1) Hypocalcemia and hypoparathyroidism occur when calcium levels decrease below normal ranges and can be caused by vitamin D deficiency, parathyroid issues, or other medical conditions.
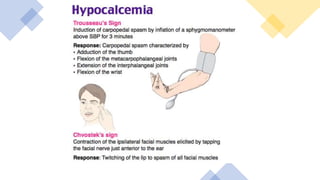
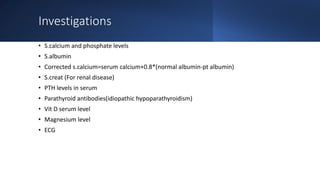
2) Symptoms include tingling, muscle cramps, seizures, and cardiac issues. Investigations include measuring calcium, albumin, phosphate, PTH, and vitamin D levels.
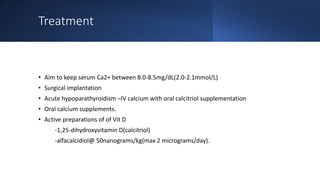
3) Treatment depends on severity but may include IV calcium for emergency symptoms and long term oral calcium and vitamin D supplements to maintain normal calcium levels.