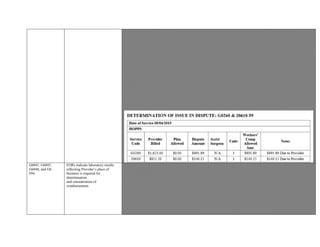
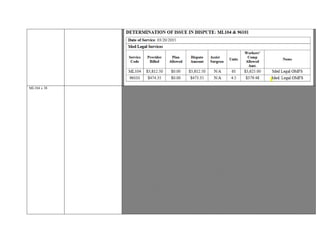
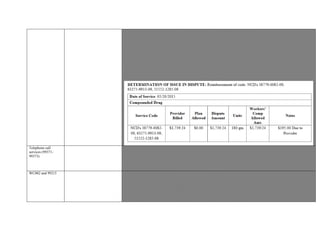
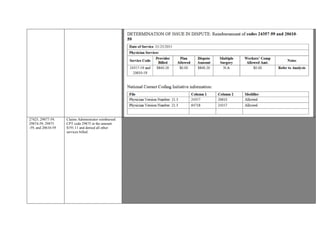
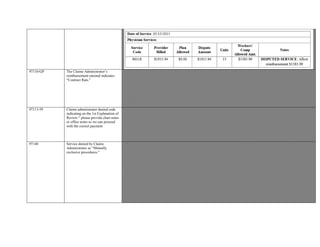
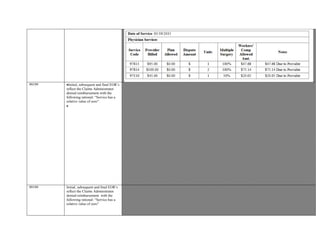
The UR determined that codes 23412 and 23120 performed on 11/18/2015 should be reimbursed based on guidelines. The claims administrator had denied reimbursement indicating pre-authorization was required and visit limits were reached. However, the UR documentation approved the procedures performed. As documentation supported the codes, reimbursement was warranted.




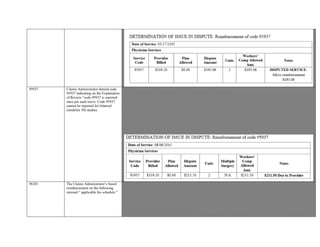
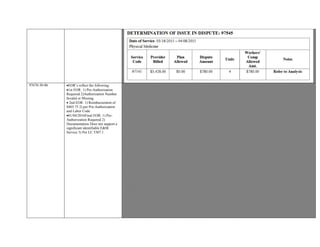
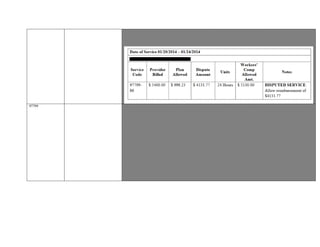
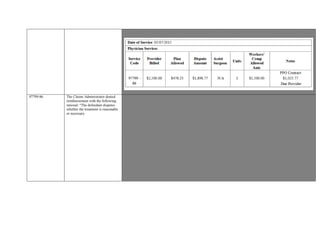
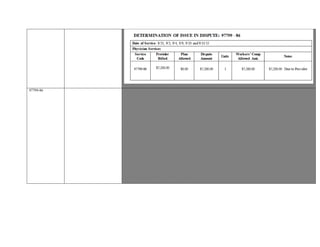
![Initial EOR does not provide a clear indication for“0.00” reimbursement .Services performed in addition to other services;
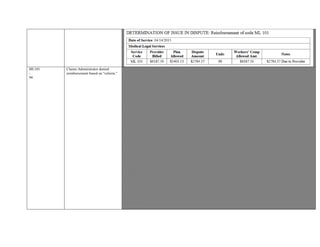
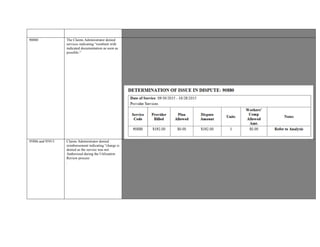
$359.07 out of $500,347.68 reimbursed.
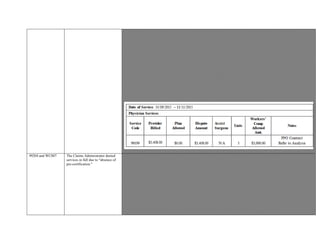
Documentation indicates SBR requested; 2ndEOR not received.
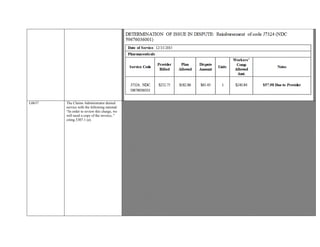
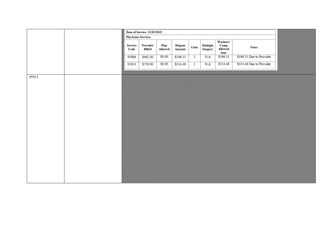
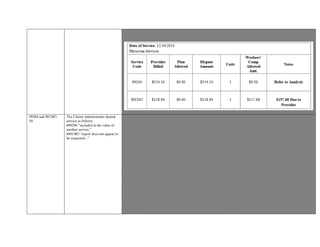
CPT Status Indicator, Weight and AMA CPT Code Description:
CPT 33249: S,442.3292 , Insertion or replacement of permanent implantable defibrillator system, with transvenous lead(s),
single or dual chamber
CPT 93005: Q3, 0.3732, Electro cardiogram tracing, Electrocardiogram, routine ecg with at least 12 leads; tracing only,
without interpretation and report
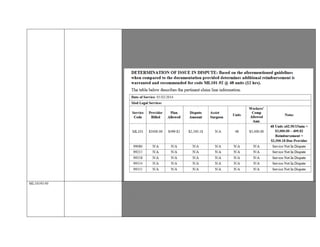
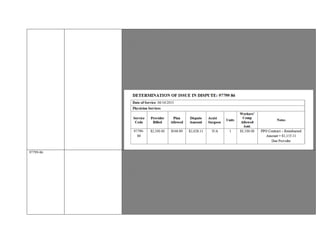
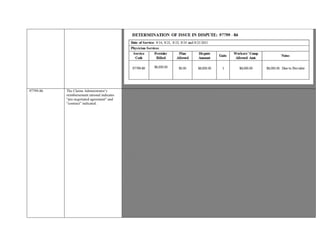
Contractual Agreement not submitted for IBR.
CCR § 9789.33 , For services rendered on or after September 1, 2014, Status Indicators; “S”, “T”, “X”, or “V”, “Q1,” Q2,” or
“Q3 ” must qualify for separate payment.” must qualify for separate payment. APC relative weight x adjusted conversion factor x
1.212 workers’ compensation multiplier, pursuant to Section 9789.30(aa). See Section 9789.39(b) for the APC relative weight by
date of service
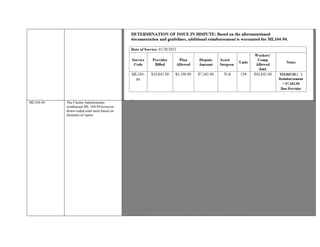
Based on the aforementioned documentation and guidelines, additional reimbursement
is indicated for
3
3249 and 93005.
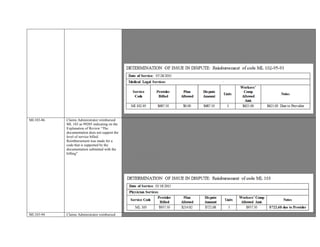
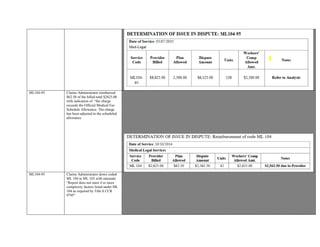
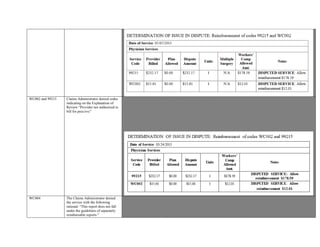
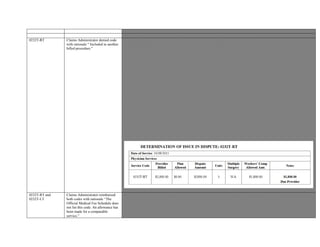
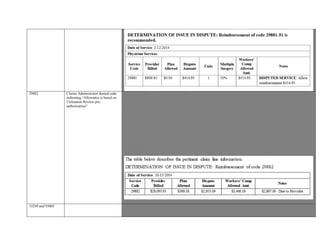
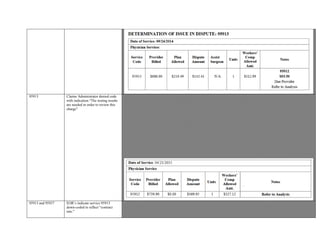
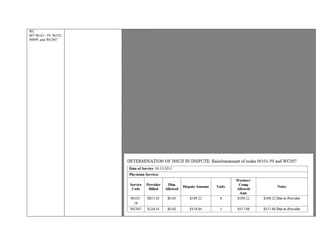
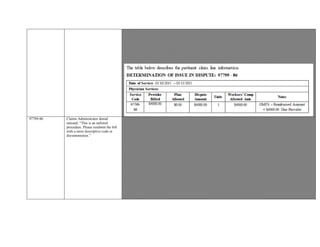
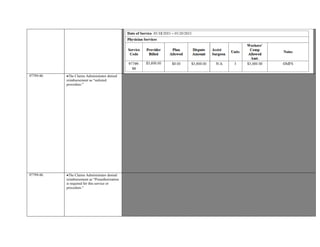
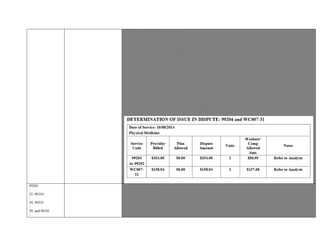
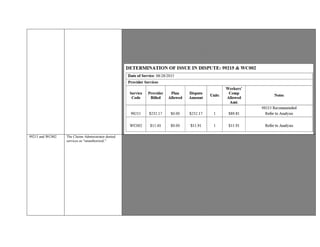
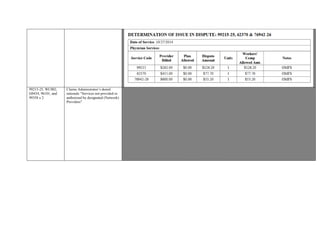
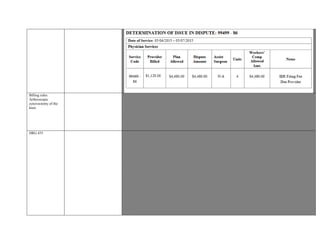
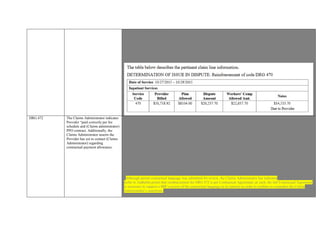
63047-59-51 Claims Administrator was incorrect
to deny code 63047-59-51 and
therefore, reimbursement is
recommended.
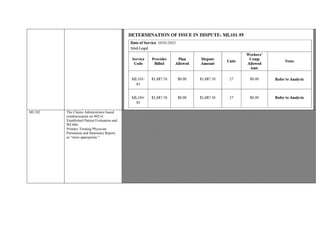
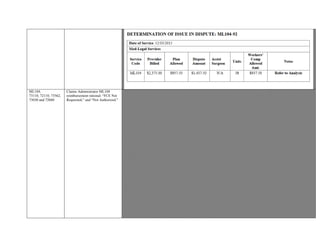
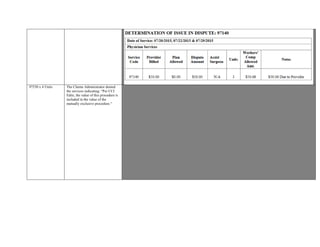
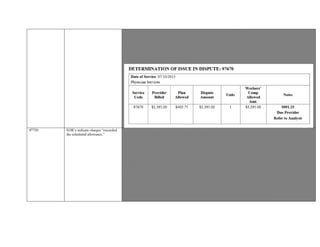
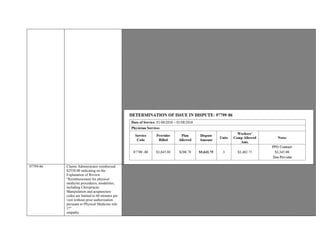
Provider is dissatisfied with denial of CPT code 63047-59-51.
Based on the NCCI edits that exist with code 63047, Modifier Indicator is showing ‘1’ as a modifier appended can override the
NCCI Edit with supporting documentation. Modifier -59 is an accepting modifier for this rule per NCCI.
CPT 63047 -Laminectomy, facetectomy and foraminotomy (unilateral or bilateral with decompression of spinal cord, cauda
equina and/or nerve root[s], [eg, spinal or lateral recess stenosis]), single vertebral
segment; lumbar
Based on review of the operative report page 2 paragraph two, Provider documents “dissection carried down bilaterally to
expose the inferior L3 lamina up the S1 lamina, and dissection was carried out laterally to the edges of the facets.”
Claims Administrator was incorrect to deny code 63047-59-51 and therefore, reimbursement is recommended.](https://image.slidesharecdn.com/9-payments-blackedout-161212014744/85/9-payments-blacked-out-14-320.jpg)
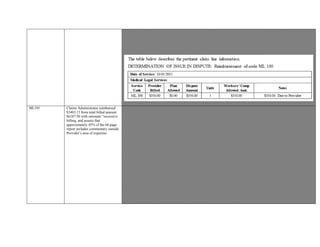
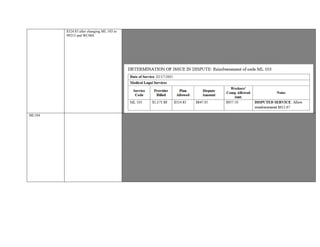
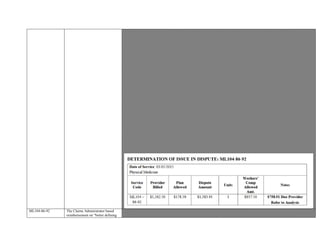
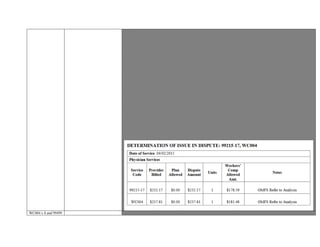
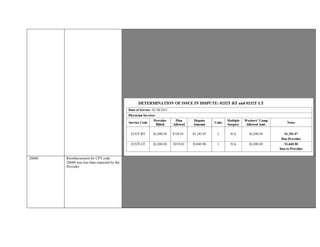
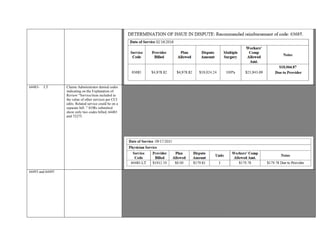
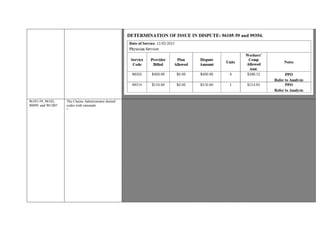
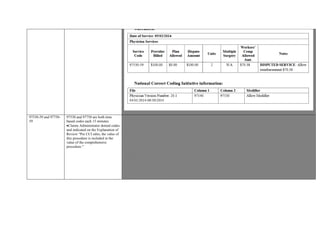
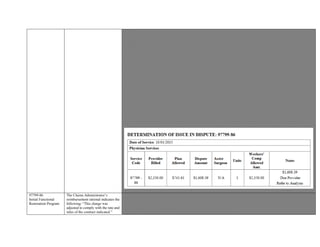
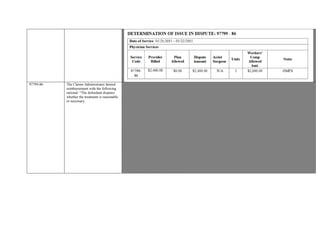
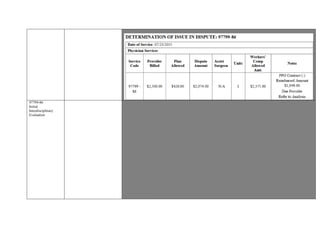
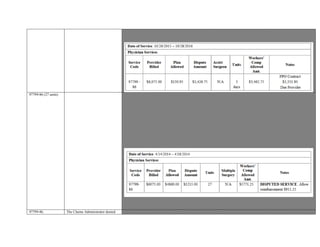
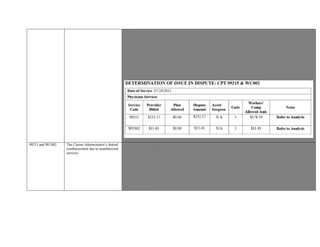
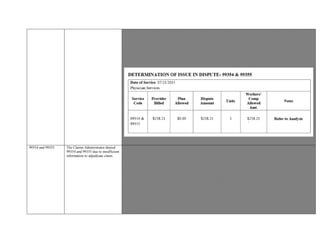
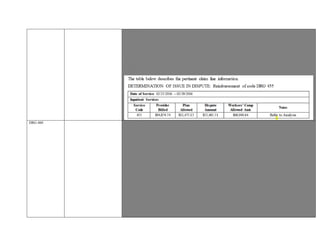
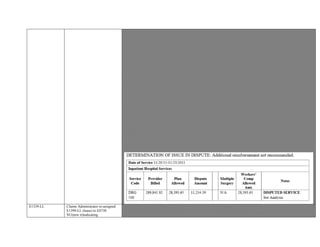
![A PPO discount of 5% will be applied as well as the multiple surgical procedures reimbursement Rule #7 Provider is dissatisfied
with denial of CPT code 63047-59-51.
Based on the NCCI edits that exist with code 63047, Modifier Indicator is showing ‘1’ as a modifier appended can override the
NCCI Edit with supporting documentation. Modifier -59 is an accepting modifier for this rule per NCCI.
CPT 63047 -Laminectomy, facetectomy and foraminotomy (unilateral or bilateral with decompression of spinal cord, cauda
equina and/or nerve root[s], [eg, spinal or lateral recess stenosis]), single vertebral
segment; lumbar
Based on review of the operative report page 2 paragraph two, Provider documents “dissection carried down bilaterally to
expose the inferior L3 lamina up the S1 lamina, and dissection was carried out laterally to the edges of the facets.”
Claims Administrator was incorrect to deny code 63047-59-51 and therefore, reimbursement is recommended.
A PPO discount of 5% will be applied as well as the multiple surgical procedures reimbursement Rule #7
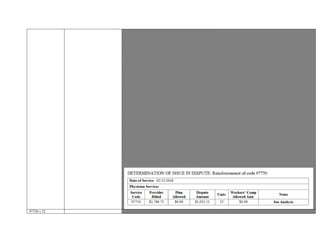
63650 and 63650
-59
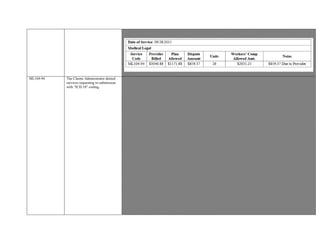
EOR indicates DWC Payment
Reduction G1:“The charge exceeds
the Official Medical Fee Scheduled
Allowance.”
Provider seeking 100 % ASC remuneration for 63650 & 63650-59 for date of service 10/13/2015.
EOR indicates DWC Payment Reduction G1:“The charge exceeds the Official Medical Fee Scheduled Allowance.”
CMS 1500 reflects Bill Type “831.”
Contractual Agreement not submitted for IBR.
For services rendered on or after December 1, 2014, section 9789.30, subsections (a) adjusted conversion factor, (e) APC
payment rate, (f) APC relative weight, (j) Facility Only Services,(q) labor](https://image.slidesharecdn.com/9-payments-blackedout-161212014744/85/9-payments-blacked-out-15-320.jpg)





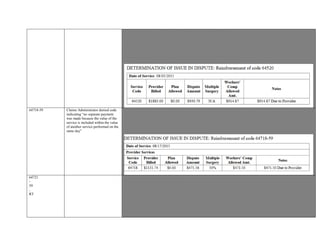









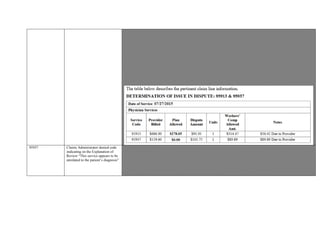





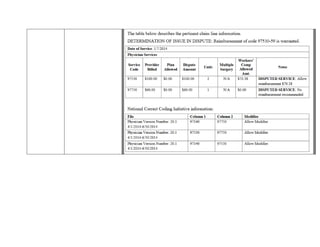








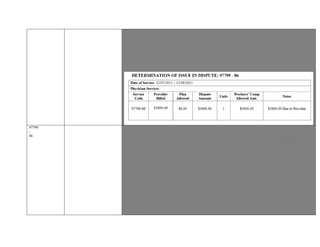















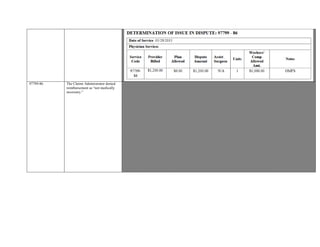




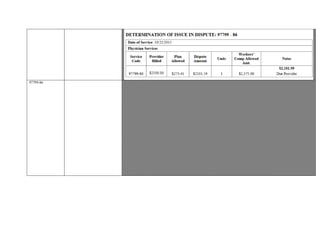

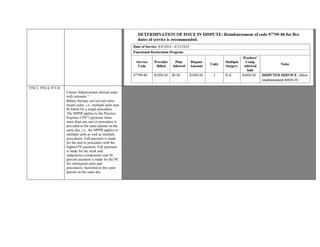













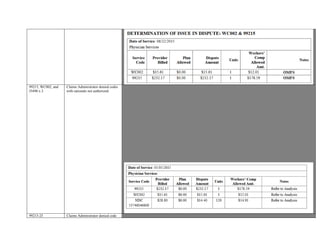


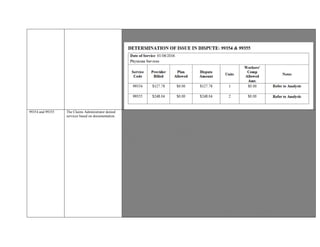


















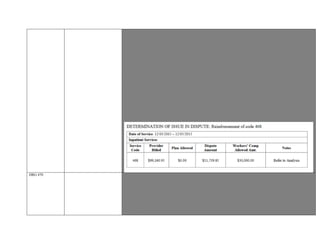




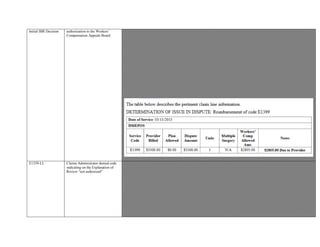
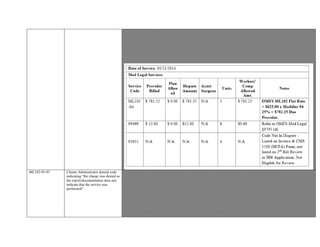
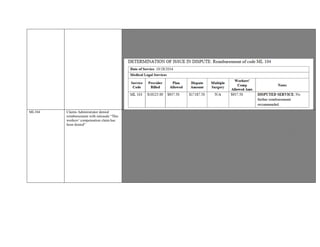
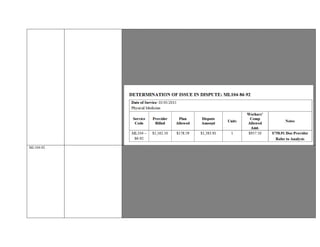
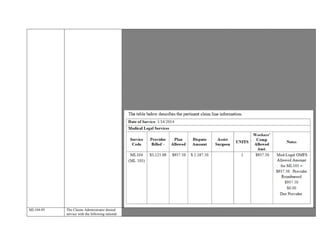
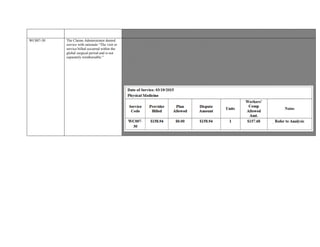
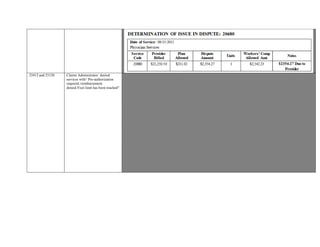
![Worker reflects entire purchase price of unit.
Invoice reflects unit delivered to Injured Workers Home Address.
Claims Administrator not denying E1399 was authorized.
§9789.60. Durable Medical Equipment, Prosthetics, Orthotics, Supplies. (a) For services, equipment, or goods provided after
January 1, 2004, the maximum reasonable reimbursement for durable medical equipment, supplies and materials, orthotics,
prosthetics, and miscellaneous supplies and services shall not exceed one hundred twenty (120) percent of the rate set forth in the
CMS' Durable Medical Equipment, Prosthetics/Orthotics, and Supplies (DMEPOS) Fee Schedule, as established by Section 1834
of the Social Security Act (42 U.S.C. § 1395m) and applicable to California.
Title 8, §9789.19 For services rendered on or after 4/1/2014, use: the OMFS Durable Medical Equipment, Prosthetics, Orthotics,
Supplies (DMEPOS) Fee Schedule applicable to the date of service
H-wave stimulation is a form of electrical stimulation that differs from other forms of electrical stimulation, such as
transcutaneous electrical nerve stimulation (TENS), in terms of its waveform (MTUS–Chronic Pain Treatment Guidelines).
The main advantage of these technologies over currently applied electrical stimulators (eg, transcutaneous electrical nerve
stimulator [TENS], interferential [IF], neuromuscular electrical stimulation [NMES], high-volt galvanic, etc.) is that H-
Wave's(R) small fiber contraction does not trigger an activation of the motor nerves of the large white muscle fibers or the
sensory delta and C pain nerve fibers, thus eliminating the negative and painful effects of tetanizing fatigue, which reduces
transcapillary fluid shifts. Another function of the H-Wave(R) device is an anesthetic effect on pain conditions, unlike a TENS
unit which in the short term activates a hypersensory overload effect (gate theory) to stop pain signals from reaching the thalamic
region of the brain.(PubMed - 20048478)
A DMEPOS or HCPCS code has yet to be assigned for H-Wave devices and a there is no comparable service code. As such, the
Provider may be reimbursed a percentage of the billed Usual and Customary Charge under the OMFS or an existing Contractual
Agreement.
The Provider is the Manufacture of the Unit; Contractual Agreement reflects “15% off Usual and Customary.”
Based on the documentation and guidelines, reimbursement is warranted for E1399-LL
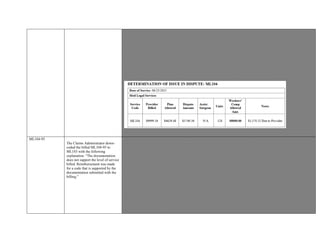
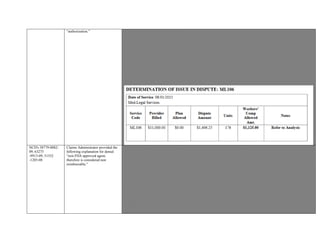
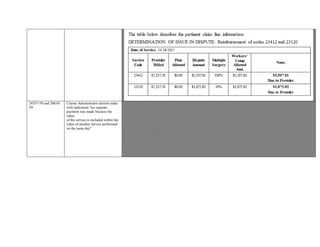
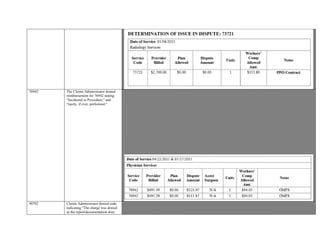
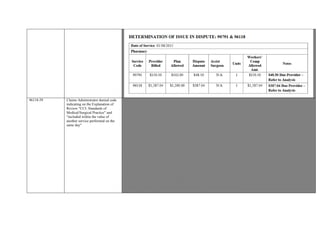
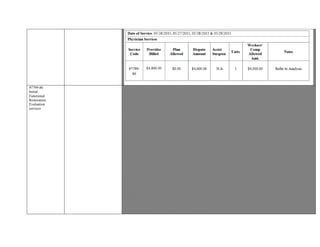
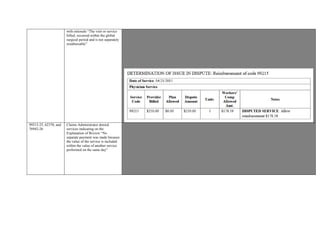
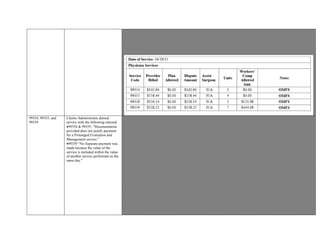
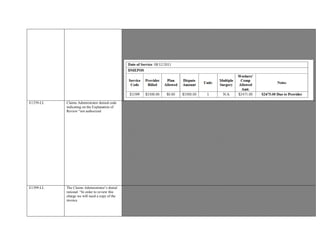
G0260 Provider remuneration for G0260 Status Indicator “T” injection procedure for sacroiliac joint; provision of anesthetic, steroid
and/or other therapeutic agent, with or without arthrography performed on
01/27/2016.
Claims Administrator denied reimbursement with rationale“ Per CA OP regs, non-surgical services
(ER, “ Facility -Only”, “Other” ) not paid in ASC setting .”
Amended Notice: Notice of Authorization dated December 22, 2015 from Utilization Review](https://image.slidesharecdn.com/9-payments-blackedout-161212014744/85/9-payments-blacked-out-167-320.jpg)