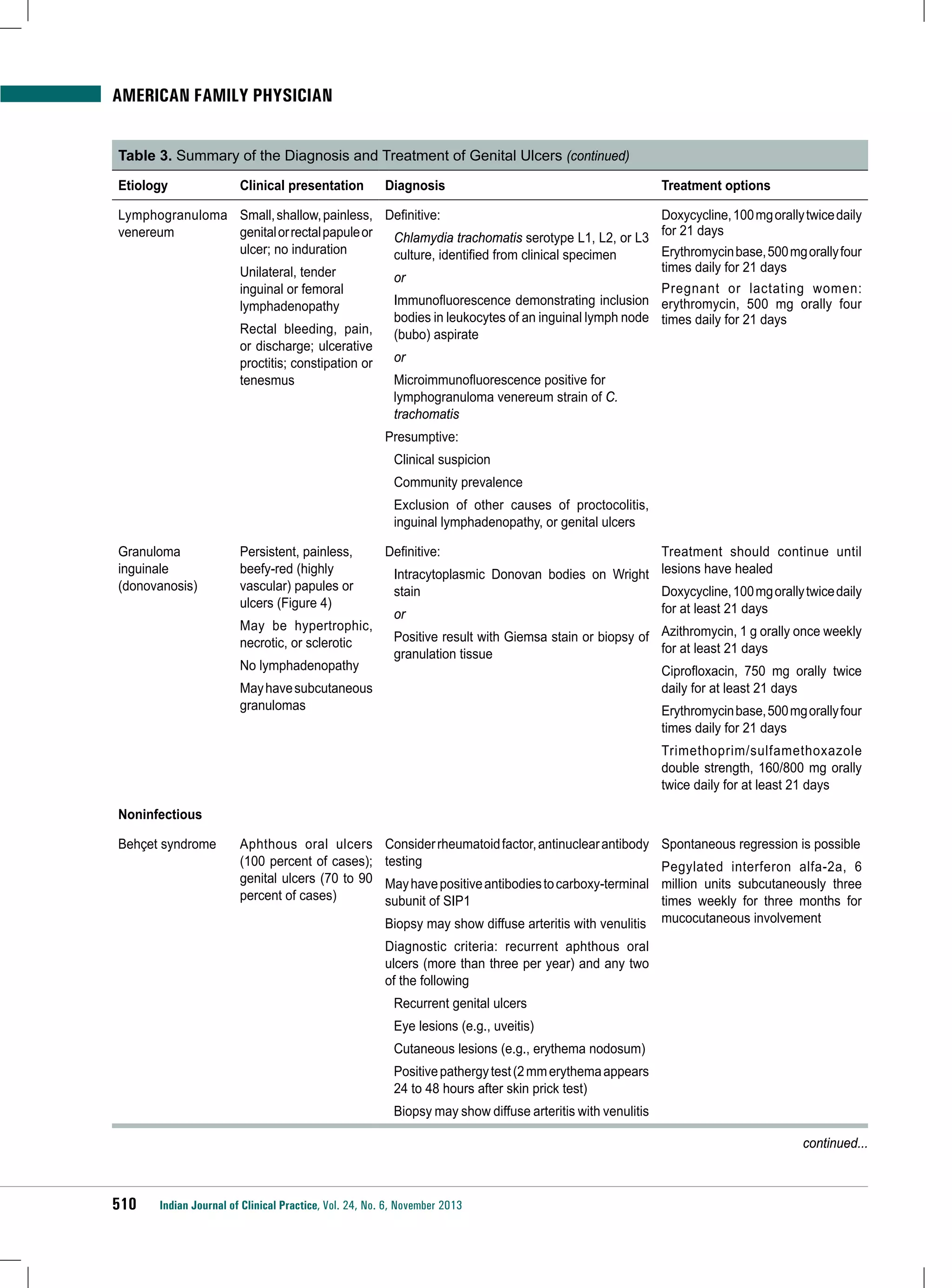
of recurrence by 75 percent and the rate of cesarean
delivery because of HSV lesions by 40 percent.45
REFERENCES
1. Augenbraun MH. Diseases of the reproductive organs
and sexually transmitted diseases: genital skin and
mucous membrane lesions. In: Mandell GL, Bennett JE,
Dolin R, eds. Mandell, Douglas, and Bennett’s Principles
and Practice of Infectious Diseases. 7th ed. Philadelphia,
Pa.: Churchill Livingstone; 2009:1475-1484.
2. Louden BA, Jorizzo JL. Behcet’s disease. In: Firestein GS,
Budd RC, Harris ED, McInnes IB, Ruddy S, Sergent JS, eds.
Kelley’s Textbook of Rheumatology. 8th ed. Philadelphia,
Pa.: Elsevier, Inc.; 2009:1475-1480.
3. Workowski KA, Berman S; Centers for Disease Control
and Prevention. Sexually transmitted diseases treatment
guidelines, 2010 [published correction appears in MMWR
Recomm Rep. 2011;60(1):18]. MMWR Recomm Rep.
2010;59(RR-12):1-110.
4. Low N, Broutet N, Adu-Sarkodie Y, Barton P, Hossain
M, Hawkes S. Global control of sexually transmitted
infections. Lancet. 2006;368(9551):2001-2016.
5. Cohen DE, Mayer K. Genital ulcer disease. In: Klausner
JD, Hook EW III, eds. Current Diagnosis & Treatment of
Sexually Transmitted Diseases. New York, NY: McGrawHill Medical; 2007:19-26.
6. Centers for Disease Control and Prevention. CDC fact
sheet. Genital herpes. http://www.cdc.gov/std/herpes/
herpes-fact-sheet-lowres-2010.pdf. Accessed September
27, 2010.
7. U.S. Department of Health and Human Services, Centers
for Disease Control and Prevention. Sexually transmitted
disease surveillance 2009. http://www.cdc.gov/std/
stats09/surv2009-Complete.pdf. Accessed May 8, 2011.
8. Centers for Disease Control and Prevention. CDC fact
sheet. Syphilis. http://www.cdc.gov/std/syphilis/syphilisfact-sheet-press.pdf. Accessed September 27, 2010.
9. Centers for Disease Control and Prevention. Chancroid:
tracking the hidden epidemics. Trends in STDs in the
United States. 2000. http://www.cdc.gov/std/Trends2000/
chancroid.htm. Accessed September 14, 2011.
10. Centers for Disease Control and Prevention. CDC fact
sheet. LGV. http://www.cdc.gov/std/lgv/LGV-Fact-Sheet.
pdf. Accessed September 27, 2011.
11. de Menthon M, Lavalley MP, Maldini C, Guillevin
L, Mahr A. HLA-B51/B5 and the risk of Behçet’s
disease: a systematic review and meta-analysis of casecontrol genetic association studies. Arthritis Rheum.
2009;61(10):1287-1296.
12. Schiffer JT, Corey L. Herpes simplex virus. In: Mandell GL,
Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s
Principles and Practice of Infectious Diseases. 7th ed.
Philadelphia, Pa.: Churchill Livingstone; 2009:1943-1962.
514
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
13. Burstein GR. Sexually transmitted infections. In: Kliegman
R, Nelson WE, eds. Nelson Textbook of Pediatrics. 19th
ed. Philadelphia, Pa.: Saunders; 2011:705-714.
14. Alpsoy E, Durusoy C, Yilmaz E, et al. Interferon alfa-2a
in the treatment of Behçet disease: a randomized placebocontrolled and double-blind study. Arch Dermatol.
2002;138(4):467-471.
15. Warts, herpes simplex and other viral infections. In:
Clinical Dermatology: A Color Guide to Diagnosis and
Therapy. Habif TP, ed. 5th ed. Edinburgh, Scotland:
Mosby; 2010:454-490.
16. O’Meara SM, Cullum NA, Majid M, Sheldon TA.
Systematic review of antimicrobial agents used for
chronic wounds. Br J Surg. 2001;88(1):4-21.
17. Sharma R, Dronen SC. Herpes simplex in emergency
medicine. Medscape Reference. http://emedicine.medscape.
com/article/783113-overview. Accessed September 13, 2011.
18. Wald A, Zeh J, Selke S, et al. Reactivation of genital
herpes simplex virus type 2 infection in asymptomatic
seropositive persons. N Engl J Med. 2000;342(12):844-850.
19. Kimberlin DW, Rouse DJ. Clinical practice. Genital herpes.
N Engl J Med. 2004;350(19):1970-1977.
20. Lewis DA. Chancroid: clinical manifestations, diagnosis,
and management. Sex Transm Infect. 2003;79(1):68-71.
21. Sethi G, Allason-Jones E, Richens J, et al. Lymphogranuloma
venereum presenting as genital ulceration and inguinal
syndrome in men who have sex with men in London,
UK [published correction appears in Sex Transm Infect.
2009;85(5):406]. Sex Transm Infect. 2009;85(3):165-170.
22. Velho PE, Souza EM, Belda Junior W. Donovanosis. Braz J
Infect Dis. 2008;12(6):521-525.
23. Klippel JH, Weyand CM. Wortmann R, eds. Primer on
the Rheumatic Diseases. 11th ed. Atlanta, Ga.: Arthritis
Foundation; 1997:89.
24. Mat MC, Goksugur N, Engin B, Yurdakul S, Yazici
H. The frequency of scarring after genital ulcers in
Behçet’s syndrome: a prospective study. Int J Dermatol.
2006;45(5):554-556.
25. Ashley RL. Sorting out the new HSV type specific
antibody tests. Sex Transm Infect. 2001;77(4):232-237.
26. Wald A, Huang ML, Carrell D, Selke S, Corey L.
Polymerase chain reaction for detection of herpes simplex
virus (HSV) DNA on mucosal surfaces: comparison with
HSV isolation in cell culture. J Infect Dis. 2003;188(9):
1345-1351.
27. Fleming DT, McQuillan GM, Johnson RE, et al. Herpes
simplex virus type 2 in the United States, 1976 to 1994.
N Engl J Med. 1997;337:1105-1111.
28. Bruisten SM, Cairo I, Fennema H, et al. Diagnosing genital
ulcer disease in a clinic for sexually transmitted diseases
in Amsterdam, The Netherlands. J Clin Microbiol.
2001;39(2):601-605.
29. Fife KH, Barbarash RA, Rudolph T, Degregorio B, Roth
R. Valaciclovir versus acyclovir in the treatment of first-](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-14-2048.jpg)
![American Family Physician
episode genital herpes infection. Results of an international,
multicenter, double-blind, randomized clinical trial. The
Valaciclovir International Herpes Simplex Virus Study
Group. Sex Transm Dis. 1997;24(8):481-486.
30. Saenz A, Ausejo M, Shea B, Wells G, Welch V, Tugwell
P. Pharmacotherapy for Behcet’s syndrome. Cochrane
Database Syst Rev. 2000;(2):CD001084.
31. Alpsoy E, Er H, Durusoy C, Yilmaz E. The use of sucralfate
suspension in the treatment of oral and genital ulceration
of Behçet disease: a randomized, placebo-controlled,
double-blind study. Arch Dermatol. 1999;135(5):529-532.
32. Powers KA, Poole C, Pettifor AE, Cohen MS. Rethinking
the heterosexual infectivity of HIV-1: a systematic review
and meta-analysis. Lancet Infect Dis. 2008;8(9):553-563.
33. Krieger JN. Prostatitis, epididymitis, and orchitis: semen
as a vector for human immunodeficiency virus. In:
Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas,
and Bennett’s Principles and Practice of Infectious
Diseases. 7th ed. Philadelphia, Pa.: Churchill Livingstone;
2009:1521-1527.
34. U.S. Preventive Services Task Force. Screening
for syphilis infection. July 2004. http://www.
uspreventiveservicestaskforce.org/uspstf/uspssyph.htm.
Accessed September 13, 2011.
35. U.S. Preventive Services Task Force. Screening
for genital herpes. March 2005. http://www.
uspreventiveservicestaskforce.org/uspstf05/herpes/
herpesrs.htm. Accessed September 13, 2011.
36. Kim HN, Wald A, Harris J, Almekinder J, Heitman C, Corey
L. Does frequency of genital herpes recurrences predict
risk of transmission? Further analysis of the valacyclovir
transmission study. Sex Transm Dis. 2008;35(2):124-128.
37. Martin ET, Krantz E, Gottlieb SL, et al. A pooled analysis
of the effect of condoms in preventing HSV-2 acquisition
[published correction appears in Arch Intern Med.
2010;170(11):929]. Arch Intern Med. 2009;169(13):12331240.
38. Wald A, Langenberg AG, Link K, et al. Effect of condoms
on reducing the transmission of herpes simplex virus type
2 from men to women. JAMA. 2001;285(24):3100-3106.
39. American College of Obstetricians and Gynecologists.
Gynecologic herpes simplex virus infections. ACOG
Practice Bulletin no. 57. Washington, DC: American
College of Obstetricians and Gynecologists; 2004.
40. Corey L, Wald A, Patel R, et al.; Valacyclovir HSV
Transmission Study Group. Once-daily valacyclovir to
reduce the risk of transmission of genital herpes. N Engl J
Med. 2004;350(1):11-20.
41. Diaz-Mitoma F, Sibbald RG, Shafran SD, Boon R,
Saltzman RL. Oral famciclovir for the suppression of
recurrent genital herpes: a randomized controlled trial.
Collaborative Famciclovir Genital Herpes Research
Group. JAMA. 1998;280(10):887-892.
42. Bodsworth NJ, Crooks RJ, Borelli S, et al. Valaciclovir
versus aciclovir in patient initiated treatment of recurrent
genital herpes: a randomised, double blind clinical trial.
International Valaciclovir HSV Study Group. Genitourin
Med. 1997;73(2):110-116.
43. Wald A, Selke S, Warren T, et al. Comparative efficacy of
famciclovir and valacyclovir for suppression of recurrent
genital herpes and viral shedding. Sex Transm Dis.
2006;33:529-533.
44. Randolph AG, Hartshorn RM, Washington AE. Acyclovir
prophylaxis in late pregnancy to prevent neonatal herpes:
a cost-effectiveness analysis. Obstet Gynecol. 1996;88(4 pt
1):603-610.
45. Sheffield JS, Hollier LM, Hill JB, Stuart GS, Wendel
GD. Acyclovir prophylaxis to prevent herpes simplex
virus recurrence at delivery: a systematic review. Obstet
Gynecol. 2003;102(6):1396-1403.
■■■■
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
515](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-15-2048.jpg)
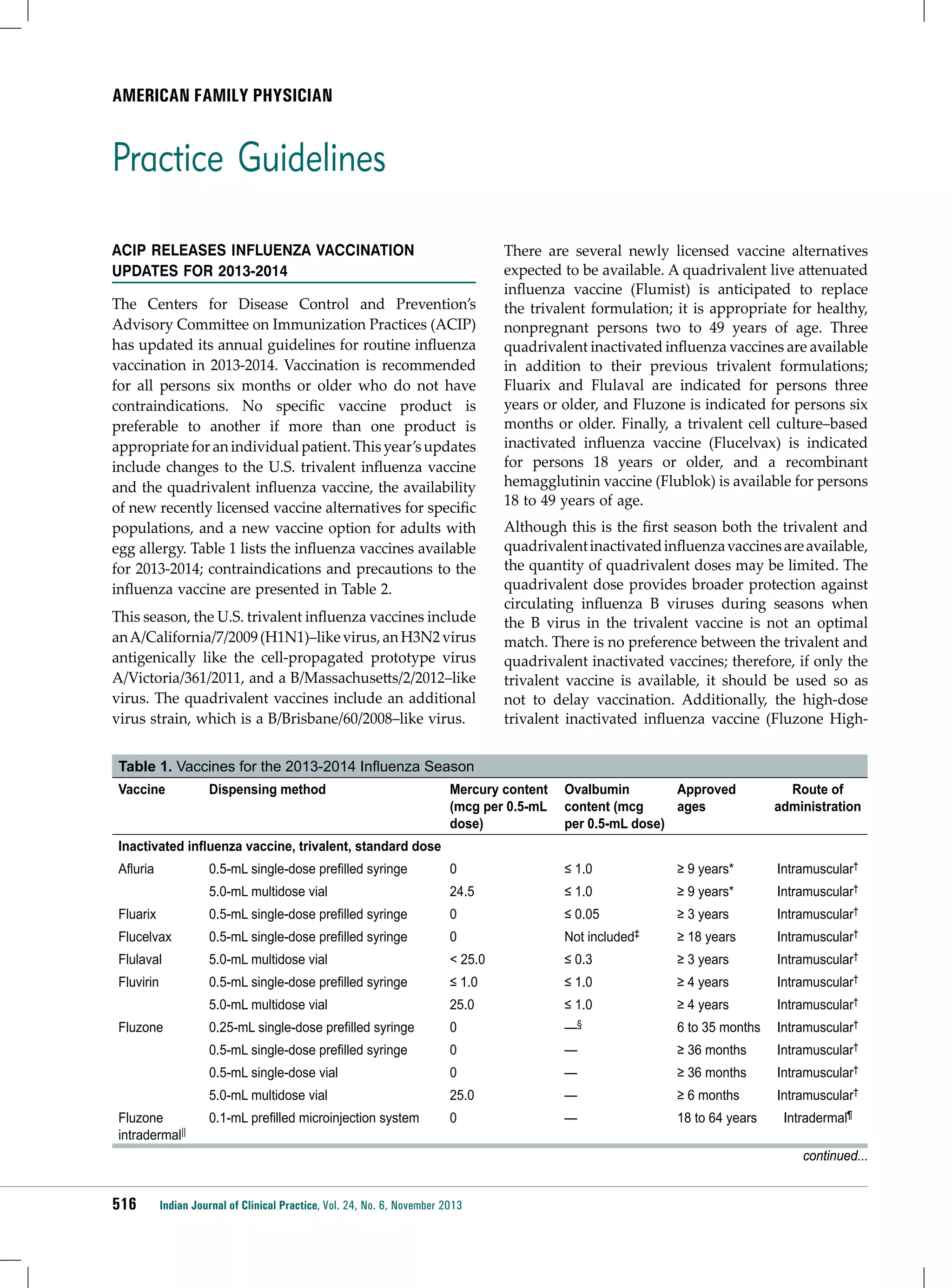
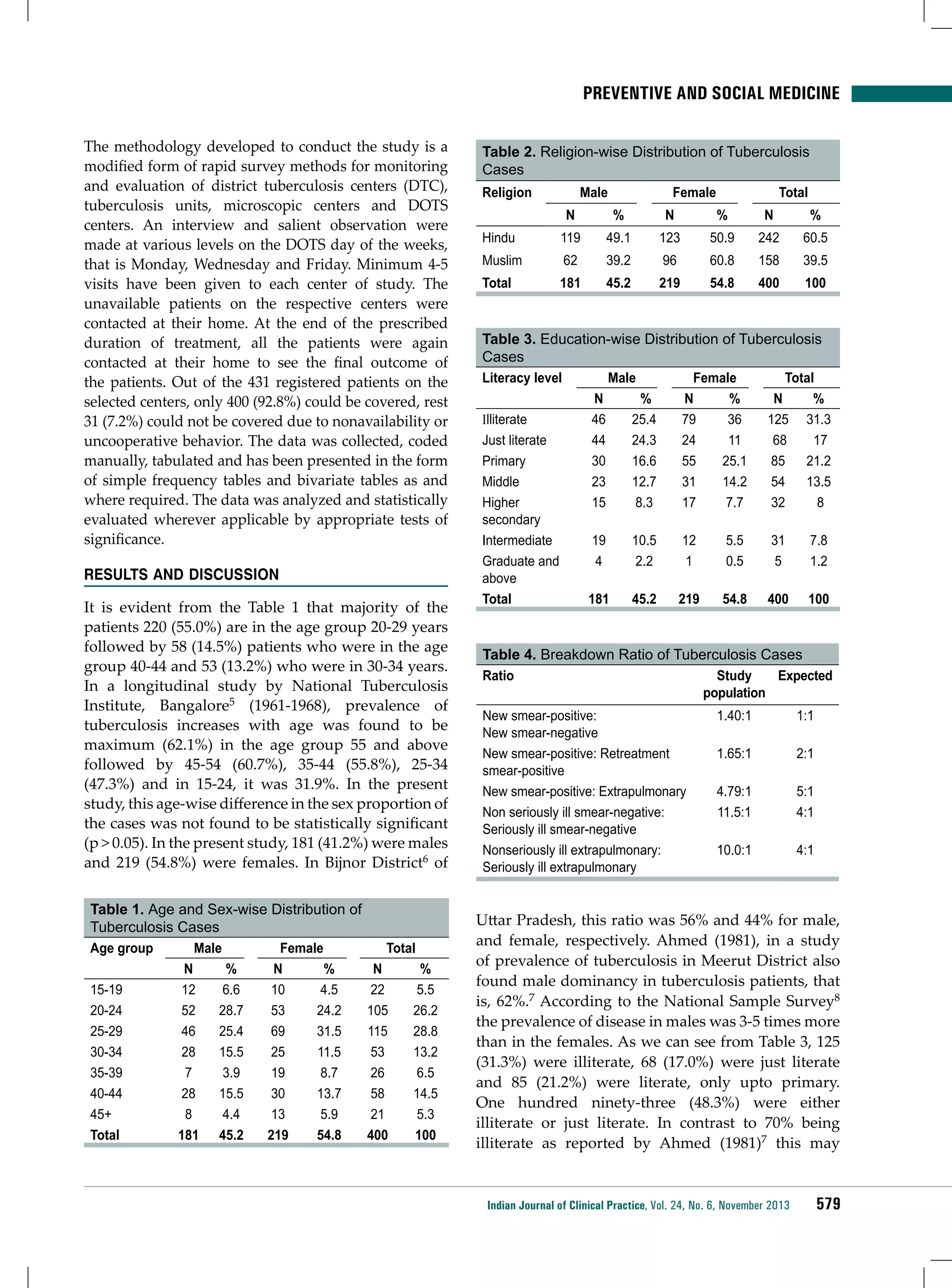
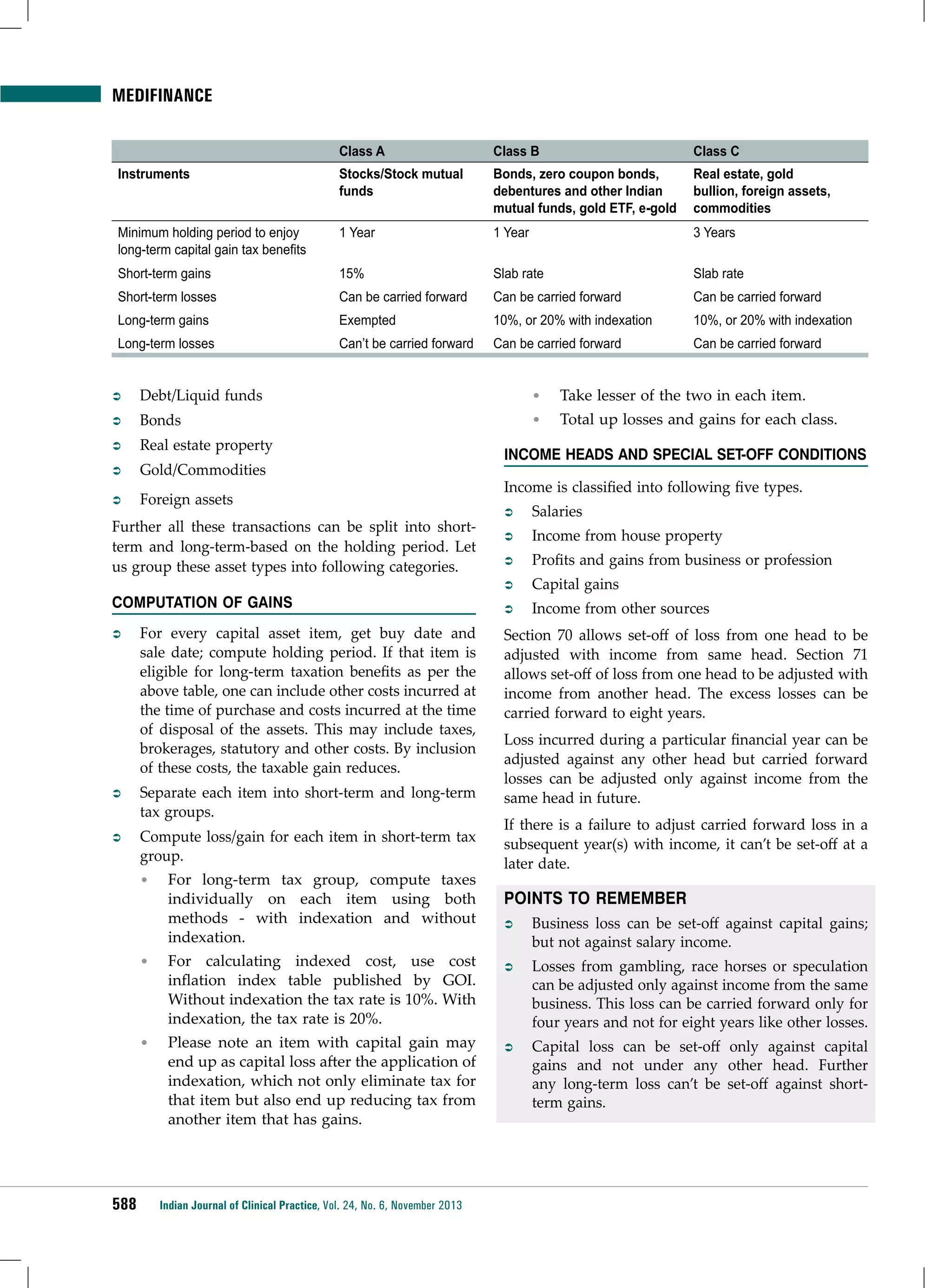
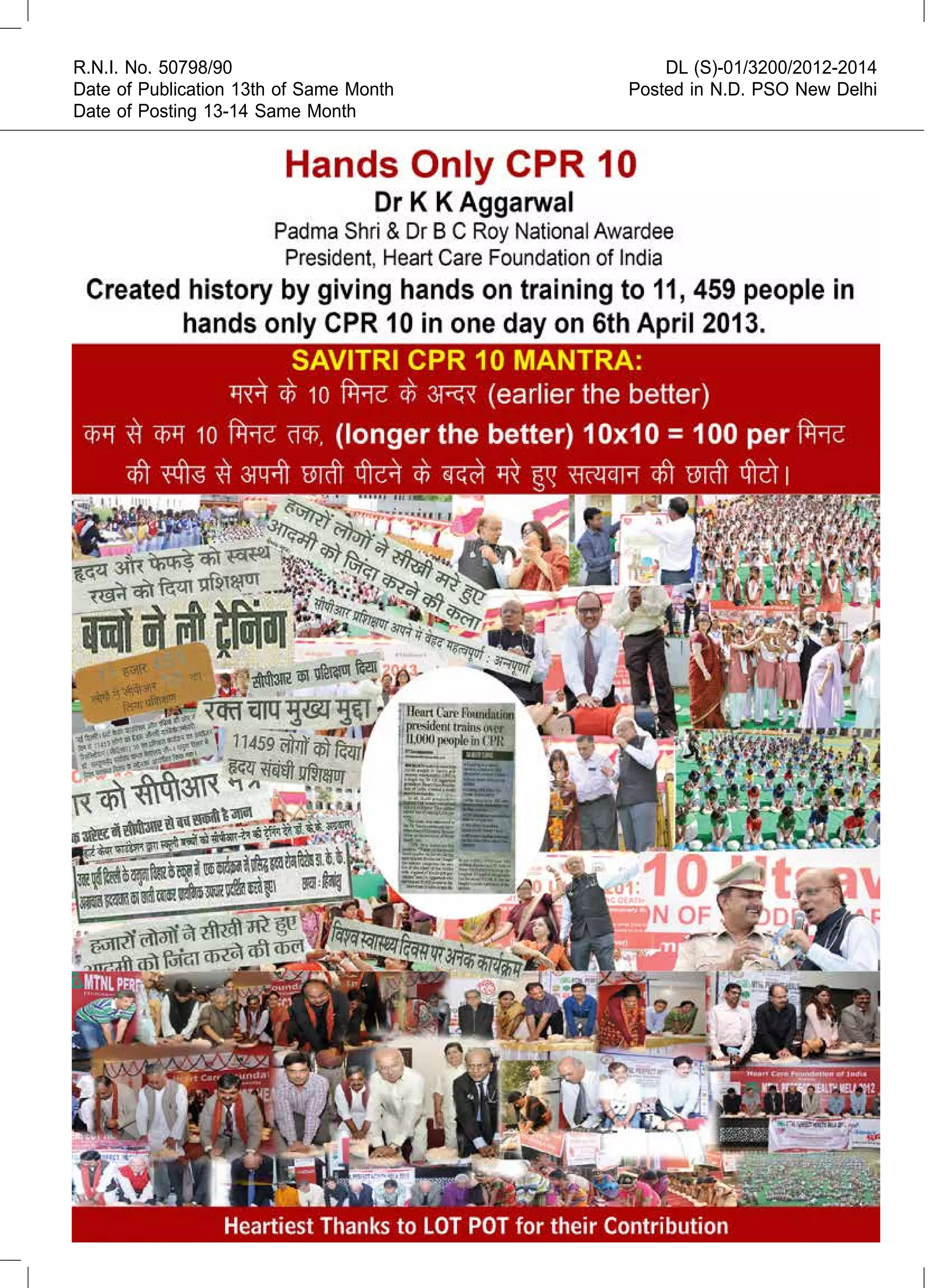
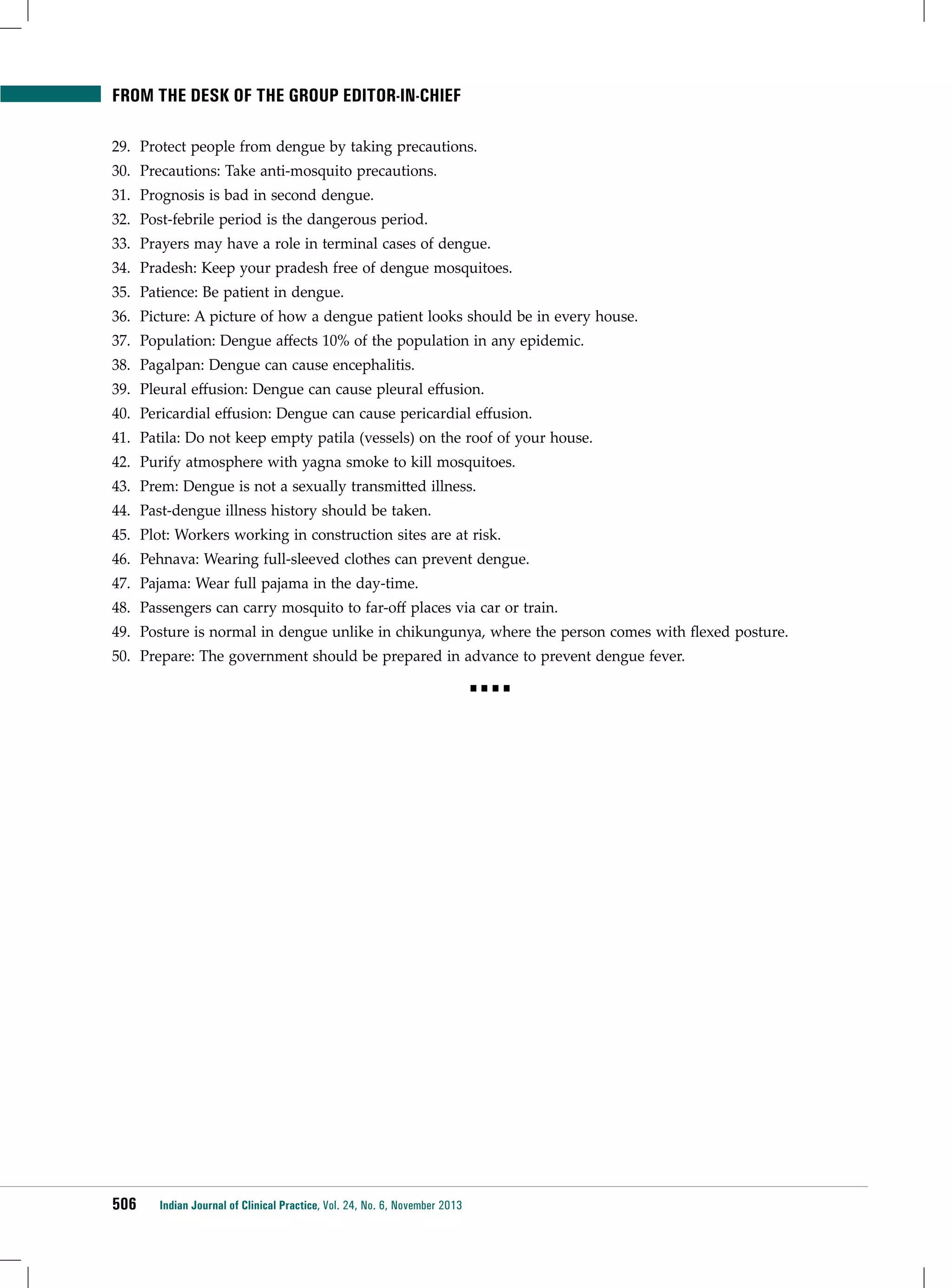
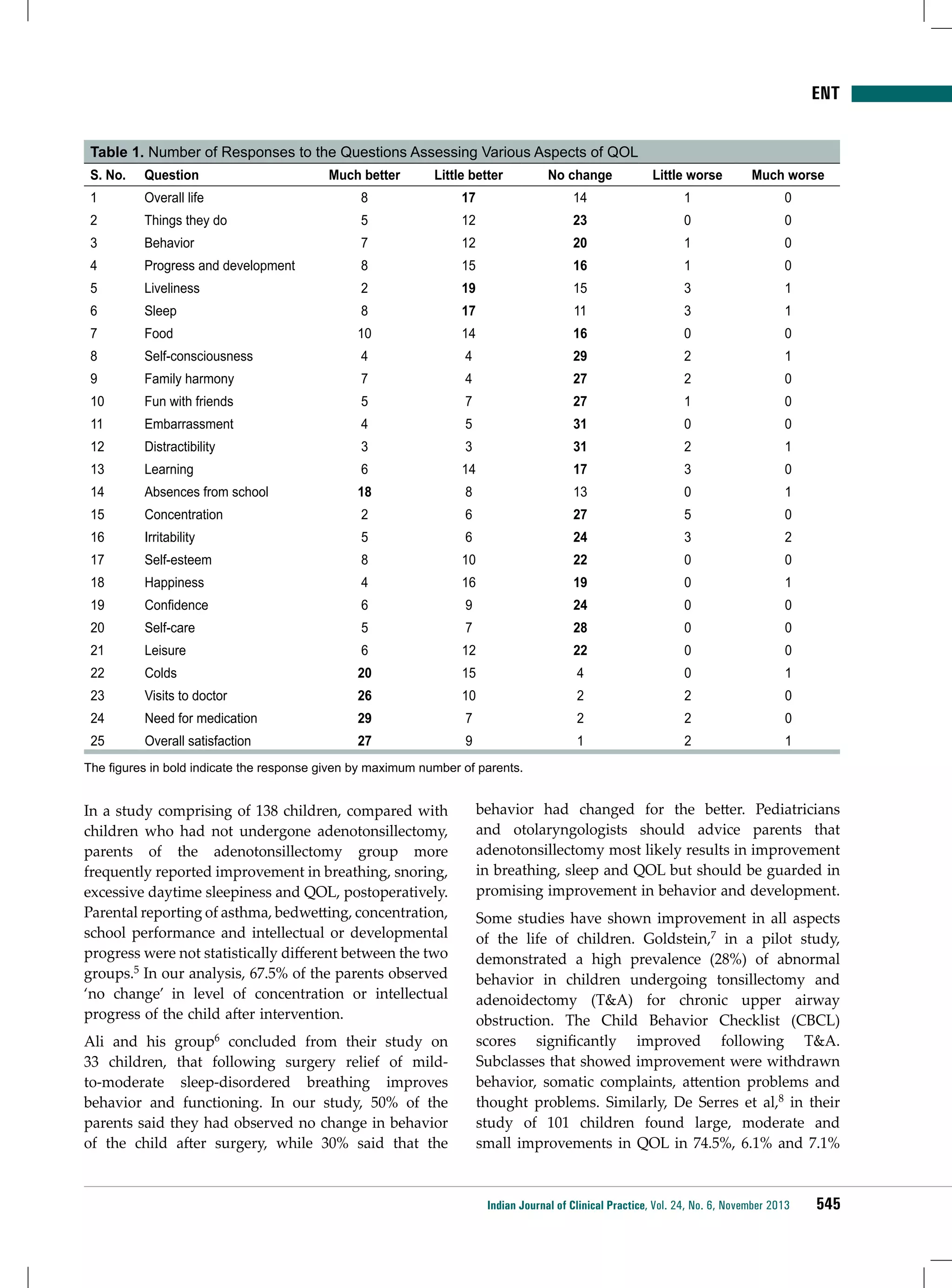
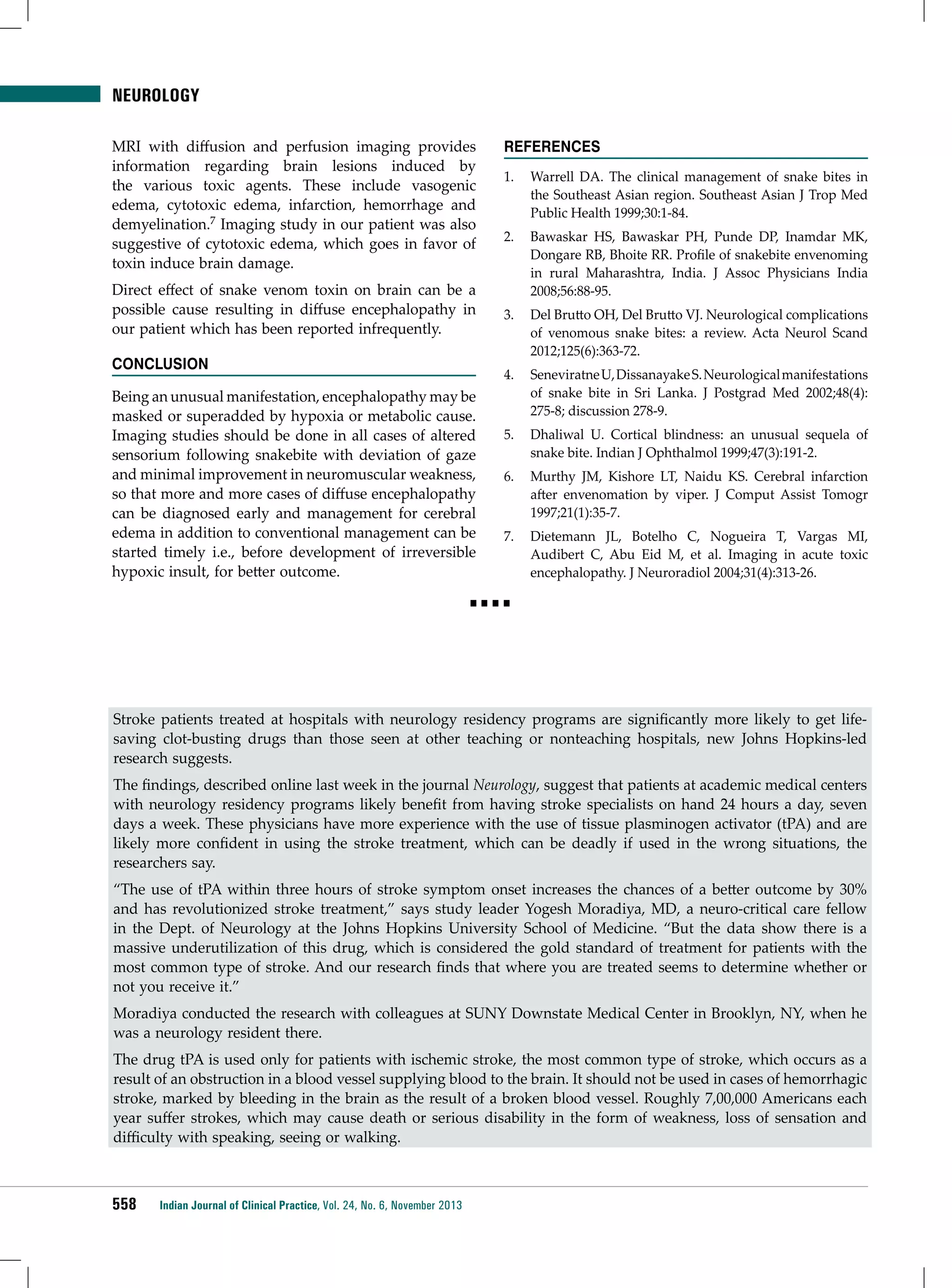
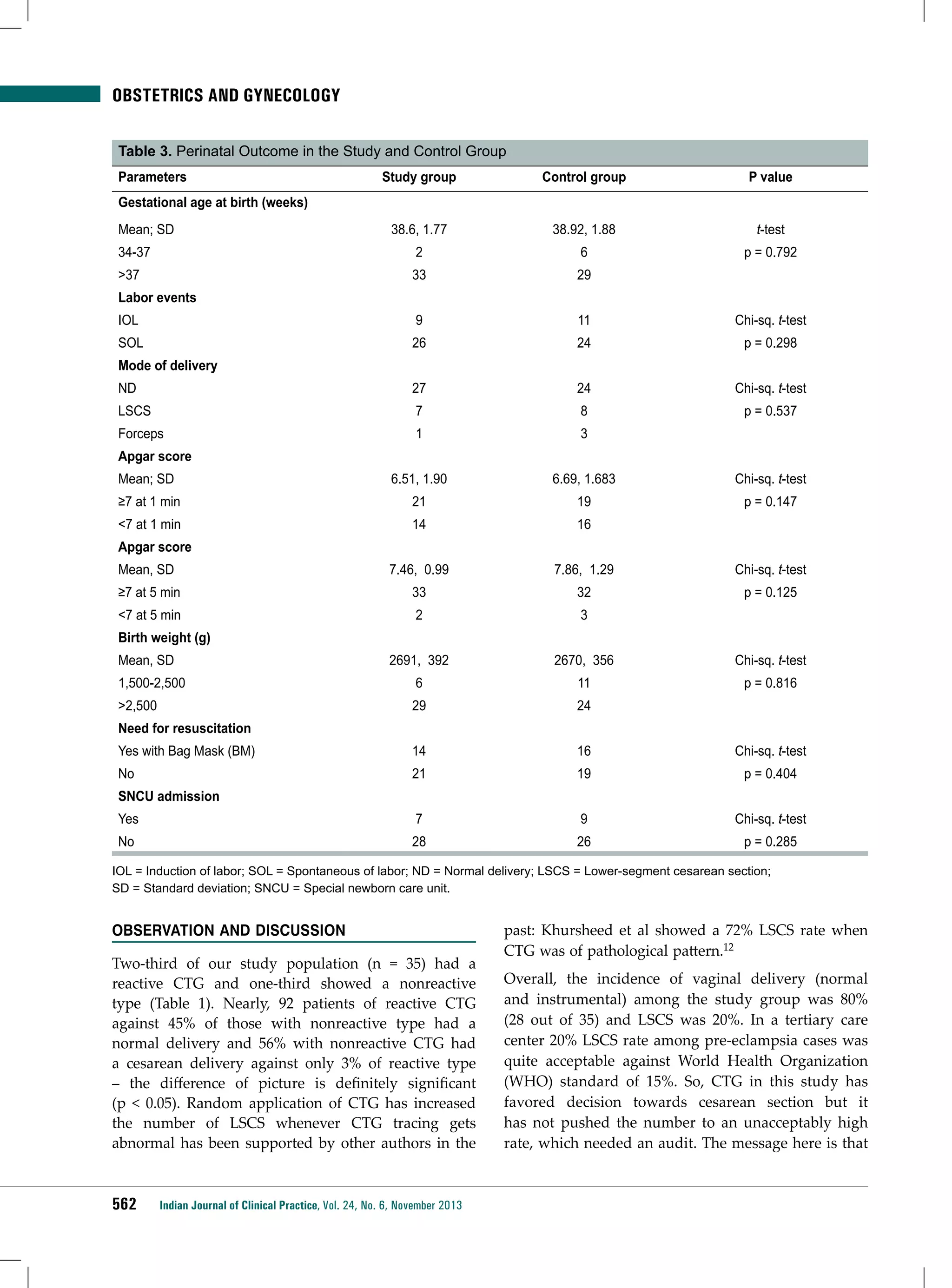
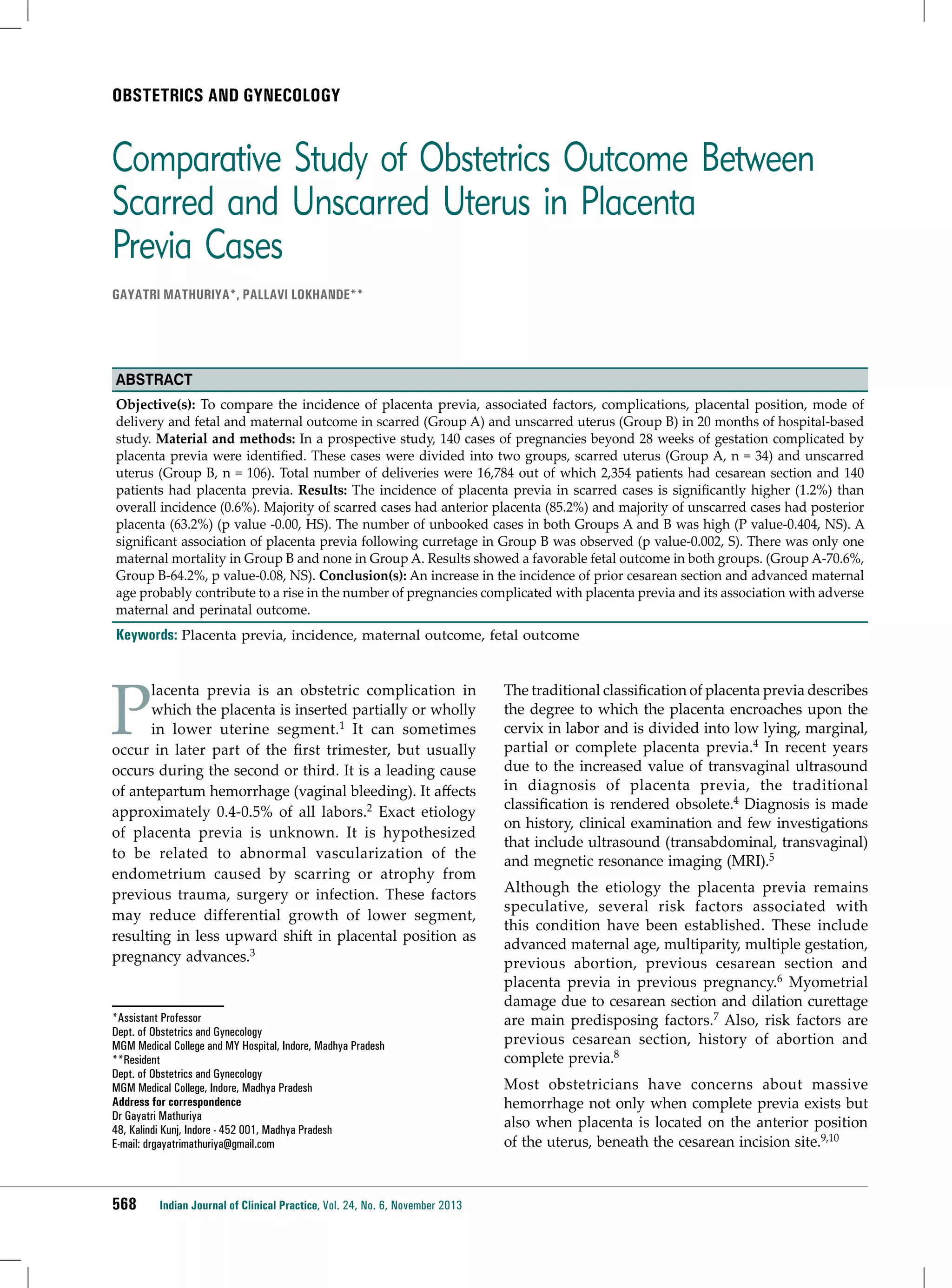
![American Family Physician
Table 1. Vaccines for the 2013-2014 Influenza Season (continued)
Vaccine
Dispensing method
Mercury
content (mcg
per 0.5-mL
dose)
Ovalbumin
content (mcg
per 0.5-mL
dose)
Approved
ages
Route of
administration
0
—
≥ 65 years
Intramuscular†
Inactivated influenza vaccine, trivalent, high dose
Fluzone High-Dose** 0.5-mL single-dose prefilled syringe
Inactivated influenza vaccine, quadrivalent, standard dose
Fluarix quadrivalent
0.5-mL single-dose prefilled syringe
0
≤ 0.05
≥ 3 years
Intramuscular†
Flulaval quadrivalent
5.0-mL multidose vial
< 25.0
≤ 0.3
≥ 3 years
Intramuscular†
0
—
6 to 35 months
Intramuscular†
0.5-mL single-dose prefilled syringe
0
—
≥ 36 months
Intramuscular†
0.5-mL single-dose vial
0
—
≥ 36 months
Intramuscular†
0
0
18 to 49 years
Intramuscular†
0 (per 0.2-mL
dose)
< 0.24 (per 0.2mL dose)
2 to 49 years‡‡
Intranasal
Fluzone quadrivalent 0.25-mL single-dose prefilled syringe
Recombinant influenza vaccine, trivalent
Flublok
0.5-mL single-dose vial
Live attenuated influenza vaccine, quadrivalent
Flumist
quadrivalent††
0.2-mL single-dose prefilled
intranasal sprayer
Note: Immunization providers should check U.S. Food and Drug Administration–approved prescribing information for 2013-2014 influenza vaccines for
the most complete and updated information, including (but not limited to) indications, contraindications, and precautions. Package inserts for U.S.licensed vaccines are available at http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm093833.htm.
*Age indication per package insert is 5 years or older; however, the Advisory Committee on Immunization Practices recommends that Afluria not be used
in children 6 months to 8 years of age because of increased risk of febrile reactions noted in this age group with 2010 Southern Hemisphere trivalent
inactivated vaccine. If no other age-appropriate, licensed inactivated seasonal influenza vaccine is available for a child 5 to 8 years of age who has a medical
condition that increases the child’s risk of influenza complications, Afluria can be used; however, health care professionals should discuss with the parents
or caregivers the benefits and risks of influenza vaccination with Afluria before administering this vaccine. Afluria may be used in persons 9 years or older.
†For adults and older children, the recommended site of vaccination is the deltoid muscle. The preferred site for infants and young children is the anterolateral
aspect of the thigh. Specific guidance regarding site and needle length for intramuscular administration may be found in the Advisory Committee on
Immunization Practices General Recommendations on Immunization (Centers for Disease Control and Prevention. General recommendations on immunization:
recommendations of the Advisory Committee on Immunization Practices, 2011. MMWR. 2011;60[RR-2].).
‡Information not included in package insert. The total egg protein is estimated to be less than 50 femtograms (5 × 1014 g) total egg protein (of which a
fraction is ovalbumin) per 0.5-mL dose of Flucelvax.
§Available on request from Sanofi Pasteur (1-800-822-2463 or MIS.Emails@sanofipasteur.com).
||Inactivated influenza vaccine, intradermal: a 0.1-mL dose contains 9 mcg of each vaccine antigen (27 mcg total).
¶The preferred site is over the deltoid muscle. Fluzone intradermal is administered using the delivery system included with the vaccine.
**Inactivated influenza vaccine, high dose: a 0.5-mL dose contains 60 mcg of each vaccine antigen (180 mcg total).
††It is anticipated that the quadrivalent formulation of Flumist will replace the trivalent formulation for the 2013-2014 season. Flumist is shipped refrigerated
and stored in the refrigerator at 35°F to 46°F (2°C to 8°C) after arrival in the vaccination clinic. The dose is 0.2 mL divided equally between each nostril.
Health care professionals should consult the medical record, when available, to identify children 2 to 4 years of age with asthma or recurrent wheezing that
might indicate asthma. In addition, to identify children who might be at greater risk of asthma and possibly at increased risk of wheezing after receiving live
attenuated influenza vaccine, parents or caregivers of children 2 to 4 years of age should be asked, “In the past 12 months, has a health care professional
ever told you that your child had wheezing or asthma?” Children whose parents or caregivers answer “yes” to this question and children who have asthma
or who had a wheezing episode noted in the medical record within the past 12 months should not receive Flumist.
‡‡Flumist is indicated for healthy, nonpregnant persons 2 to 49 years of age. Persons who care for severely immunosuppressed persons who require a
protective environment should not receive Flumist given the theoretical risk of transmission of the live attenuated vaccine virus.
Dose) is approved for persons 65 years or older. Three
prelicensure studies among persons in this age group
showed that, compared with the standard dose, the
high-dose vaccine elicited higher hemagglutination
inhibition antibody titers against the three virus strains
included in the seasonal influenza vaccine during the
study period. However, there is no recommendation
for using the high-dose vaccine vs. the standard-dose
vaccine in this population.
Persons 18 to 49 years of age who have an egg allergy of
any severity now have the option of receiving trivalent
recombinant influenza vaccine, an egg-free vaccine. In
persons who have no known history of egg exposure
but who have received allergy test results suggestive of
an egg allergy, consultation with a physician who has
expertise in allergy management is recommended before
vaccination. Figure 1 provides an algorithm for influenza
vaccination in persons who report an allergy to eggs.
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
517](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-17-2048.jpg)


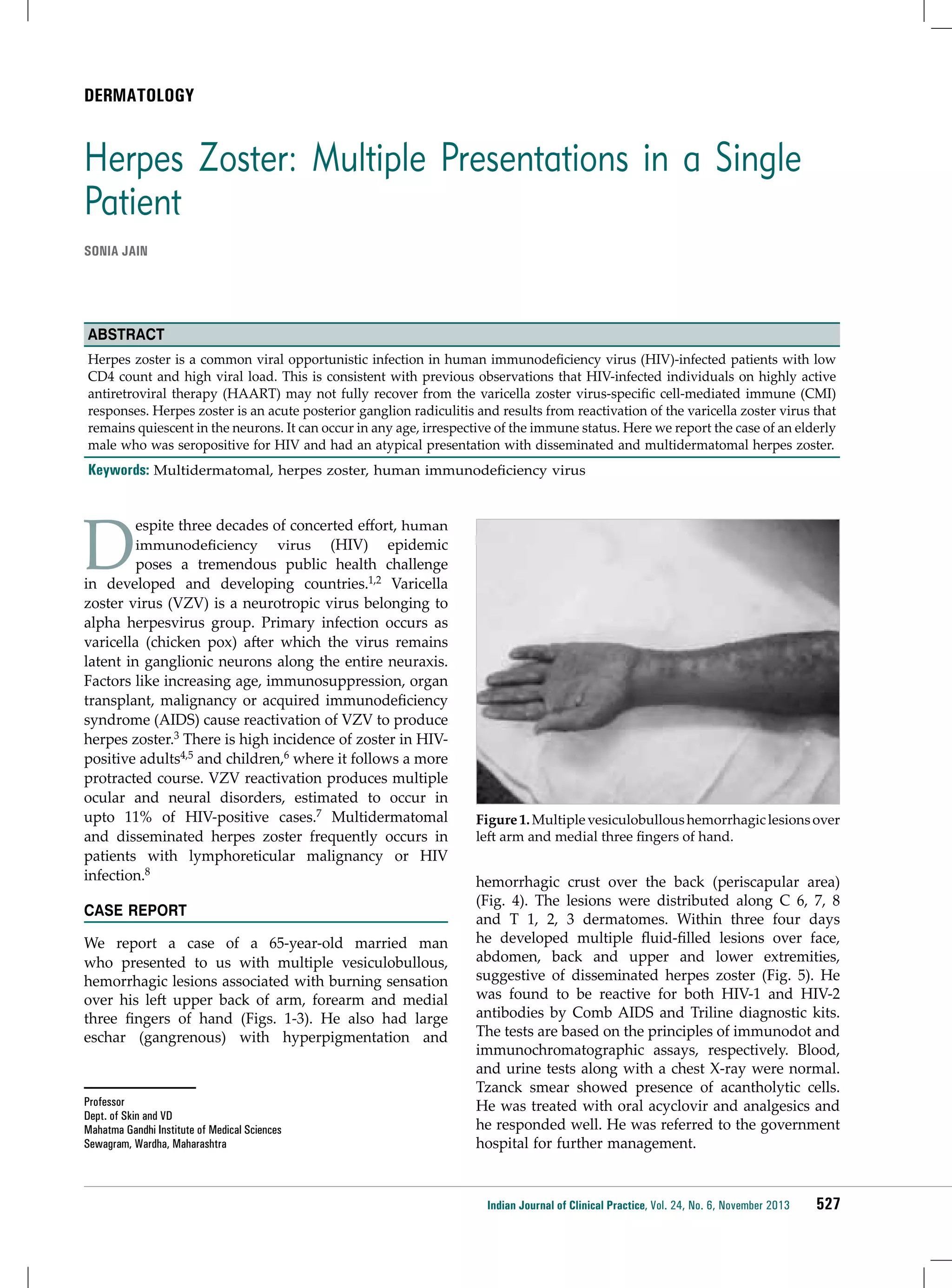
![DENTISTRY
ÂÂ
Inhibition of specific organisms
Inhibition of pathogen adhesion, colonization and
biofilm formation
Inhibition of pathogen growth by various substances
such as organic acids, hydrogen peroxide and
bacteriocins against oral pathogens
Effects on host response
Inhibition of collagenases and reduction of
inflammation-associated molecules
Induction of expression of cytoprotective proteins
on host cell surfaces
Modulation of proinflammatory pathways induced
by pathogens
Prevention of cytokine-induced apoptosis
ÂÂ
Modulation of host immune response
ÂÂ
ÂÂ
ÂÂ
ÂÂ
ÂÂ
ÂÂ
ÂÂ
Probiotics: Role in prevention of
periodontal disease
Various studies have reported the capacity of lactobacilli
to inhibit the growth of periodontopathogens,
including P. gingivalis, Prevotella intermedia and
A. actinomycetemcomitans.10,11
Krasse and colleagues12 assessed the beneficial effect
of L. reuteri against gingivitis. First, L. reuteri is known
for its secretion of two bacteriocins, reuterin and
reutericyclin, that inhibit the growth of a wide variety
of pathogens;13,14 second, L. reuteri has a strong capacity
to adhere to host tissues, thereby competing with
pathogenic bacteria.15
periodontitis.19 Hojo et al suggested that Bifidobacterium
inhibited some black-pigmented anaerobes by
competing for an essential growth factor vitamin K.20
Shimauchi et al demonstrated that the oral
administration of a tablet containing L. salivarius
WB21 decreased plaque index significantly and pocket
probing depth markedly in smokers and reduced
salivary lactoferrin at the end of 8-week trial.21
Twetman et al used L. reuteri-containing chewing gum in
42 healthy patients and assessed its effects on crevicular
fluid volume, cytokine (interleukin-1β, interleukin-6,
interleukin-10 and tumor necrosis factor-α [TNF-α])
levels and bleeding on probing. Crevicular fluid
volume, as well as TNF-α and interleukin-8 levels and
bleeding were significantly reduced.22
When the probiotic Streptococcus salivarius K12 was
added to this bacterial model, the amount of cytokine
release was greatly reduced after eight hours. This
strongly suggests that S. salivarius K12 was able to
dramatically downregulate the cytokine release from
the pathogenic bacteria.23
Probiotics and Halitosis
Kang and colleagues24 reported the capacity of various
strains of W. cibaria to inhibit the production of volatile
sulfur compounds by F. nucleatum. They concluded
that this beneficial effect resulted from the production
of hydrogen peroxide by W. cibaria, which inhibited the
proliferation of F. nucleatum.24
Staab et al observed reduction in activity of matrix
metalloprotein-3 (MMP-3) and elastase enzymes in
subjects with plaque-induced gingivitis after consuming
probiotic milk containing Lactobacillus casei species for a
period of eight weeks.16
Currently Available Probiotic Agents in
Periodontal Disease Management
Riccia et al studied the anti-inflammatory effects of
Lactobacillus brevis in a group of patients with chronic
periodontitis. Anti-inflammatory effects of L. brevis
could be attributed to its capacity to prevent the
production of nitric oxide and consequently the release
of prostaglandin E2(PGE2) and the activation of MMPs
induced by nitric oxide.17
ÂÂ
Probiotics in the form of tablets, lozenges, chewing
gums or toothpastes are available:
Another probiotic lozenge is avaliable, which
is a blend of two L. reuteri strains containing a
minimum of 1 × 108 colony forming units (CFU)
for each of the strains DSM 17938 and ATCC PTA
5289.26
Ishikawa et al observed in vitro inhibition of P. gingivalis,
P. intermedia and P. nigrescens by daily ingestion of
L. salivarius in tablet form.18
Van Essche et al have reported that B. bacteriovorus
attack, prey on and kill A. actinomycetemcomitans,
thus suggesting a potential scope for the role of
B. bacteriovorus in the prevention and treatment of
Lozenges: One of the first probiotic specifically
formulated to fight periodontal disease, contained
a patented combination of two strains of L. reuteri
selected for their synergistic properties in fighting
cariogenic bacteria and periodontopathogens. Each
dose of lozenge contained at least 2 × 108 living
cells of L. reuteri Prodentis.25
ÂÂ
Toothpastes: Toothpastes containing Dental-Lac,
a functional Lactobacillus paracasei probiotic are
available.25
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
525](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-25-2048.jpg)


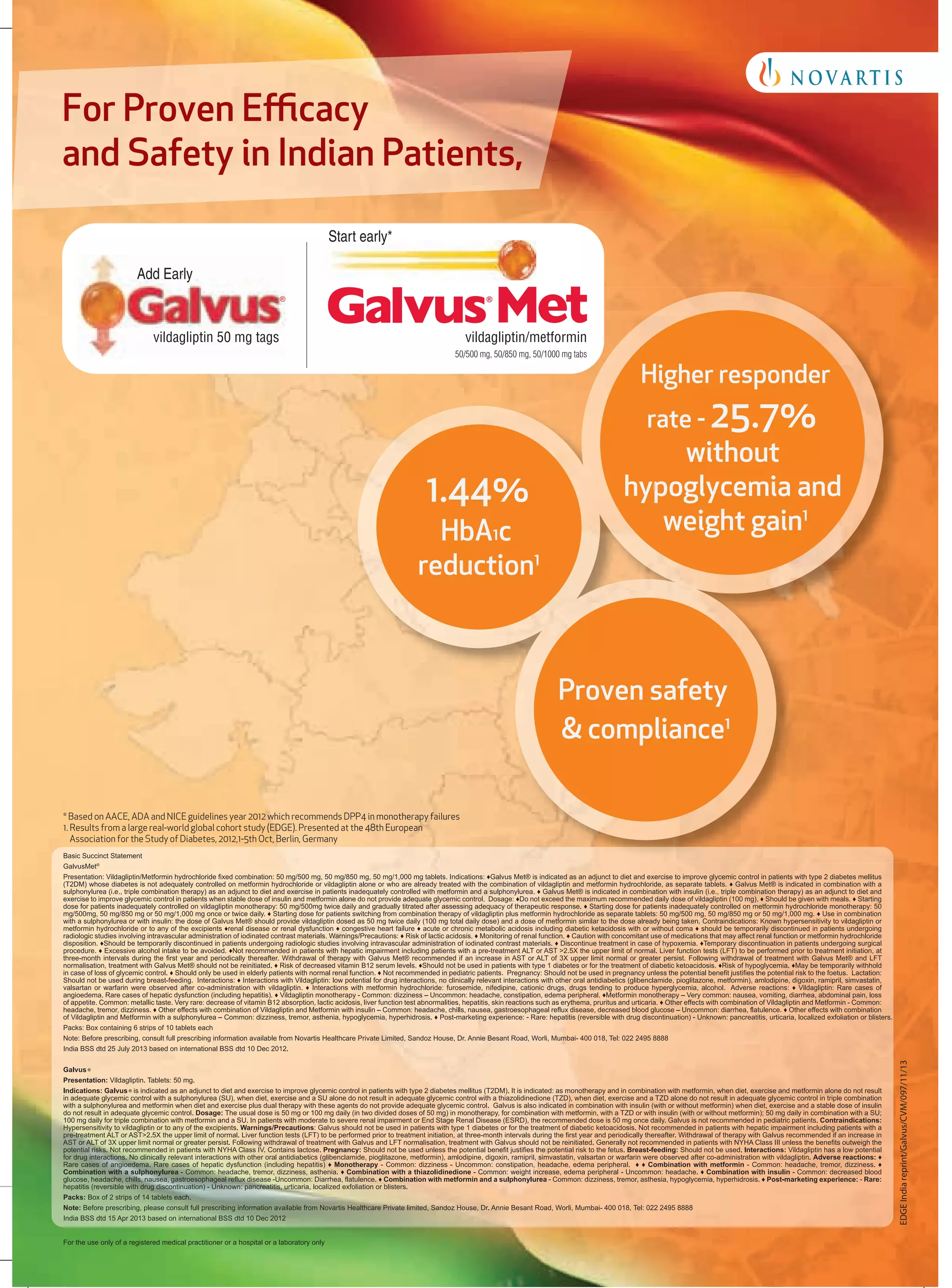
![ENDOCRINOLOGY
Effectiveness and Tolerability of Vildagliptin in Indian
Patients with Type 2 Diabetes Mellitus: Results From
Edge−A Real-World Observational Study
Subhash K Wangnoo*, Giovanni Bader**, Apurva Gawai†, Shradhanand Singh‡
Abstract
Objective: To assess the effectiveness and tolerability of vildagliptin in combination with another oral antidiabetic drug (OAD)
versus any other two-agent OAD combinations in Indian patients with type 2 diabetes mellitus (T2DM) in a real-world setting.
Study design: This was a post hoc analysis of a multicenter, prospective, 1-year, observational EDGE study for patients enrolled in
India. The primary efficacy endpoint of the study was proportion of patients achieving glycosylated hemoglobin (HbA1C) reduction
of >0.3% without peripheral edema, hypoglycemic event, discontinuation due to a gastrointestinal event or weight gain. One of the
secondary efficacy endpoints was proportion of patients achieving HbA1C <7% without hypoglycemia and weight gain. Results:
The mean age, body mass index, HbA1C and duration of T2DM were 51.8 years, 26.6 kg/m2, 8.6% and 4.3 years, respectively.
The proportion of patients achieving the efficacy endpoints was significantly higher in the vildagliptin cohort compared with the
comparator cohort (p < 0.0001). The vildagliptin cohort showed a numerically greater reduction in HbA1C than the comparator cohort
(1.4 vs 1.1%; analysis not pre-specified). Adverse events were comparable in both groups (4.2% vs 4.9%). Conclusion: In India, in
a real-world setting, vildagliptin showed better overall clinical benefits compared with comparator OADs in patients with T2DM.
Keywords: Dipeptidyl peptidase-4 inhibitor, dual combination, India, oral antidiabetic drug, real-world, type 2
diabetes, vildagliptin
T
ype 2 diabetes mellitus (T2DM), a major
lifestyle disorder, has transitioned from being
a class disease to a mass epidemic and poses a
rapidly emerging global threat to public health with
a worldwide prevalence of 366 million.1 India, once
known as the ‘diabetes capital of the world’2, was home
to 61.3 million patients with T2DM in 2011 and this
figure is expected to rise to 101.2 million by 2030.1
Various phenotypic and genotypic characteristics in
Indians may lead to increased insulin resistance, lower
*Senior Consultant Endocrinologist and Diabetologist
Apollo Centre for Obesity, Diabetes and Endocrinology (ACODE)
Indraprastha Apollo Hospital, Sarita Vihar, New Delhi
**Principal Medical Scientific Expert, Global Medical Affairs - Diabetes, Novartis
Pharma AG, Postfach, Switzerland
†Medical Advisor
Novartis Healthcare Private Limited, Worli, Mumbai
‡Clinical Research Medical Advisor
Novartis Healthcare Private Limited, Worli, Mumbai
Address for correspondence
Dr Apurva Gawai
Medical Advisor
Novartis Healthcare Private Limited
Sandoz House, 7th Floor, Shivsagar Estate
Dr Annie Besant Road, Worli, Mumbai - 400 018
E-mail: apurva.gawai@novartis.com
adiponectin, greater abdominal adiposity (higher
waist circumference despite lower body mass index
[BMI]) and a higher prevalence of impaired glucose
tolerance; all of these factors contribute to a higher
risk of developing T2DM at a comparatively young
age.3 Physical inactivity, changes in dietary habits, a
carbohydrate rich diet, urbanization and environmental
factors also add to this risk.4 In addition, patients and
healthcare professionals in India face challenges such
as clinical inertia (failure to initiate or intensify the
treatment) in achieving glycemic control, inadequate
treatment follow-up and lack of disease awareness
among patients.4
Guidelines suggest the use of combination therapies
including diverse oral antidiabetic drugs (OADs),
acting via multiple mechanisms, to effectively manage
hyperglycemia, while dealing with the challenges of the
progressive nature of T2DM and monotherapy failure.5
Vildagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor
improves pancreatic α- and β-cell responsiveness
to glucose, and consequently provides improved
glycemic control as monotherapy, or as a component
of combination therapy, without weight gain and
hypoglycemia.6-8
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
537](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-37-2048.jpg)
![ENDOCRINOLOGY
Pragmatic real-world observational studies are
designed to provide a closer look into routine clinical
practice.9 EDGE (Effectiveness of Diabetes control
with vildaGliptin and vildagliptin/mEtformin) was
a prospective, 1-year, observational study conducted
across 27 countries from Europe, Central and Latin
America, Asia and Middle East to evaluate the efficacy,
safety and tolerability of vildagliptin in combination
with another OAD versus all other two-agent OAD
combinations in real-world settings.10 In these post hoc
analyses, we assessed the effectiveness and tolerability
of vildagliptin combination versus all other two-agent
OAD combinations in patients enrolled from India in
the EDGE study.
Subjects and Study Design
Of the 45,868 patients enrolled in the EDGE study,10
11,057 were enrolled across 472 sites in India. Patients
with T2DM, aged ≥18 years, who had inadequate
glycemic control, while receiving OAD monotherapy
with a sulfonylurea (SU), metformin, thiazolidinedione,
glinide or α-glucosidase inhibitor were eligible. Patients
receiving DPP-4 inhibitors other than vildagliptin,
incretinmimetics/analogs or insulin, requiring three or
more OADs, or who had a history of hypersensitivity
to study drugs were excluded.
Physicians chose antidiabetic treatment for their
patients at their own discretion. To avoid physician
bias for a particular choice of treatment, patients were
asked for informed consent and enrolled in the study
only after the treatment decision was made (Fig. 1).
The term index therapy was used to represent the
combination treatment initiated at enrolment. Further
details of the subjects and study design are reported
elsewhere.10
Materials and Methods
Efficacy Endpoints
The primary efficacy endpoint of the study was the
proportion of patients responding to the treatment
(reduction in glycosylated hemoglobin [HbA1C] >.3%
from baseline to 12 months) with no intolerability
findings (peripheral edema, hypoglycemic event,
discontinuation due to a gastrointestinal event or
weight gain ≥5%). One of the secondary efficacy
endpoints was the proportion of patients with baseline
HbA1C ≥7% who achieved target HbA1C <7% without
hypoglycemia and weight gain ≥3%. Change in HbA1C
from baseline to study endpoint was also evaluated in
538
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
these post hoc analyses (an analysis not pre-specified in
the protocol). Hypoglycemia was defined as symptoms
suggestive of hypoglycemia that resolved promptly on
administration of oral carbohydrate (including mild
and severe events).
Statistical Analysis
Descriptive statistics were used for these post hoc
analyses. Inference is provided for primary and
secondary efficacy endpoints. The per protocol (PP:
Patients who completed the study without any major
protocol deviation) population was used for analyses
of the efficacy endpoints. Data were censored if
patients changed index therapy. The probability of
success was analyzed for the efficacy endpoints using
a binary logistic regression model to calculate odds
ratios (ORs) with 95% confidence intervals (CIs). The
OR expresses odds in favor of success with vildagliptin
combinations relative to odds in favor of success with
comparator OADs. Patients whose outcomes could
not be categorized as a success or failure (e.g., due to
missing HbA1C or body weight data at the 12-month
endpoint) were considered nonevaluable. These nonevaluable patient data were considered failures in
calculation of the OR for success. Only unadjusted ORs
were reported for the primary and secondary efficacy
endpoints in these post hoc analyses. HbA1C drop was
adjusted with baseline value by using an analysis of
covariance (ANCOVA) model.
Results
Of the 11,057 patients enrolled from India in the
EDGE study, 365 patients (198 in the vildagliptin and
167 in the comparator cohort) were excluded due to
inadequate source documentation or problems with
quality or accuracy of data entry. The remaining
intention-to-treat (ITT) population received newly
prescribed vildagliptin (5,621) or a nonvildagliptin
OAD (5,071) added to prior monotherapy (Table 1).
The PP population, a subset of the ITT population
comprising 5,606 patients in the vildagliptin cohort
and 5,070 patients in the comparator cohort, was used
for the analyses of efficacy endpoints.
The demographic and baseline characteristics of
patients in the ITT population are summarized in
Table 2. Overall, 61.4% patients were male. The mean
values of age, BMI, HbA1C and duration of T2DM
at baseline were 51.8 years, 26.6 kg/m2, 8.6% and
4.3 years, respectively. Despite the fact that this was a
nonrandomized study, the baseline characteristics were
comparable across the groups (Table 2).](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-38-2048.jpg)
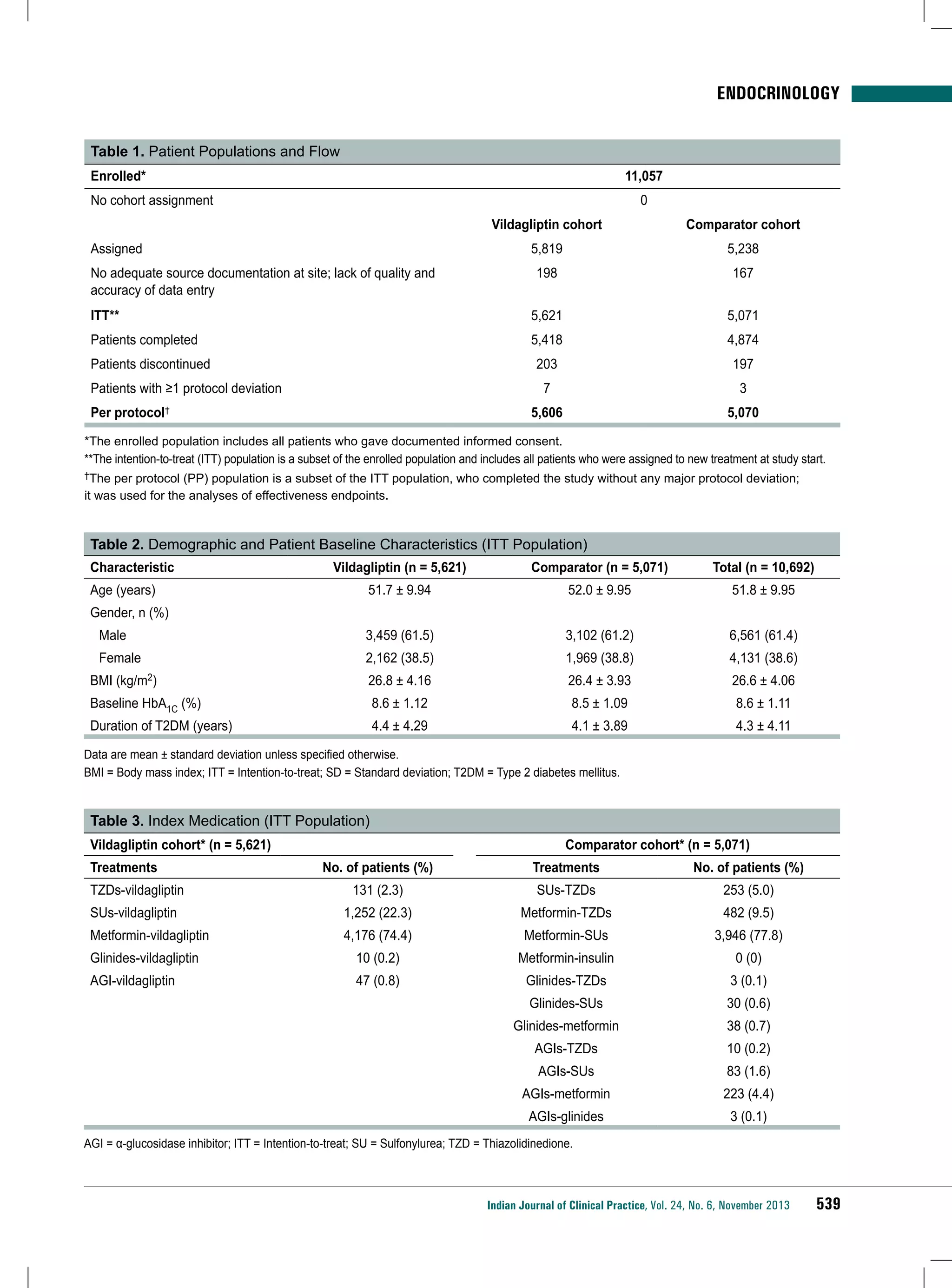
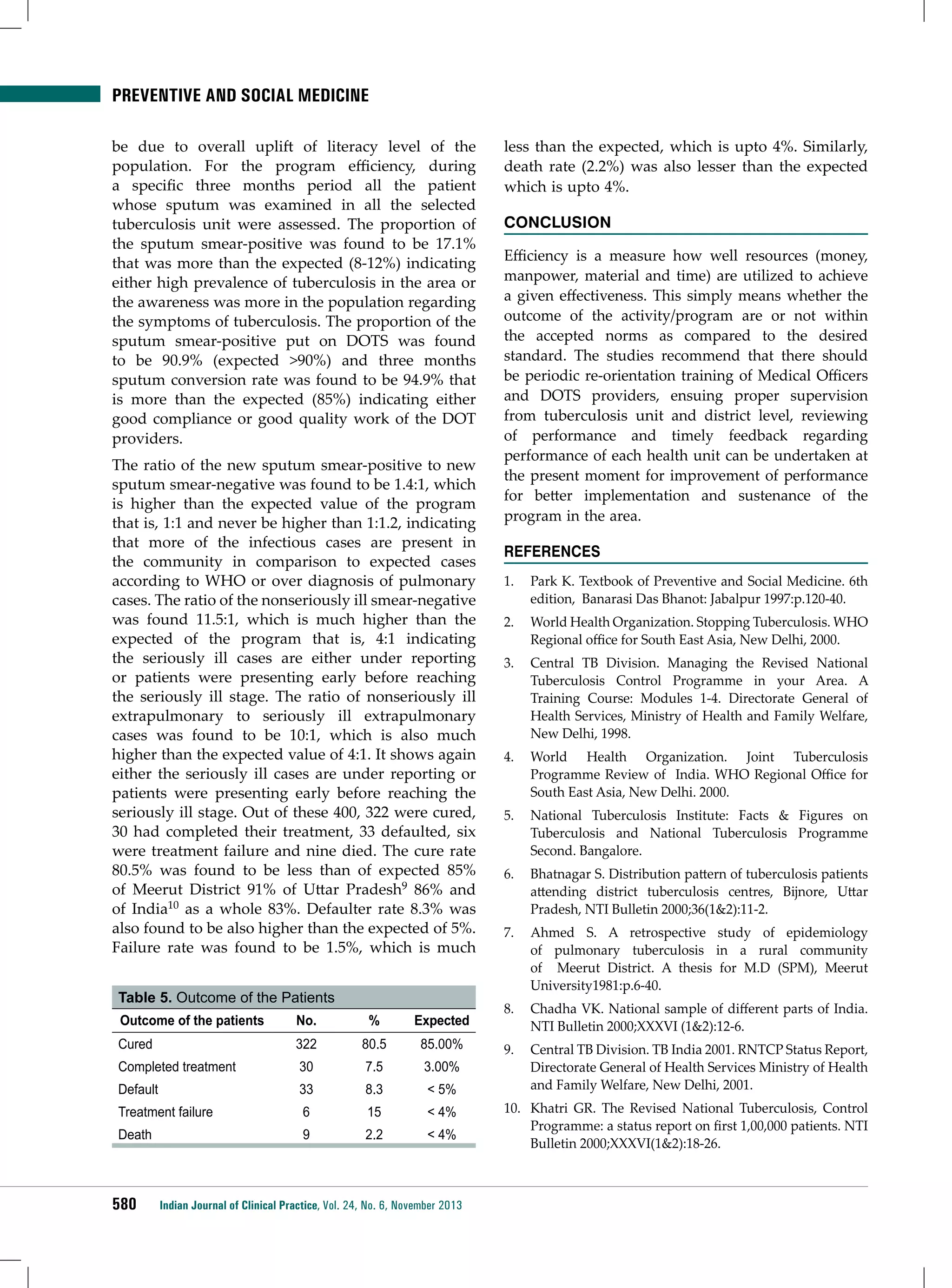
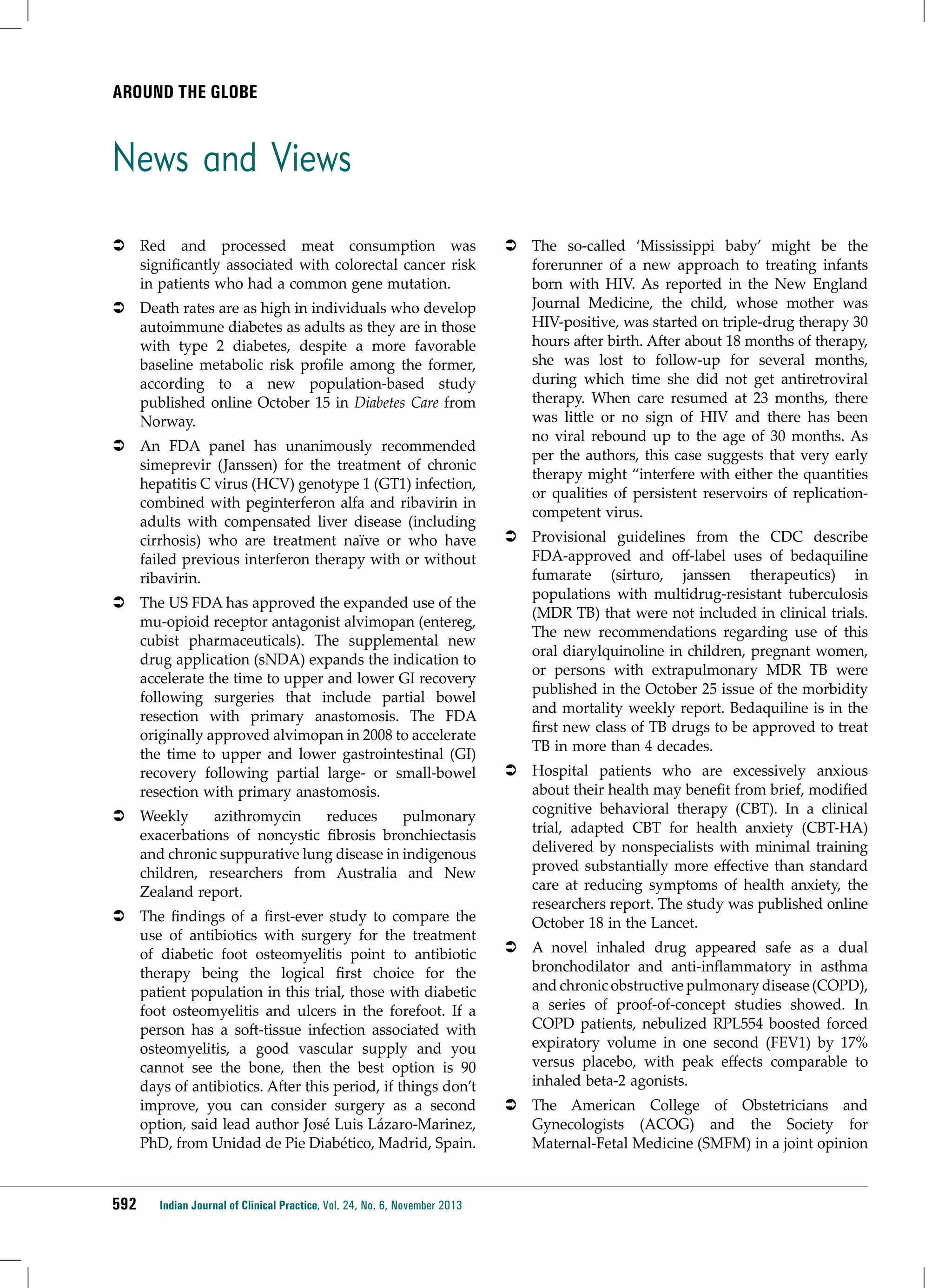
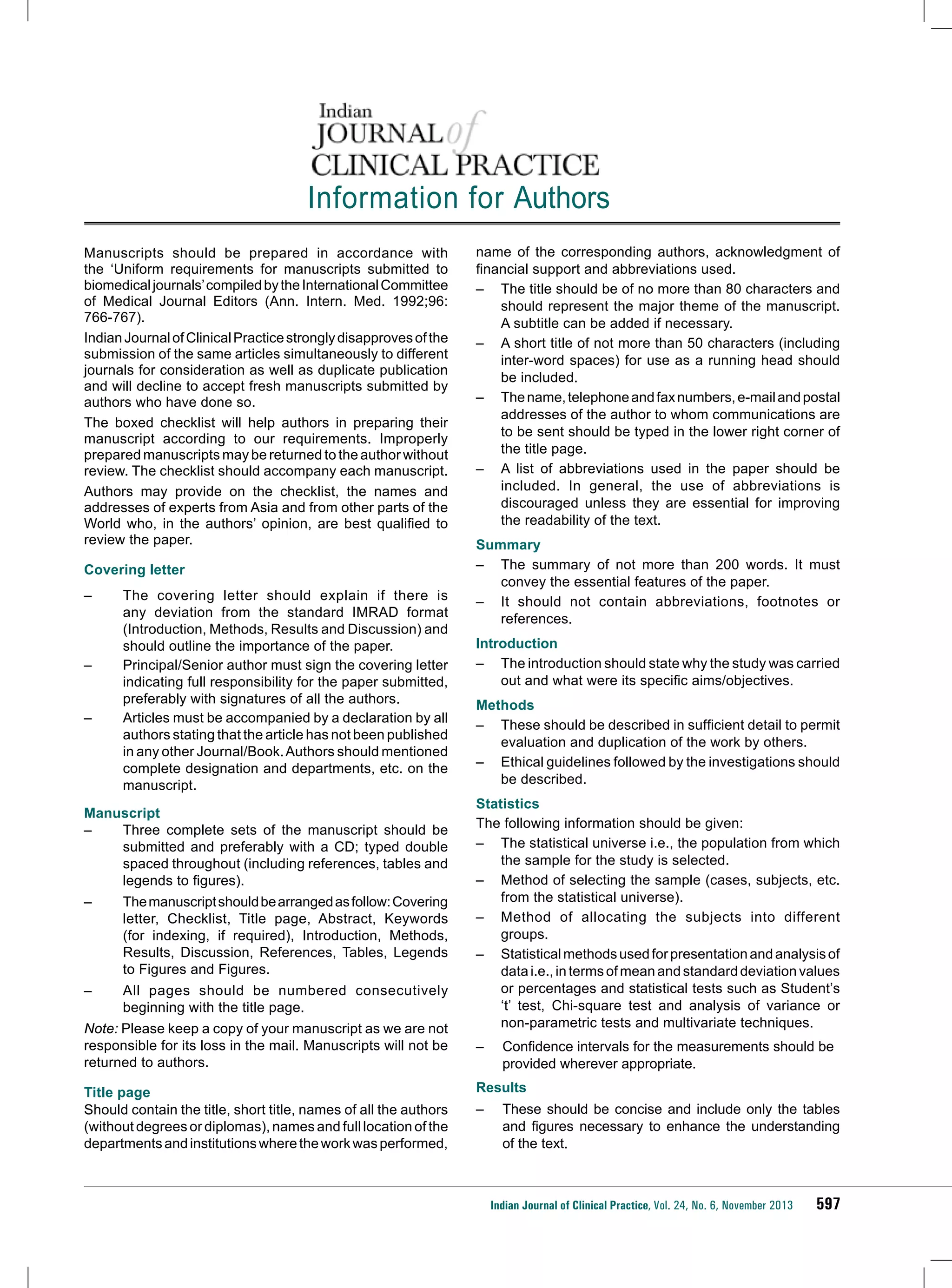
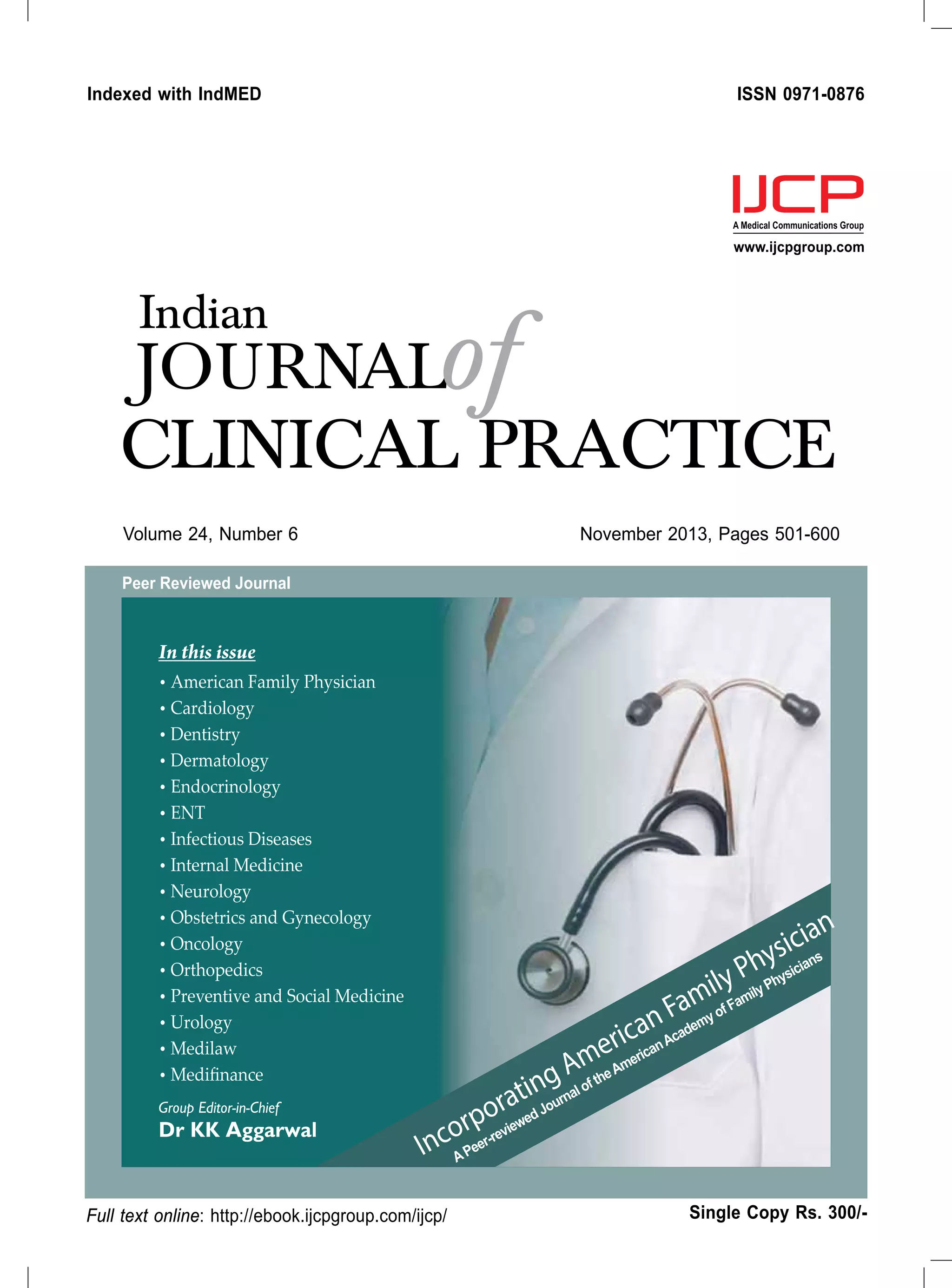
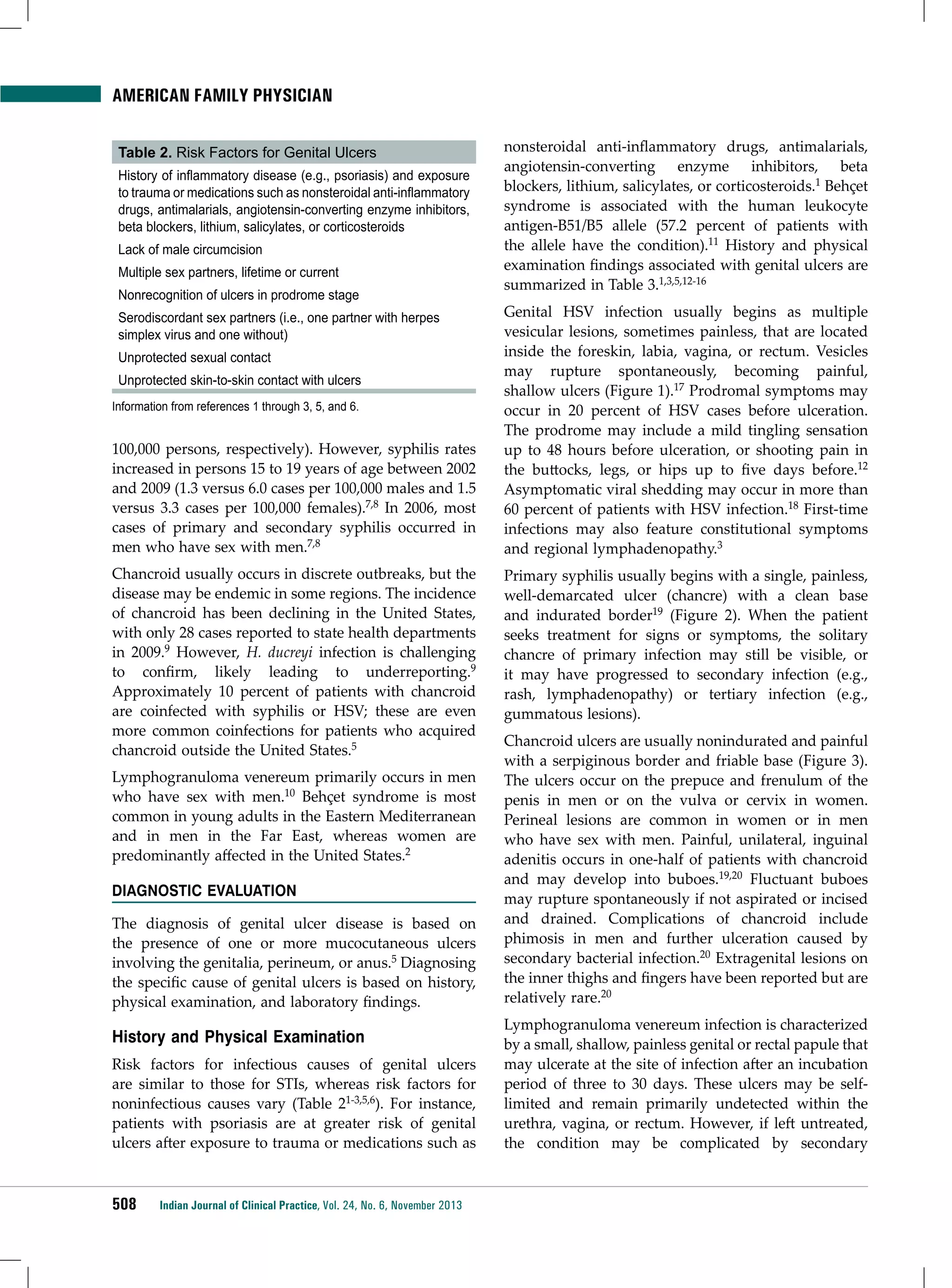
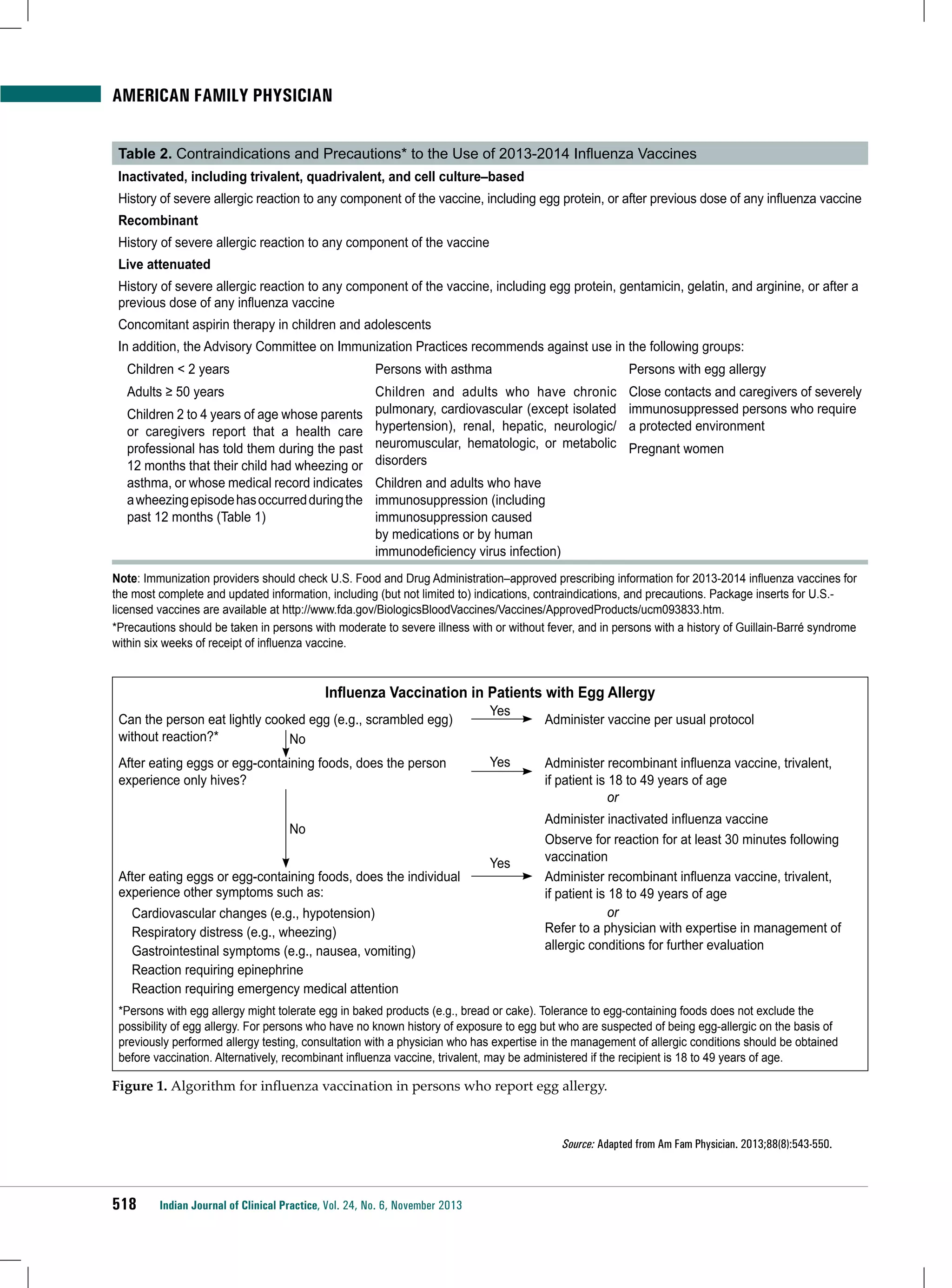
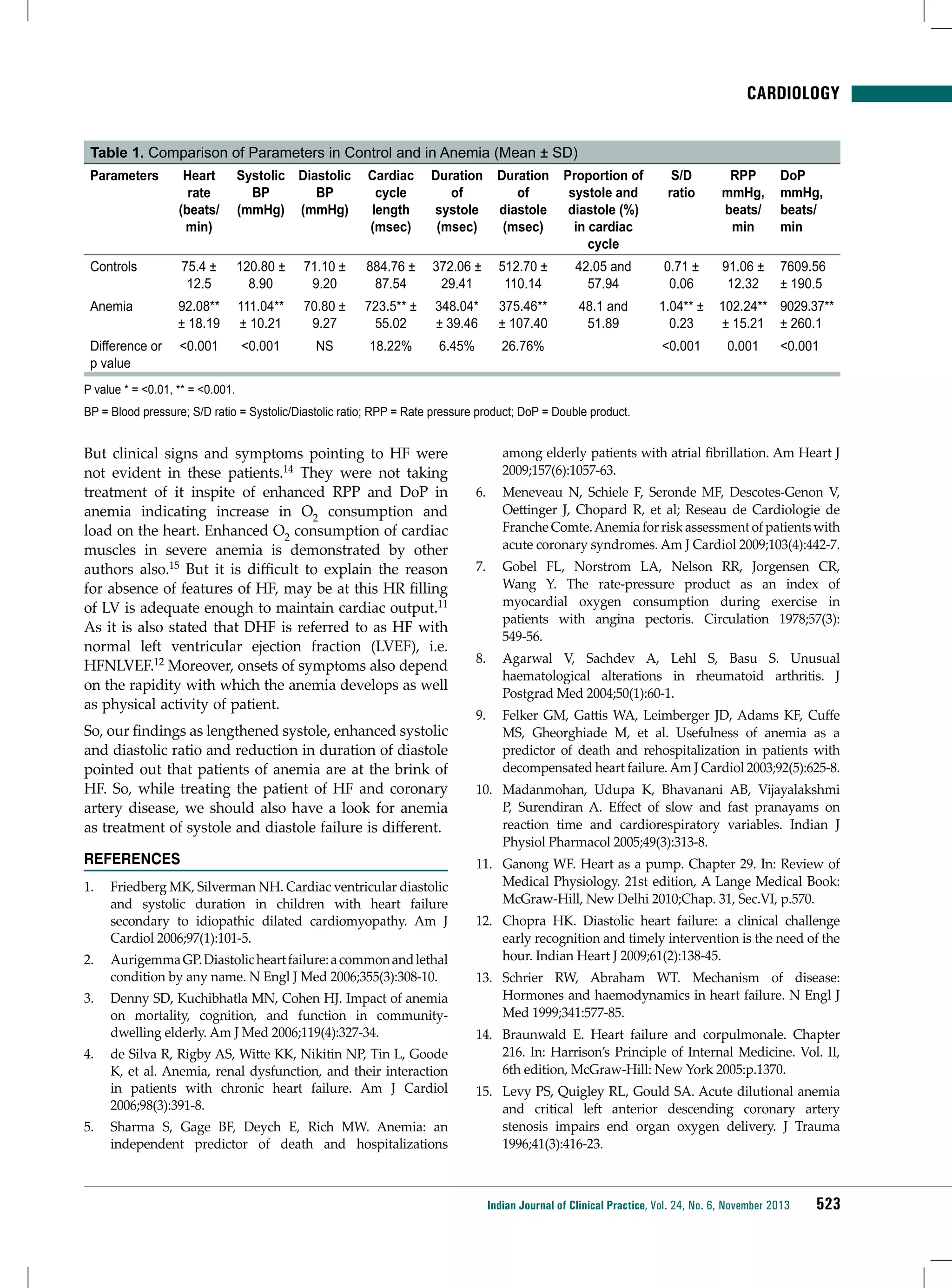
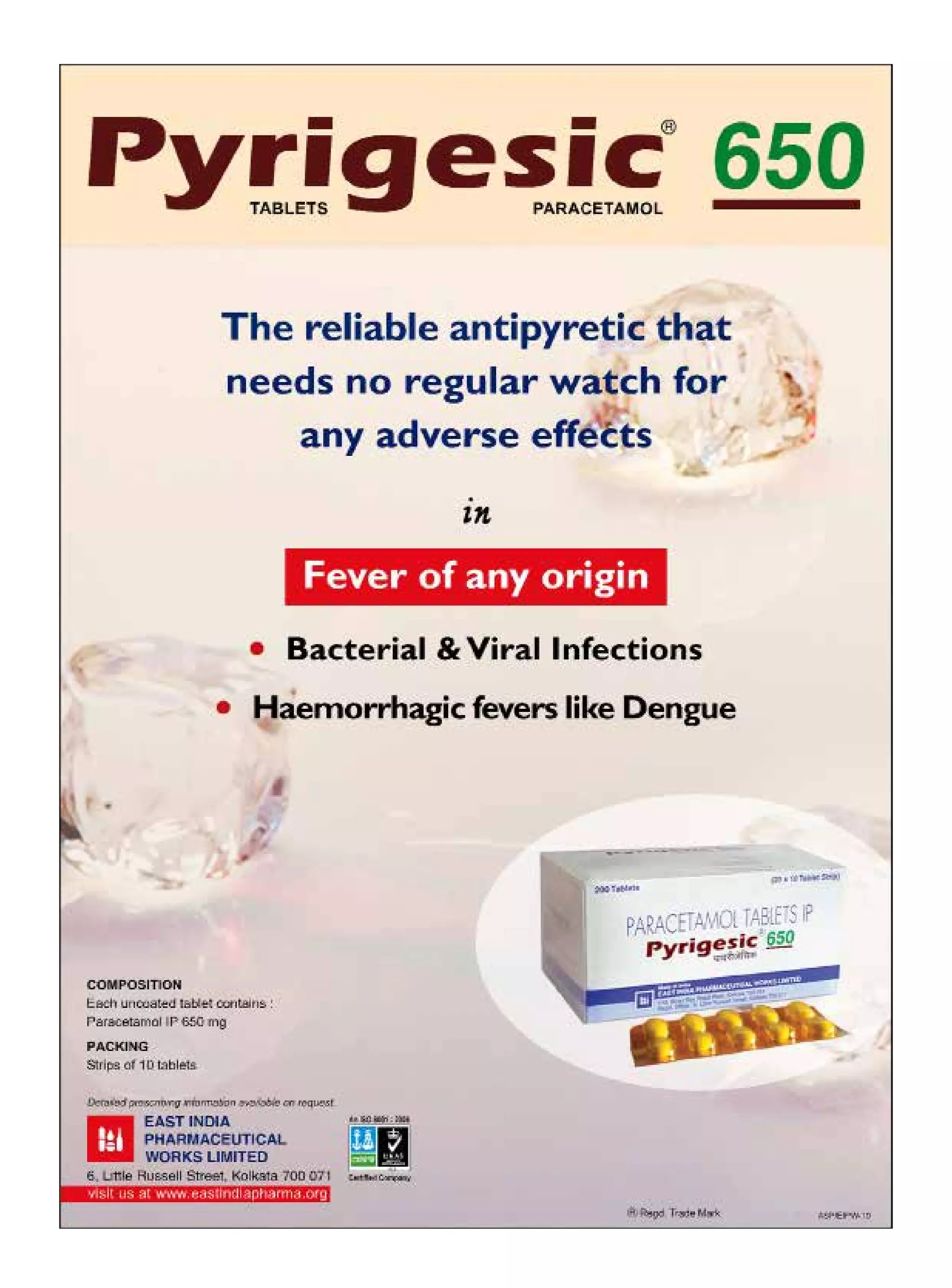
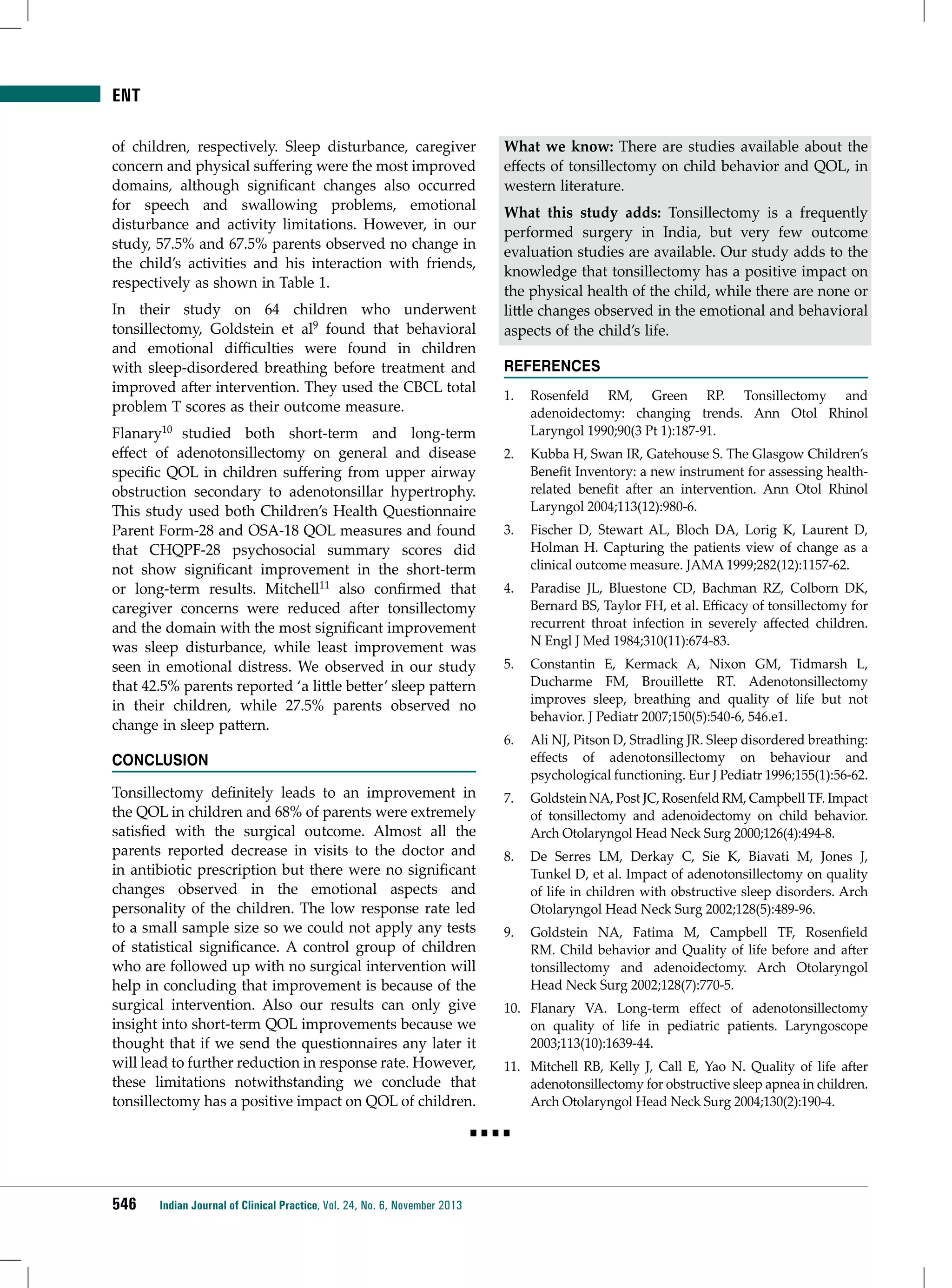
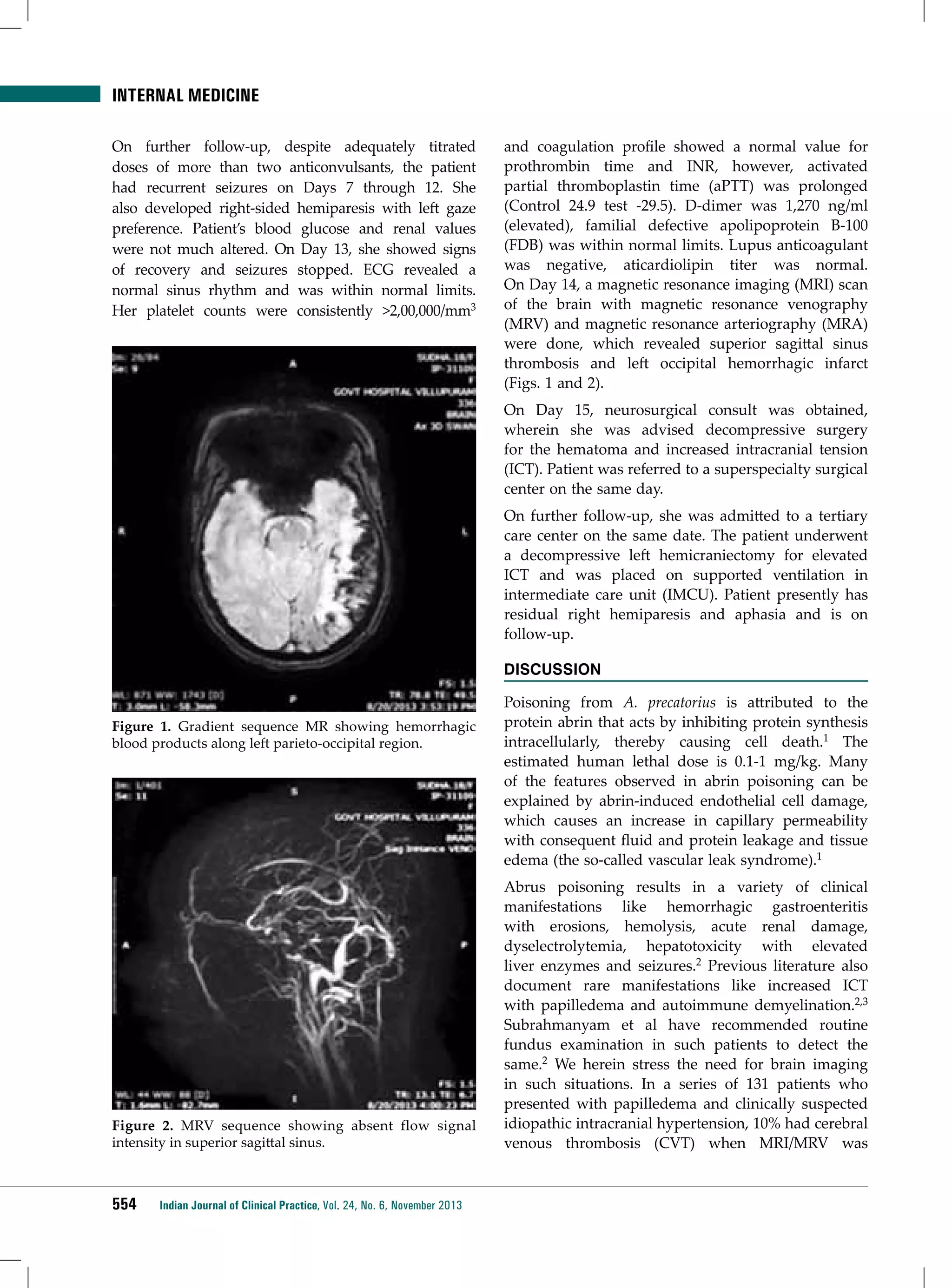
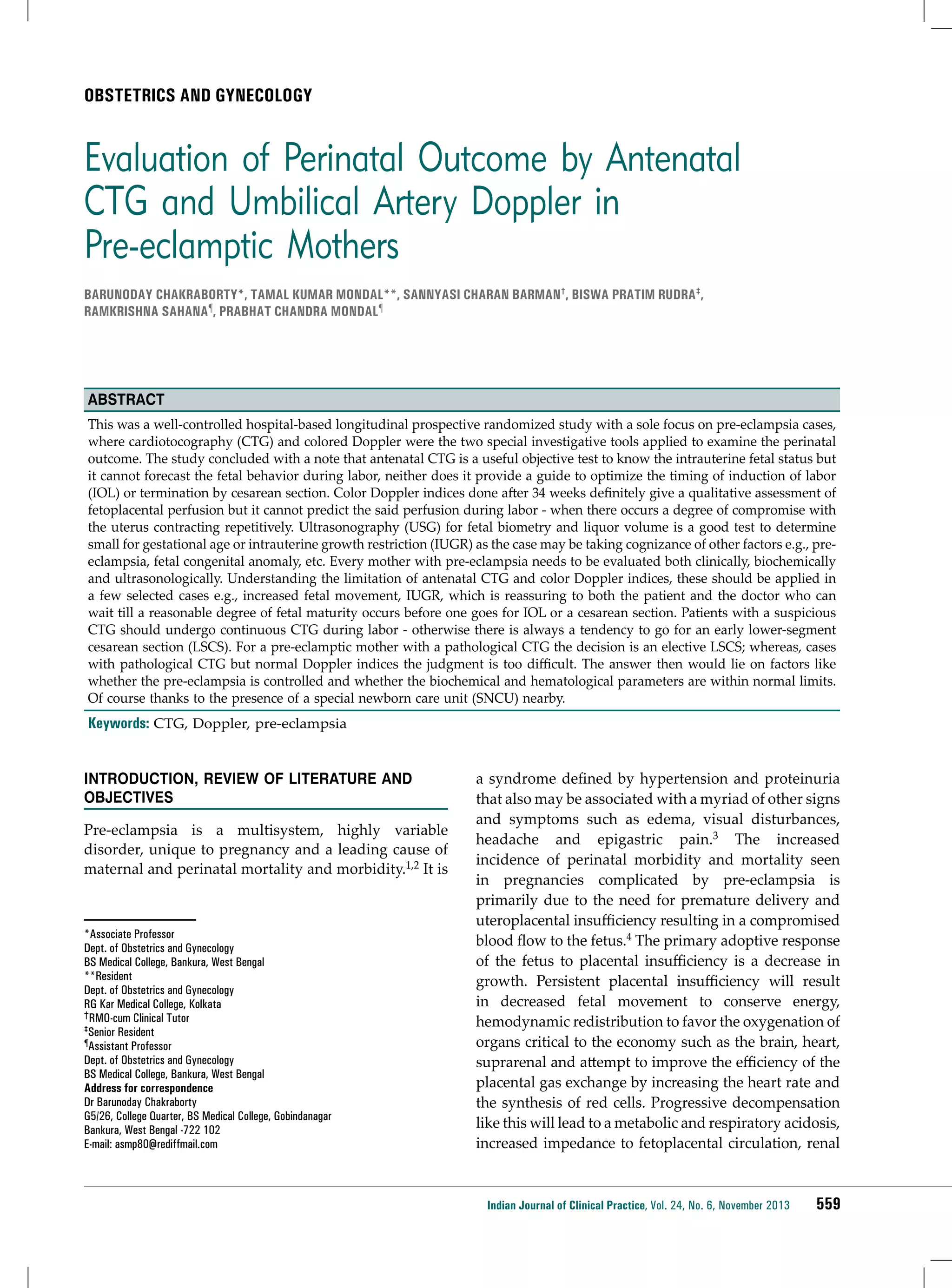
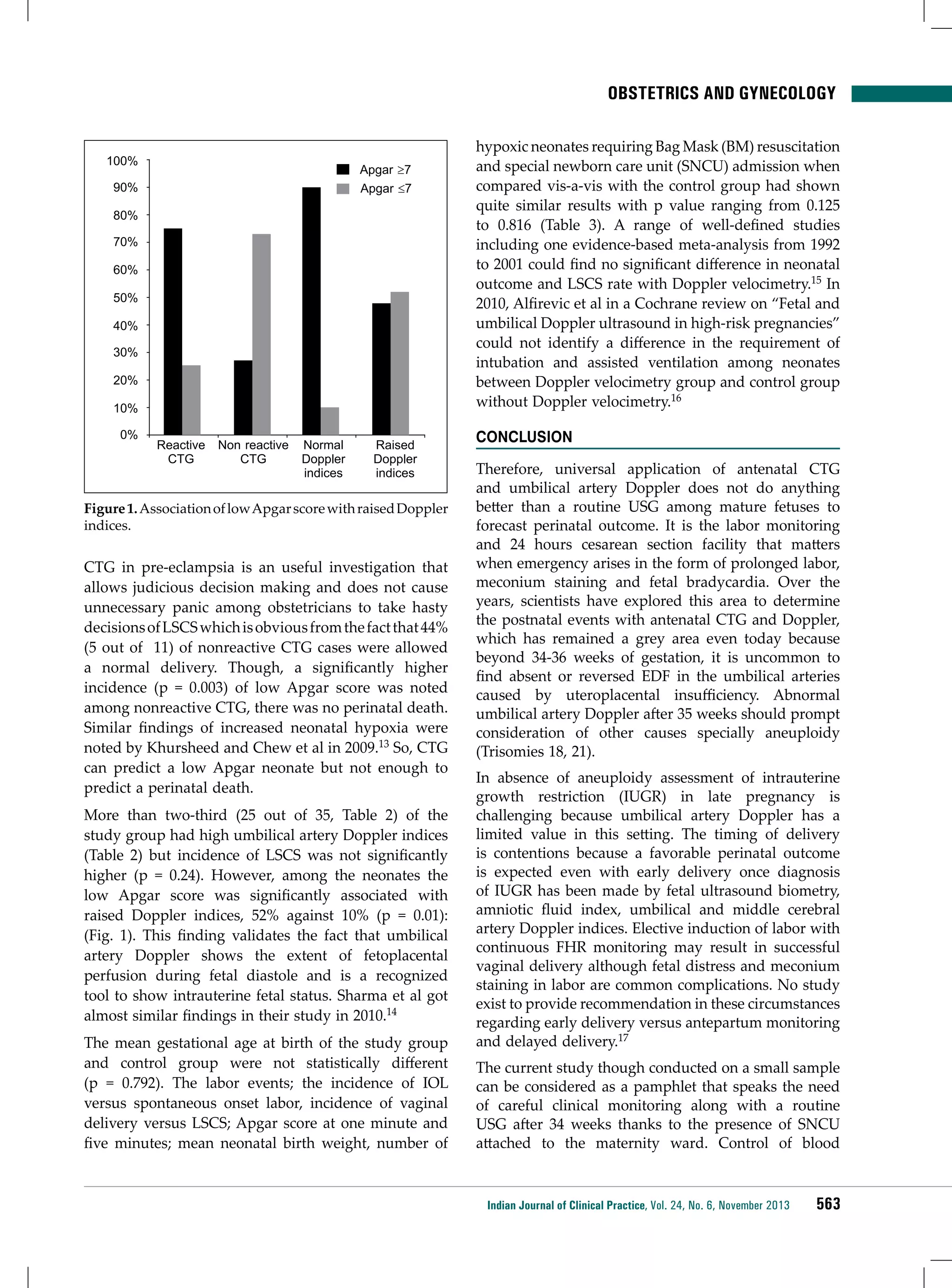
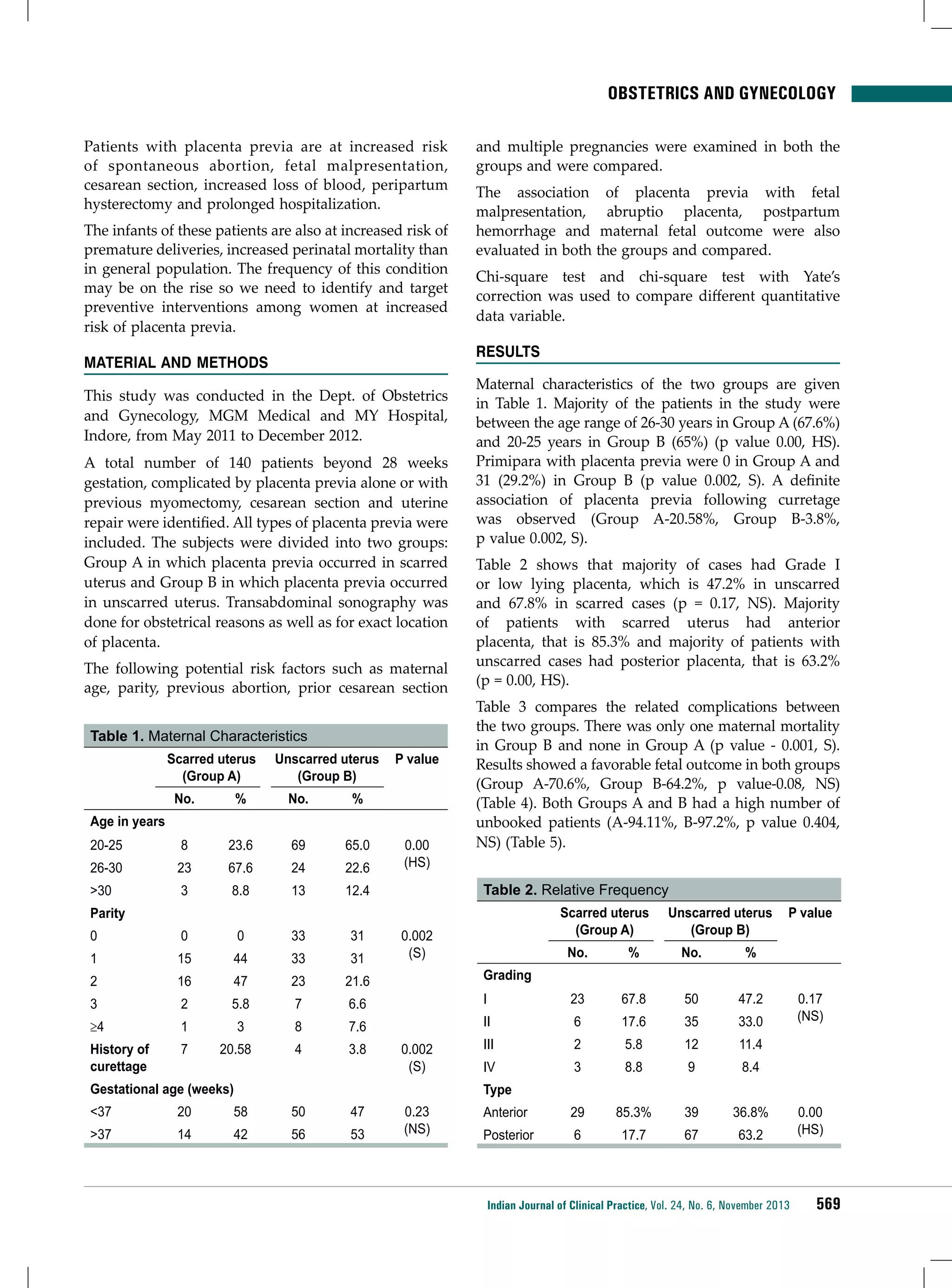
![ENDOCRINOLOGY
A
Patients achieved study endpoints (%)
80
70
60
Vildagliptin
68.5
Comparator
56.8
50
40
30
25.7
20
14.6
10
0
B
Primary efficacy endpoint
Secondary efficacy endpoint
0.0
Change in HbA1C from baseline (%)
−0.2
−0.4
−0.6
−0.8
−1.0
−1.1
−1.2
−1.4
−1.4
−1.6
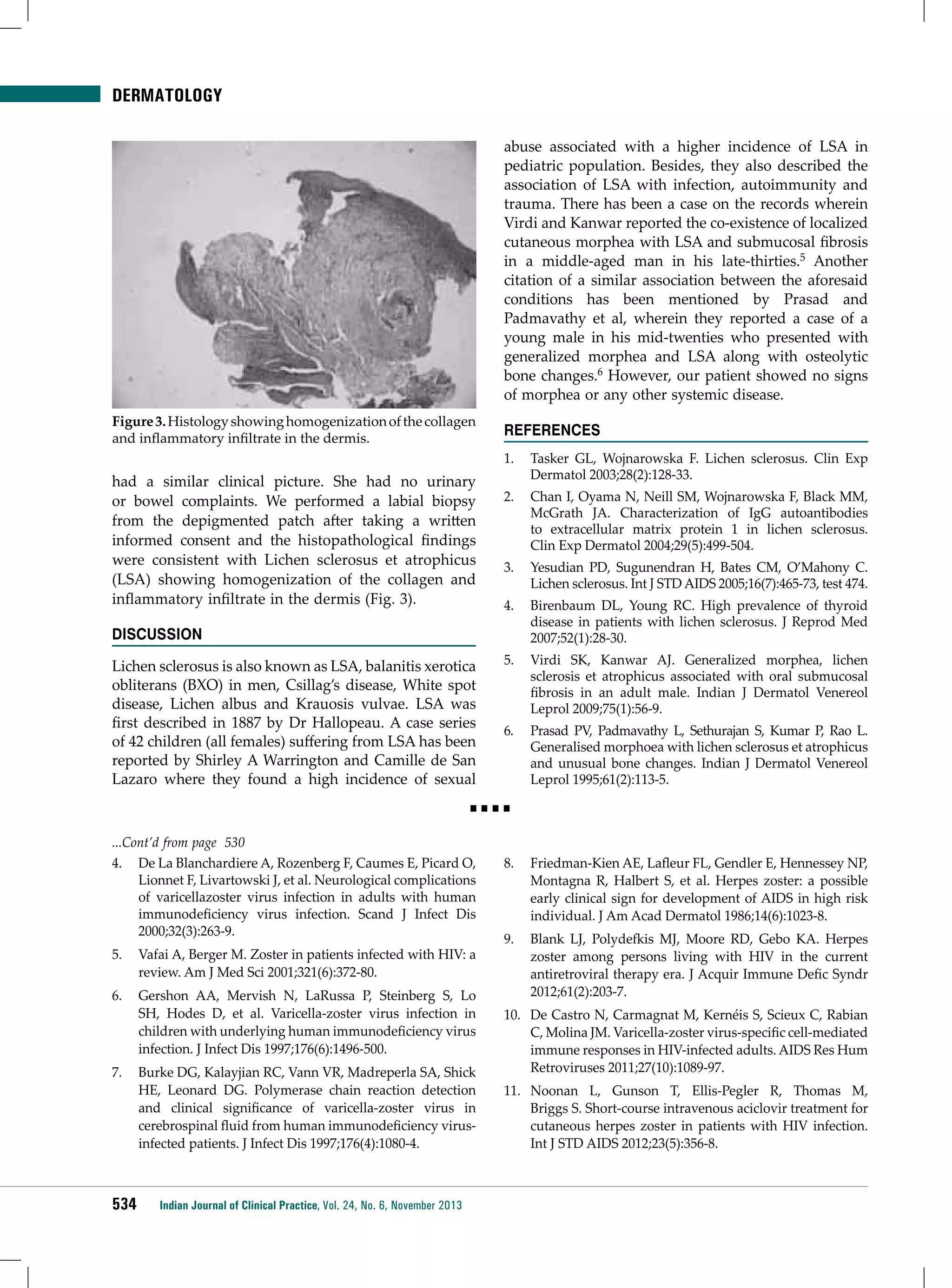
Figure 2. (A) Primary and secondary efficacy endpoints
(PP population); (B) Change in HbA1C after 12 months of
treatment (ITT population).
(A) Percentage of patients achieving study endpoints in PP population;
unadjusted odds ratios (95% CI): 1.65 (1.53, 1.79) for primary endpoint and
2.03 (1.83, 2.25) for secondary endpoint; both p <0.0001. (B) Mean HbA1C
change (± standard error) from baseline to study endpoint in ITT population
using an ANCOVA model.
These post hoc analyses demonstrated that vildagliptin
in combination with another OAD provides better
glycemic control than any other two-agent OAD
combination. After 12 months of treatment, the
vildagliptin cohort exhibited a greater proportion
of patients (unadjusted OR 1.65 [95% CI: 1.53, 1.79])
achieving the primary efficacy endpoint (reduction in
HbA1C >0.3% without peripheral edema, hypoglycemic
event, discontinuation due to a gastrointestinal event or
weight gain ≥5%) and the secondary efficacy endpoint
of HbA1C<7% without hypoglycemia and weight gain
≥3% from a baseline HbA1C of ≥7% (unadjusted OR 2.03
[95% CI: 1.83, 2.25]) versus all other two-agent OAD
combinations.
The results for this secondary efficacy endpoint
confirm results from other studies, which consistently
showed better responder rates with vildagliptin
versus comparators, although such comparisons have
limitations.14,15
The reduction in HbA1C was numerically greater with
vildagliptin combinations versus other two-agent
OAD combinations, as in the overall EDGE study
population.10 However, the vildagliptin cohort in
the Indian population showed a numerically greater
reduction (1.4%) when compared with the vildagliptin
cohort in the overall EDGE study population (1.2%).10
This larger reduction in HbA1C in Indian patients may
be partly explained by the higher baseline HbA1C in the
Indian patients.
The vildagliptin cohort showed a good safety and
tolerability profile without any clinically relevant trends,
which further corroborates the good safety profile of
vildagliptin.16,17 The study revealed that fewer patients
in the vildagliptin cohort reported hypoglycemia than
in the comparator cohort; the majority of patients
reporting hypoglycemia were using a metformin and
SU combination. This is consistent with results from
a previously reported large pooled analysis of safety
data, which showed that vildagliptin, as monotherapy
or in combination with metformin, thiazolidinedione
or an SU, is associated with significantly fewer
hypoglycemic events than comparators.17
There were some limitations to our study. Because
physicians were required to select any drug-based on
their clinical judgment, the open study design resulted
in a possible imbalance favoring the vildagliptin arm in
the overall EDGE study population, although this did
not seem to be the case in the Indian patients. Moreover,
the patients were recruited both in specialty and
routine care centers, which may have had an impact on
the overall results because of poor quality and missing
data that needed to be excluded from the effectiveness
analyses. In addition, unlike in randomized controlled
trials, reporting of AEs was based on a voluntary
reporting scheme, which might have led to unnoticed
or under-reported events.
conclusion
These post hoc analyses of the EDGE study confirmed
that vildagliptin in combination with another OAD
showed better overall clinical benefit versus any
other two-agent OAD combination, as measured
by a composite endpoint assessing effectiveness
(HbA1C reduction) and tolerability (peripheral edema,
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
541](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-41-2048.jpg)



![infectious diseases
Overall, AILD has a moderately aggressive course,
with occasional spontaneous remissions or protracted
responses to therapy. The median survival is 24 months.
AILD can evolve into high-grade lymphomas of T- or
B-cell type, EBV-positive B-cell lymphomas and chronic
lymphatic leukemia, among other kinds of lymphoma
and leukemia. Most patients eventually die of infections
due to immunologic compromise.
REFERENCES
1. Frizzera G, Moran EM, Rappaport H. Angioimmunoblastic lymphadenopathy with dysproteinaemia.
Lancet 1974;1(7866):1070-3.
2. Krenacs L, Schaerli P, Kis G, Bagdi E. Phenotype of
neoplastic cells in angioimmunoblastic T-cell lymphoma
is consistent with activated follicular B helper T cells.
Blood 2006;108(3):1110-1.
3. Dunleavy K, Wilson WH, Jaffe ES. Angioimmunoblastic
T cell lymphoma: pathobiological insights and clinical
implications. Curr Opin Hematol 2007;14(4):348-53.
4. Murakami YI, Yatabe Y, Sakaguchi T, Sasaki E, Yamashita
Y, Morito N, et al. c-Maf expression in angioimmunoblastic
T-cell lymphoma. Am J Surg Pathol 2007;31(11):1695-702.
5. Tripodo C, Gri G, Piccaluga PP, Frossi B, Guarnotta C,
Piconese S, et al. Mast cells and Th17 cells contribute
to
the
lymphoma-associated
pro-inflammatory
microenvironment
of
angioimmunoblastic
T-cell
lymphoma. Am J Pathol 2010;177(2):792-802.
6. Saito M, Fukuda T, Shiohara T, Homori M.
Angioimmunoblastic T-cell lymphoma: a relatively
common type of T-cell lymphoma in Sjögren’s syndrome.
Clin Exp Rheumatol 2005;23(6):888-90.
12. Rahmani R, Brenner S, Krakowski A, Lipitz R, Ilie B,
Behar AJ. Angioimmunoblastic lymphadenopathy with
scleromyxedema-like lesions and serum monoclonal
protein. Isr J Med Sci 1983;19(3):235-9.
13. Sellier S, Levesque H, Courville P, Joly P.
[Cyclophosphamide-induced neutrophilic disease in a
patient with angioimmunoblastic lymphadenopathy and
myelodysplastic syndrome]. Ann Dermatol Venereol
2006;133(5 Pt 1):459-62.
14. Jones B, Vun Y, Sabah M, Egan CA. Toxic epidermal
necrolysis secondary to angioimmunoblastic T-cell
lymphoma. Australas J Dermatol 2005;46(3):187-91.
15. Jarrett R, Walk N, Castellano-Sanchez AA, Kreisel FH. A
68-year-old man with shortness of breath and peripheral
edema. Angioimmunoblastic T-cell lymphoma. Arch
Pathol Lab Med 2006;130(2):219-22.
16. Goenka MK, Vaiphei K, Nagi B, Sriram PV, Joshi K,
Kochhar R. Angioimmunoblastic lymphadenopathy: an
etiology for gastrointestinal lymphomatous polyposis.
Am J Gastroenterol 1996;91(6):1236-8.
17. Matsumiya H, Arai A, Nagai A. [A case of angioimmunoblastic T-cell lymphoma with interstitial shadow which
disappeared after injection of hydrocortisone]. Nihon
Kokyuki Gakkai Zasshi 2006;44(7):537-40.
18. Alizadeh AA, Advani RH. Evaluation and management of
angioimmunoblastic T-cell lymphoma: a review of current
approaches and future strategies. Clin Adv Hematol
Oncol 2008;6(12):899-909.
19. Pautier P, Devidas A, Delmer A, Dombret H, Sutton L, Zini
JM, et al. Angioimmunoblastic-like T-cell non Hodgkin’s
lymphoma: outcome after chemotherapy in 33 patients
and review of the literature. Leuk Lymphoma 1999;32
(5-6):545-52.
7. Martel P, Laroche L, Courville P, Larroche C, Wechsler J,
Lenormand B, et al. Cutaneous involvement in patients
with angioimmunoblastic lymphadenopathy with
dysproteinemia: a clinical, immunohistological, and
molecular analysis. Arch Dermatol 2000;136(7):881-6.
20. Rodríguez J, Conde E, Gutiérrez A, Arranz R, Gandarillas
M, Leon A, et al. Prolonged survival of patients with
angioimmunoblastic T-cell lymphoma after high-dose
chemotherapy and autologous stem cell transplantation: the
GELTAMO experience. Eur J Haematol 2007;78(4):290-6.
8. Siegert W, Nerl C, Agthe A, Engelhard M, Brittinger G,
Tiemann M, et al. Angioimmunoblastic lymphadenopathy
(AILD)-type T-cell lymphoma: prognostic impact
of clinical observations and laboratory findings at
presentation. The Kiel Lymphoma Study Group. Ann
Oncol 1995;6(7):659-64.
21. Shinohara A, Asai T, Izutsu K, Ota Y, Takeuchi K,
Hangaishi A, et al. Durable remission after the administration of rituximab for EBV-negative, diffuse large
B-cell lymphoma following autologous peripheral blood
stem cell transplantation for angioimmunoblastic T-cell
lymphoma. Leuk Lymphoma 2007;48(2):418-20.
9. Singh MK, Solanki RN, Shah NJ, Tanna D, Patel DR,
Desai IM. Angioimmunoblastic lymphadenopathy with
dysproteinemia: thoracic involvement. Indian J Chest Dis
Allied Sci 2004;46(2):125-8.
22. Halene S, Zieske A, Berliner N. Sustained remission
from angioimmunoblastic T-cell lymphoma induced
by alemtuzumab. Nat Clin Pract Oncol 2006;3(3):165-8;
quiz 169.
10. Hosoki K, Okada S, Ichinohasama R, Yamaguchi M,
Uchiyama B, Maeyama T. Angioimmunoblastic T-cell
lymphoma developed with lymphocytic pleural effusion.
Intern Med 2007;46(11):739-42.
23. Amengual JE, Raphael BG. Sustained, durable responses
with alemtuzumab in refractory angioimmunoblastic
T-cell lymphoma. Leuk Lymphoma 2010;51(7):1347-50.
11. Ferran M, Gallardo F, Baena V, Ferrer A, Florensa L,
Pujol RM. The ‘deck chair sign’ in specific cutaneous
involvement by angioimmunoblastic T cell lymphoma.
Dermatology 2006;213(1):50-2.
552
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
24. Nakashima M, Suzuki K, Okada M, Takada K, Kobayashi
H, Hama Y. Successful coil embolization of a ruptured
hepatic aneurysm in a patient with polyarteritis nodosa
accompanied by angioimmunoblastic T cell lymphoma.
Clin Rheumatol 2007;26(8):1362-4.](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-52-2048.jpg)
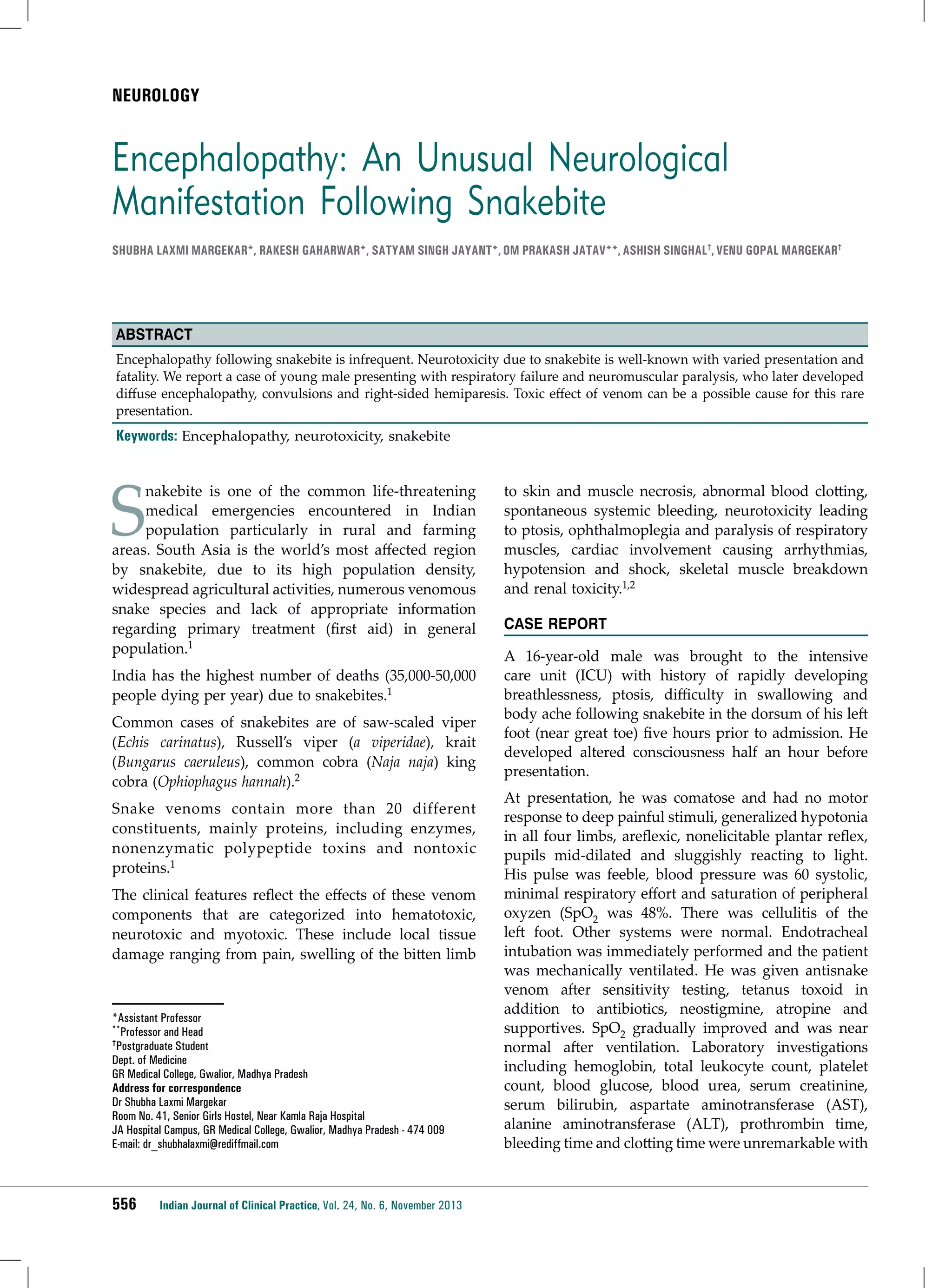
![INTERNAL MEDICINE
Cerebral Venous Thrombosis Due to Abrin Toxicity:
A Case Report
KV Rajalakshmi*, G Shivkumar**, S Karthikeyan, V Punitha, K Sangeetha
Abstract
Abrus precatorius (jequirity bean) is a common cause of accidental or intentional poisoning in the tropics. The data on exact
incidence of abrus poisoning is largely insufficient in our country, due to lack of reporting. The estimated lethal dose for humans
is 0.1-1 µg/kg. The toxic component is the protein abrin that causes widespread endothelial damage. Abrin causes a variety of
manifestations like hemorrhagic gastroenteritis with erosions, hemolysis, acute renal damage, dyselectrolytemia, hepatotoxicity
with elevated liver enzymes and seizures. Apart from the common manifestation of hemorrhagic gastroenteritis, patients
experiencing mental status perturbations have been identified and documented earlier. There have been previous reports of
elevated intracranial tension (ICT) in abrus poisoning, however, the exact cause for this phenomenon had not been elucidated.
We herein report a case of intentional A. precatorius poisoning in a young girl that caused cerebral venous thrombosis (CVT).
Keywords: Abrus precatorius poisoning, abrin poisoning, cerebral venous thrombosis, increased intracranial tension
A
brus precatorius seeds are often ingested with
suicidal intent in India, however, data on exact
incidence is lacking. Abrin is a potentially fatal
toxalbumin obtained from the seeds of A. precatorius
(jequirity bean, gundumani [Tamil]), which is similar
in structure and properties to ricin.1
We herein report a case of A. precatorius poisoning with
cerebral venous sinus thrombosis and intracerebral
bleed that has never been documented earlier.
CASE REPORT
An 18-year-old girl, a school dropout, was brought with
an alleged history of consumption of approximately
10-15 crushed abrus seeds on July 31, 2013 at 22:00
hours, following a family dispute. She was given local
indigenous treatment and taken to Taluk HQ Hospital,
Ulundurpet at 08:50 hours on August 1, 2013. There
she was instituted emergency care and subsequently
transferred to the Govt. Villupuram Medical College, at
19:35 hours, the same day. Upon arrival, the patient was
*Associate Professor
**Assistant Professor
Dept. of Internal Medicine
Govt. Villupuram Medical College, Villupuram,Tamil Nadu
Address for correspondence
Dr (Major) G Shivkumar
Assistant Professor
Dept. of Internal Medicine
Govt. Villupuram Medical College, Villupuram, Tamil Nadu - 605 601
E-mail: majorshivk@yahoo.com
dehydrated and had recurrent diarrhea and vomiting.
She was actively resuscitated with oral and intravenous
fluid replacement. Her hydration status improved and
vital parameters were stabilized. Her blood counts,
biochemical analysis and liver function tests (LFTs)
were within normal limits. Serum Na+ 158 mEq/l, K+
2.3 mEq/l, Cl- 126 mEq/l, HCO3- 26 mEq/l.
Patient’s vomit improved but diarrhea persisted despite
supportive treatment. On Day 4, patient developed
bloody diarrhea for which 1 unit of compatible group
blood was transfused. Biochemical analysis revealed
serum creatinine of 1.1 mg%, Na+ 143 mEq/l, K+ 2.4
mEq/l, Cl- 110 mEq/l and HCO3- 23 mEq/l. Repeat
LFTs including prothrombin time/INR (international
normalized ratio) were within normal limits. Her blood
pressure was 120/86 mmHg and urine output was 2,100
ml/24 hours. On Day 6, the patient experienced one
episode of generalized tonic-clonic seizures. She was
managed with intravenous loading and maintenance
dose of phenytoin. She became progressively drowsy
thereafter with persistent depressed mentation.
Fundus examination revealed bilateral papilledema. A
noncontrast computed tomography (CT) scan of brain
revealed a hyperdense lesion with perilesional edema
in left occipital region with hyperdense appearance
of sagittal sinus (filled delta sign). The features were
suggestive of superior sagittal sinus thrombosis with
hemorrhage in left occipital lobe. CT contrast study
was advised. Anti-edema and anticoagulant treatment
with unfractionated heparin commenced.
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
553](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-53-2048.jpg)




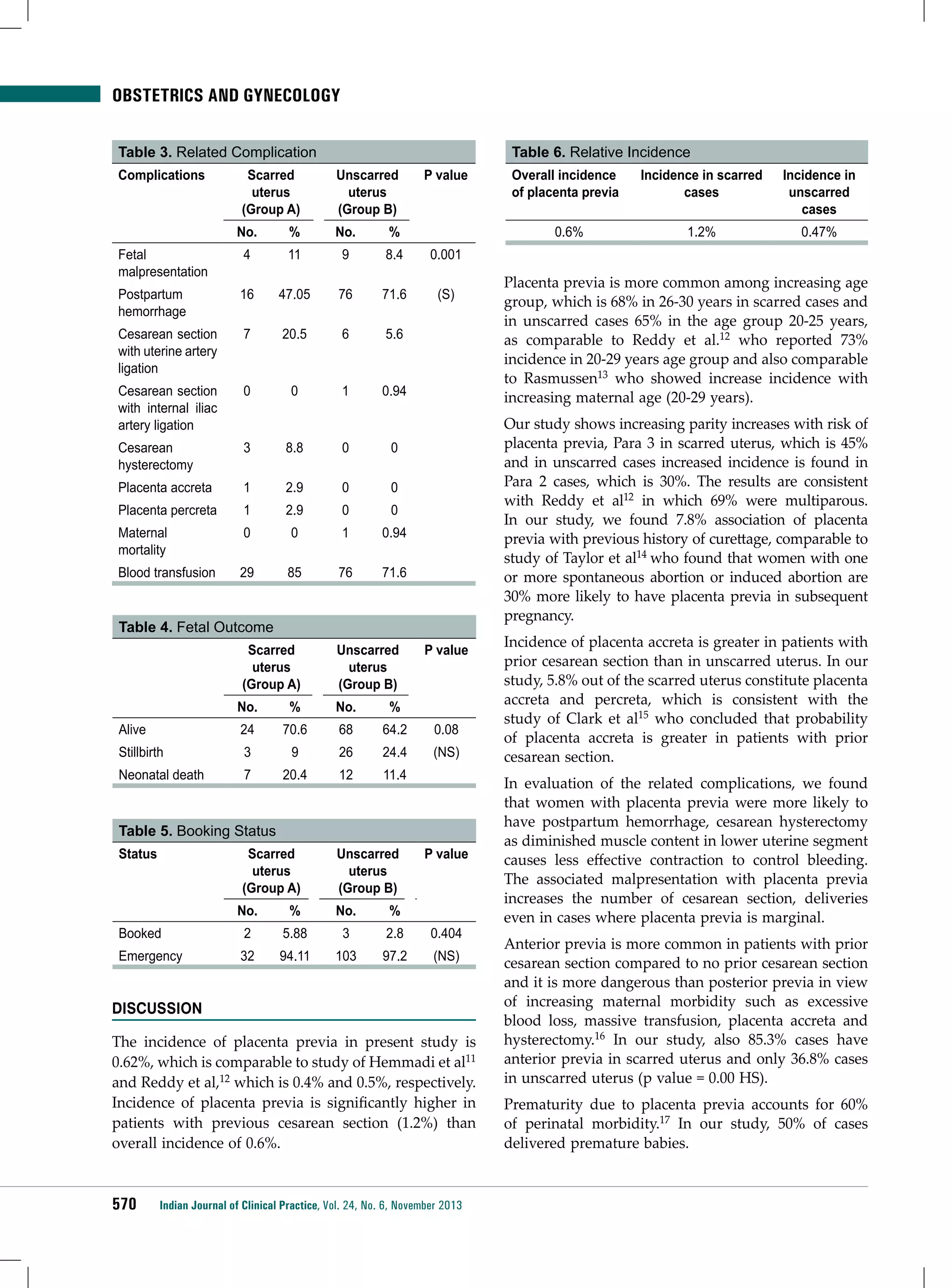

![ONCOLOGY
lytic lesion in superior aspect of left acetabulum.
X-ray skull showed lytic lesion in right parietal bone.
Computed tomography (CT) revealed an irregular
osteolytic lesion in right parietal bone that invaded and
expanded through both inner and outer tables of the
skull in full thickness with normal brain parenchyma
(Fig. 1a). X-ray chest showed consolidation in left lower
zone (Fig. 1b). Ultrasound abdomen was normal. He
underwent gross total removal of the lesion to establish
the diagnosis. Histological examination of the tumor
revealed a metastatic adenocarcinoma.
initial treatment, modified follow-up or reconsideration
of surgical therapy for the primary tumor.9,11
Discussion
3. Wong GK, Boet R, Poon WS, Ng HK. Lytic skull metastasis
secondary to thyroid carcinoma in an adolescent. Hong
Kong Med J 2002;8(2):149-51.
Lung cancer is the most common cancer in the world
and accounts for 12.3% of all new cancer cases with
millions of deaths per year.5 According to reports by
the American Lung Association, the vast majority of
patients with lung cancer (85%) have metastatic disease
at the time of presentation.6 Patients with metastatic lung
cancer have a 5-year survival rate of 2.1%, compared
to those who have disease limited to the lungs at
48.5%.7 Hematogenous skull metastases can be caused
by nearly all types of tumors including breast, lung,
prostate, thyroid carcinoma, malignant melanoma).1,3,8
However, the most common sites for metastases from
lung cancer are the upper abdomen followed by lung
and pleura and lastly bone.2 Metastases from lung
cancer involve spine and hip but skull involvement
is uncommon.9 X-ray and CT is a keystone in the
diagnostic evaluation of suspected lung cancer, because
it provides the most detailed anatomical images.10
Multiplicity, irregular edges and absence of peripheral
sclerosis should arouse suspicion of malignancy and
a biopsy is warranted in these cases.3 Preoperative
contrast-enhanced Magnetic resonance imaging of the
brain and skeleton is recommended for the detection
of parenchymal and osseous lesions in patients with
large pulmonary lesions (>3 cm diameter or higher
than T1 stage).9,11 The correct staging of patients with
lung cancer is essential for appropriate care and cost
containment as patients with nonresectable metastatic
disease may need additional therapy at the time of
References
1. Stark AM, Eichmann T, Mehdorn HM. Skull metastases:
clinical features, differential diagnosis, and review of the
literature. Surg Neurol 2003;60(3):219-25; discussion 225-6.
2. Aquino SL, Fischman AJ. Does whole-body 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography
have an advantage over thoracic positron emission
tomography for staging patients with lung cancer? Chest
2004;126(3):755-60.
4. Kim SH, Kosnik E, Madden C, Morran S, Rusin J, Gordon
T, et al. Lytic skull metastasis from a follicular thyroid
carcinoma in a child. Pediatr Neurosurg 1998;28(2):84-8.
5. Tyczynski JE, Bray F, Parkin DM. Lung cancer in Europe
in 2000: epidemiology, prevention, and early detection.
Lancet Oncol 2003;4(1):45-55.
6. Pretreatment evaluation of non-small-cell lung cancer. The
American Thoracic Society and The European Respiratory
Society. Am J Respir Crit Care Med 1997;156(1):320-32.
7. Trends in lung cancer morbidity and mortality. American
Lung Association Epidemiology and Statistics Unit,
Research and Scientific Affairs, June 2003. Available at:
http://www. lungusa.org/atf/cf/. Accessed March 12, 2008.
8. Bontoux D, Plazanet F, Azais I. Distribution of bone
metastases of cancers. A scintigraphic study of 376 cases.
Bull Acad Natl Med 1998;182(5):997-1008; discussion
1008-9.
9. Earnest F 4th, Ryu JH, Miller GM, Luetmer PH, Forstrom
LA, Burnett OL, et al. Suspected non-small cell lung
cancer: incidence of occult brain and skeletal metastases
and effectiveness of imaging for detection - pilot study.
Radiology 1999;211(1):137-45.
10. Verschakelen JA, Bogaert J, De Wever W. Computed
tomography in staging for lung cancer. Eur Respir J Suppl
2002;35:40s-48s.
11. Akeson P, Larsson EM, Kristoffersen DT, Jonsson E,
Holtås S. Brain metastases--comparison of gadodiamide
injection-enhanced MR imaging at standard and high
dose, contrast-enhanced CT and non-contrast-enhanced
MR imaging. Acta Radiol 1995;36(3):300-6.
■■■■
For HIV-infected patients with cancer undergoing chemotherapy, the integrase strand-transfer inhibitor raltegravir
is the best choice for viral suppression, according to a new study presented at the 53rd Interscience Conference
on Antimicrobial Agents and Chemotherapy. The efficacy of raltegravir is similar to that of nonnucleoside reversetranscriptase inhibitors, but the rate of adverse events is lower.
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
573](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-73-2048.jpg)
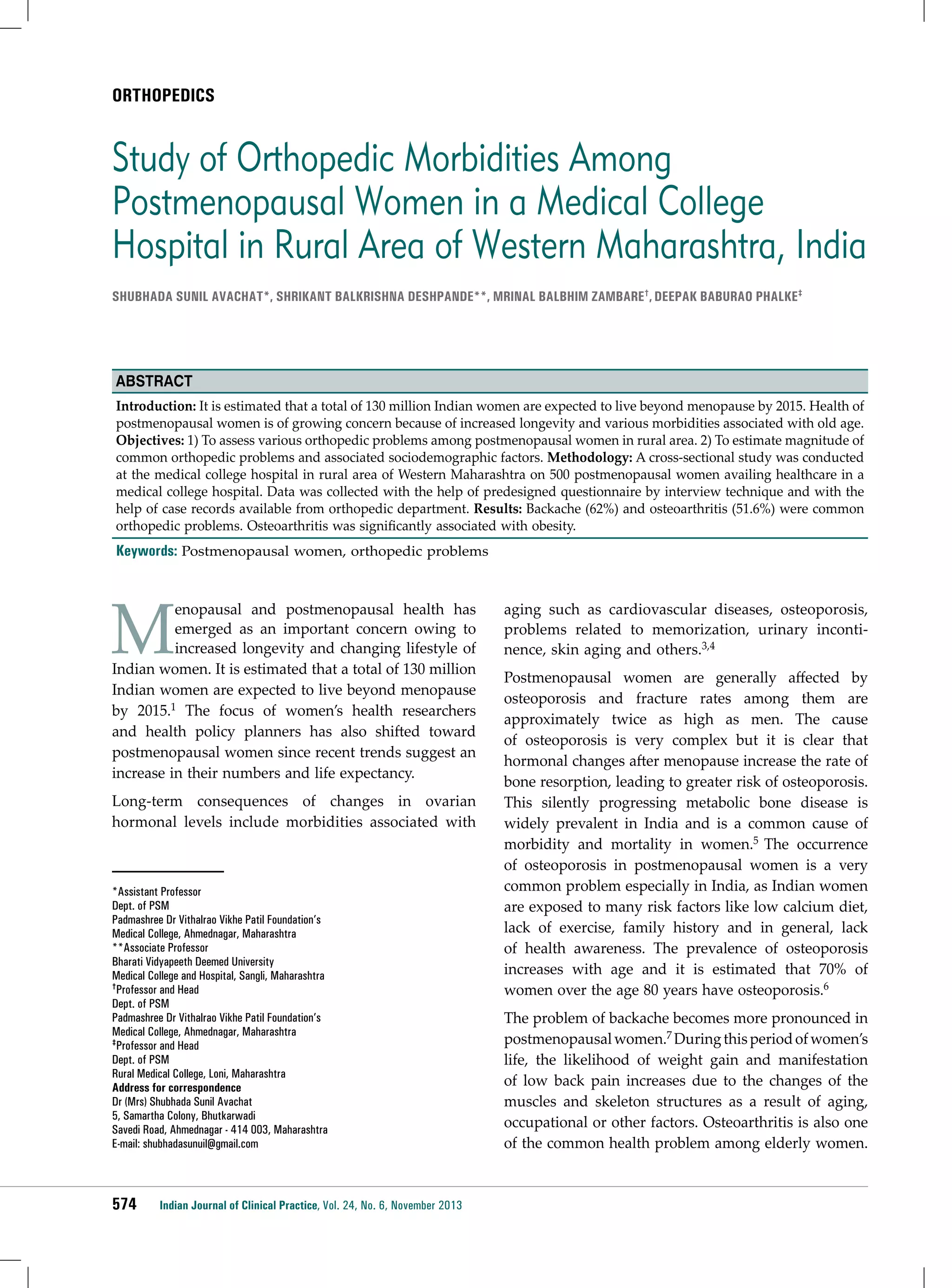

![ORTHOPEDICS
are the common orthopedic problems and large
number of these health problems can be prevented and
managed by simple measures like exercise, diet and
proper healthcare.
Acknowledgment
7. Popkess-Vawter S, Patzel B. Compounded problem:
chronic low back pain and overweight in adult females.
Orthop Nurs 1992;11(6):31-5, 43.
8. Felson DT. The epidemiology of knee osteoarthritis:
results from the Framingham Osteoarthritis Study. Semin
Arthritis Rheum 1990;20(3 Suppl 1):42-50.
We are thankful to the management of Pravara Medical Trust,
Dept. of Orthopedic, Pravara Rural Hospital, for allowing
the study and the interns Miss Bajpayee and Sharmin Bala
for their help.
9. Kellgren JH, Lawrence JS, Bier F. Genetic factors in
generalized osteoarthrosis. Ann Rheum Dis 1963;22:
237-55.
References
11. Mandal PK, Chakrabarty D, Manna N, Mallik S. Disability
among geriatric females: an uncared agenda in rural
India. Sudanese J Pub Health 2009;4(4):377-82.
1. Sengupta A. The emergence of the menopause in India.
Climacteric 2003;6(2):92-5.
2. World Health Organization. Women Aging and Health.
WHO: Geneva, 2000. Fact sheet No. 252.
3. Genazzani AR, Gambacciani M, Schneider HP,
Christiansen C. International Menopause Society Expert
Workshop. Postmenopausal osteoporosis: therapeutic
options. Climacteric 2005;8(2):99-109.
4. Isles CG, Hole DJ, Hawthorne VM, Lever AF. Relation
between coronary risk and coronary mortality in women
of the Renfrew and Paisley survey: comparison with men.
Lancet 1992;339(8795):702-6.
5. Gupta A. Osteoporosis in India - the nutritional
hypothesis. Natl Med J India 1996;9(6):268-74.
6. Osteoporosis in Postmenopausal Women: Diagnosis and
Monitoring. Summary, Evidence Report/Technology
Assessment: No.28. Agency for Healthcare Research and
Quality Publication No. 01-E031, Feb 2001. Available at:
http://www.ahrq.gov/clinic/epcsums/osteosum.htm
10. Kumar P. Social classification - need for constant updating.
IJCM 1993;18(2):60-1.
12. Scharla S, Oertel H, Helsberg, et al. Skeletal pain in
postmenopausal women with osteoporosis. J Bone Miner
Res 2005;20(Suppl 1):318-98.
13. Felson DT. The epidemiology of knee osteoarthritis:
results from the Framingham Osteoarthritis Study. Semin
Arthritis Rheum 1990;20(3 Suppl 1):42-50.
14. Slemenda CW. The epidemiology of osteoarthritis of the
knee. Curr Opin Rheumatol 1992;4(4):546-51.
15. Eti E, Kouakou HB, Daboiko JC, Ouali B, Ouattara B, Gabla
KA, et al. Epidemiology and features of knee osteoarthritis
in the Ivory Coast. Rev Rhum Engl Ed 1998;65(12):
766-70.
16. Lena A, Ashok K, Padma M, Kamath V, Kamath A. Health
and social problems of the elderly: a cross-sectional study
in Udupi Taluk, Karnataka. Indian J Community Med
2009;34(2):131-4.
Diet Combined with Exercise Relieves Arthritic Knee Pain
Osteoarthritis (OA) is a common trouble in old age. Symptoms of OA may include joint pain, tenderness, stiffness,
locking and sometimes an effusion. Generally, doctors advise the patients to reduce weight to help reduce knee
pain. A study was published recently that aimed to assess the clinical and functional outcome in knee pain in
arthritic patients by modifying diet alone (Group A), modifying diet and combining it with exercise (Group B),
and by exercise only (Group C). It was single-blind, randomized clinical trial, which was done for 18 months to
study the outcome of pain on 454 overweight and obese people aged >55 years with positive radiographic knee
OA findings. It was observed that slightly changing the lifestyle by doing some amount of exercise along with
diet control were more effective in reducing weight, inflammation and pain. Their quality-of-life improved as
they had less pain and more mobility. On the contrary, the group that performed only diet modifications or only
exercised did not experience such positive results. In diet modifications, two meals consisted of only nutritional
shakes while the third meal had very less fats but was rich in vegetables. Average weight loss was greater in the
diet and exercise group (−10.6 kg; 95% confidence interval [CI], −14.1 to −7.1 kg) and the diet group (−8.9 kg; 95%
CI, −12.4 to −5.3 kg) compared with the exercise group (−1.8 kg; 95% CI, −5.7 to 1.8 kg) at the 18-month follow-up.
On 6-month follow-up, all the three groups had similar amount of pain reduction, but on 18-month follow-up
it was noticed that the group with diet modifications combined with exercises provided more relief in pain and
better mobility. So, it was concluded that diet or exercise alone would be less effective than diet clubbed with
exercise in knee OA.
(Source: JAMA 2013;310:1263-73.)
Indian Journal of Clinical Practice, Vol. 24, No. 6, November 2013
577](https://image.slidesharecdn.com/ijcp-140222021057-phpapp01/75/Ijcp-77-2048.jpg)