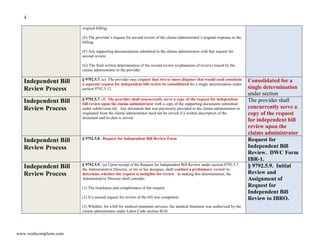
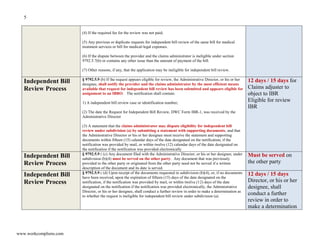
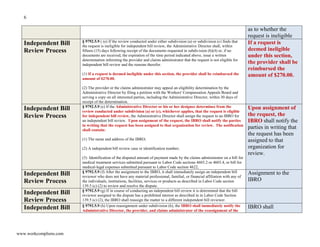
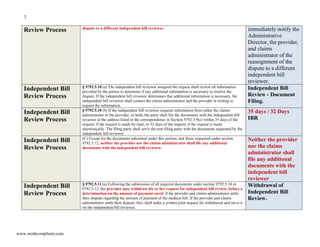
This document provides information about California's independent bill review process established under SB 863. It includes a quick reference guide to the rules governing the IBR process with 14 pages of content and timelines. The document also contains 6 flowcharts illustrating the steps in the IBR process. It was created by Richard Boggan, an attorney, as a reference for understanding how the IBR system works according to the emergency regulations.