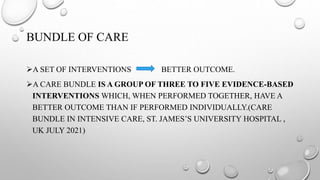
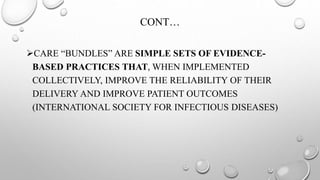
This document discusses various care bundles for critically ill patients, including:
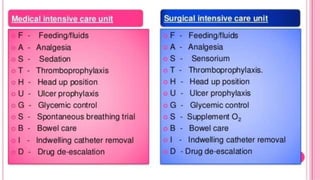
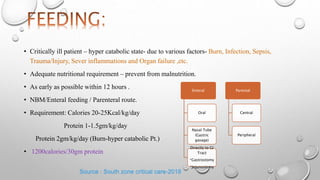
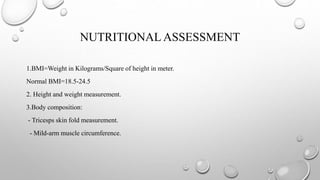
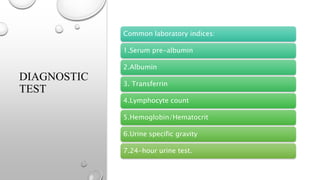
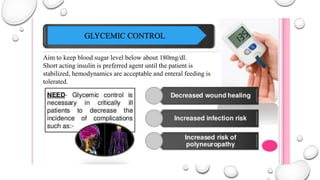
- Nutrition bundles to provide adequate calories and protein within 12 hours to prevent malnutrition.
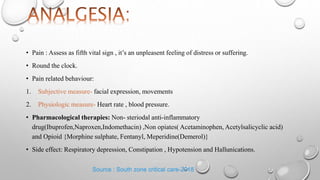
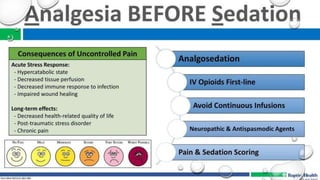
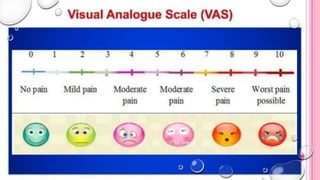
- Pain management bundles using pharmacological and non-pharmacological approaches.
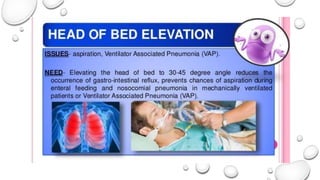
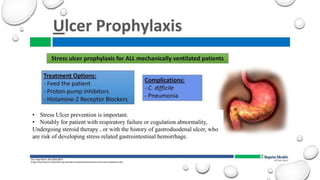
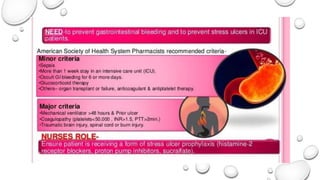
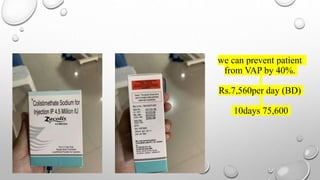
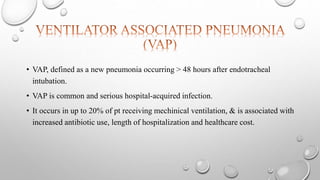
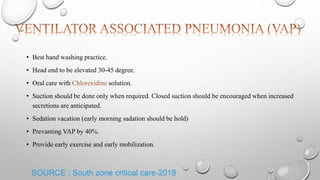
- Ventilator bundles like daily sedation holds to assess readiness for extubation.
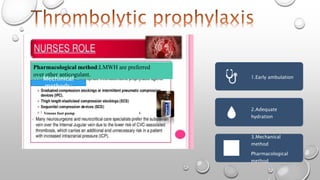
- Thromboprophylaxis bundles using mechanical methods like foot pumps and pharmacological methods like low molecular weight heparin.