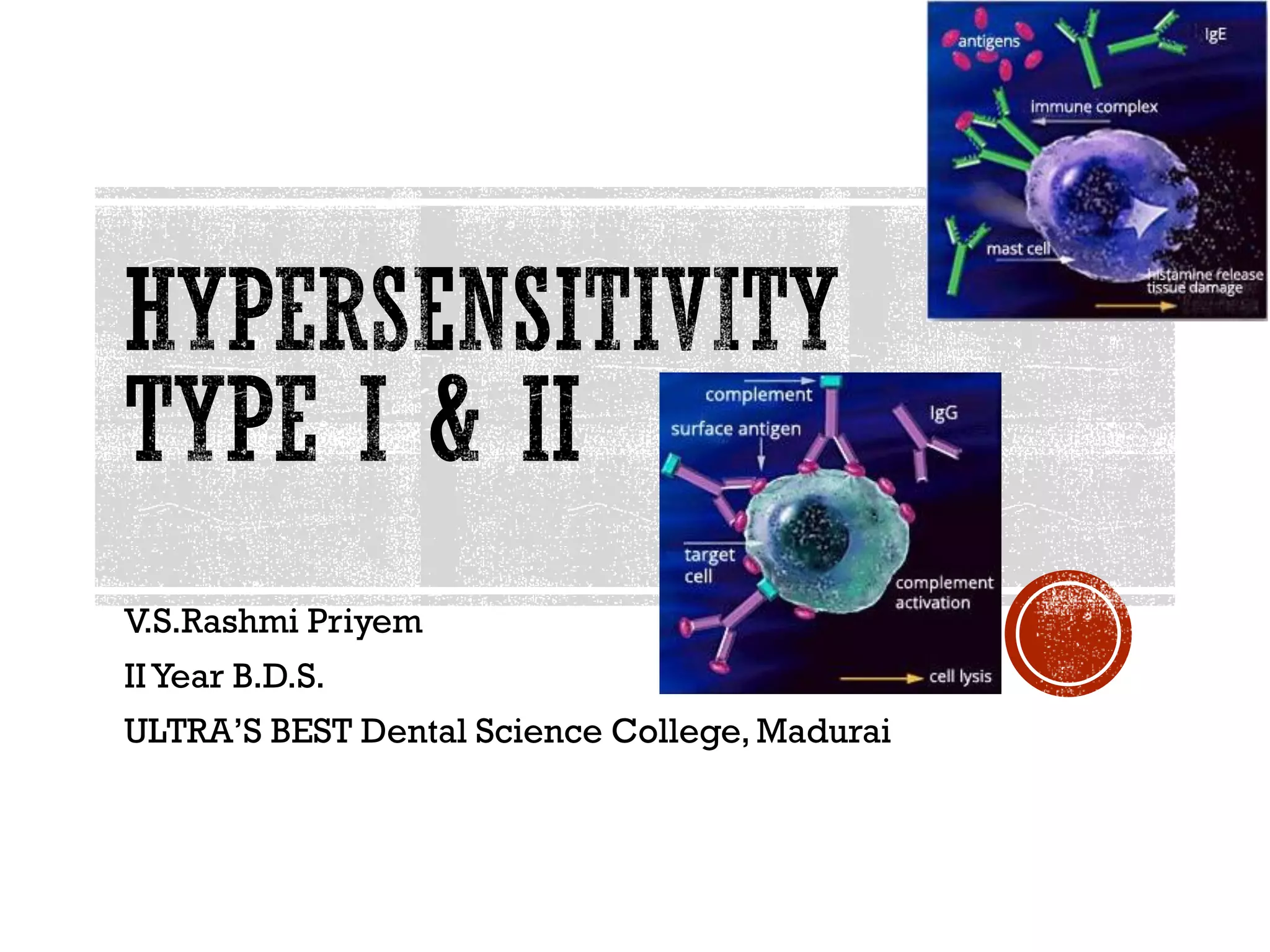
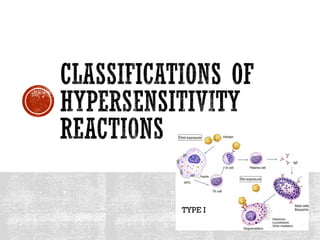
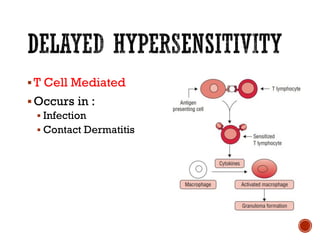
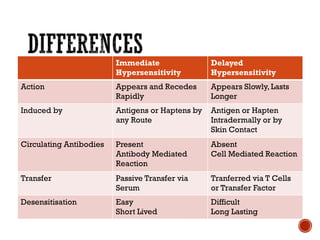
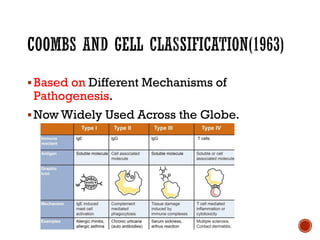
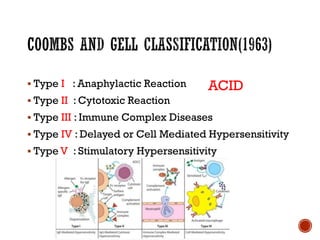
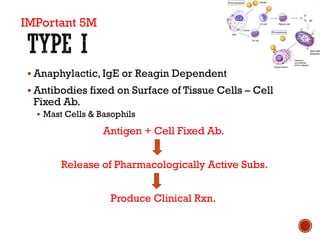
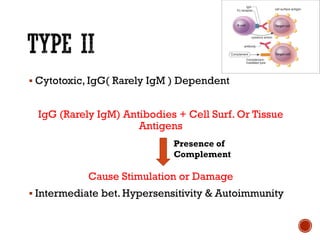
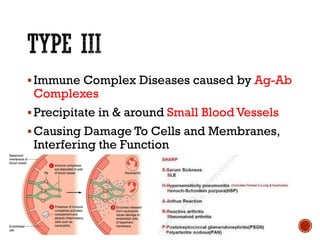
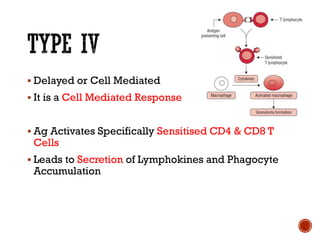
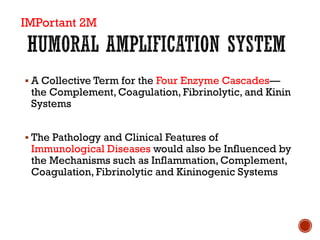
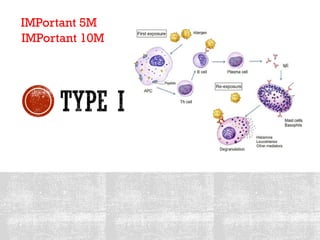
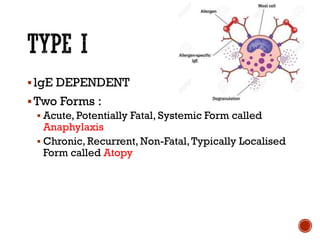
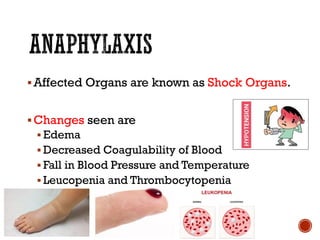
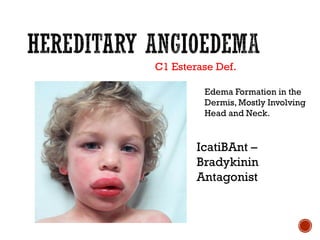
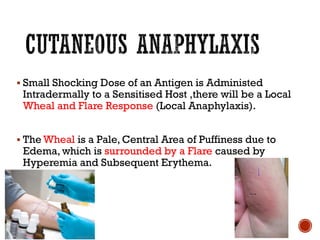
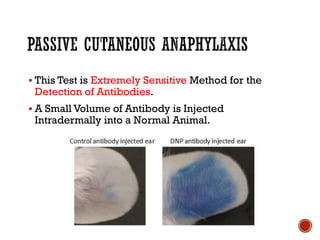
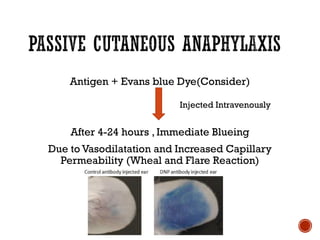
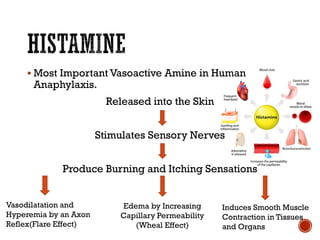
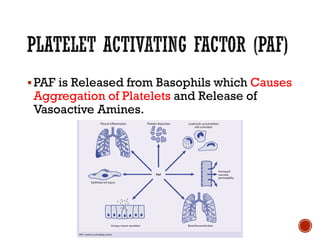
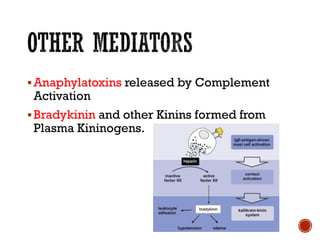
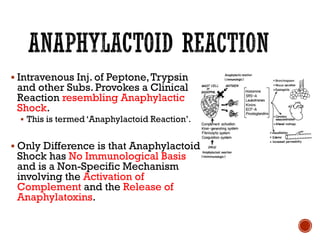
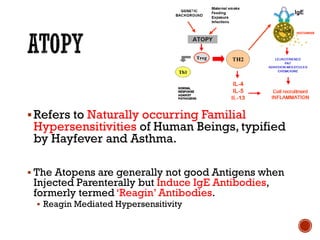
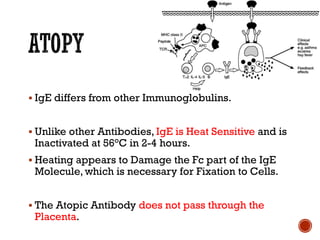
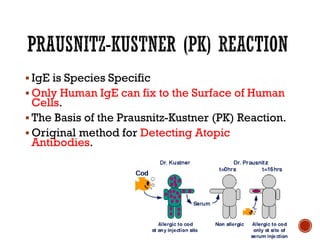
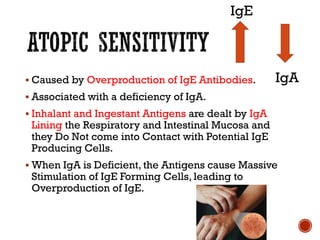
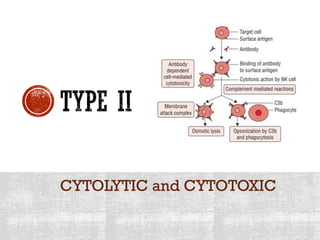
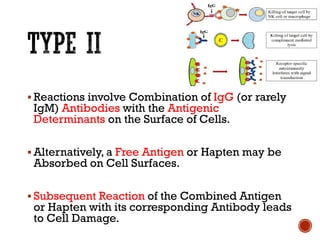
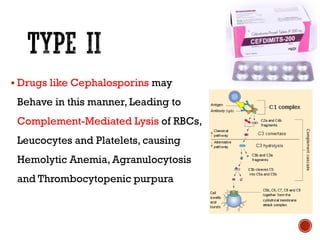
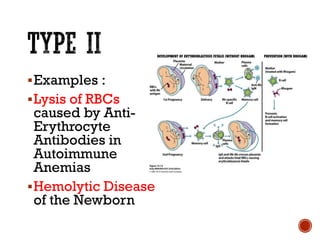
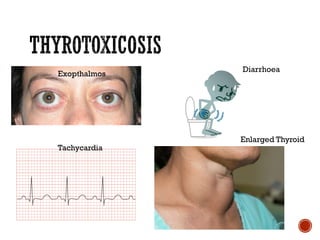
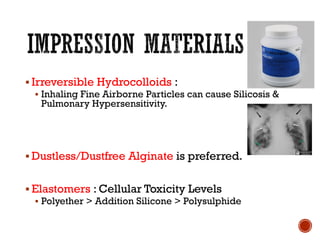
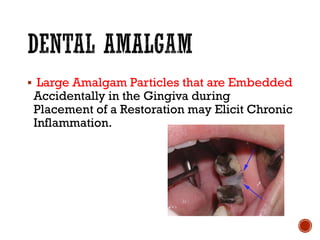
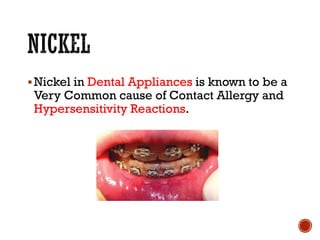
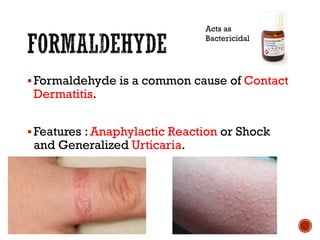
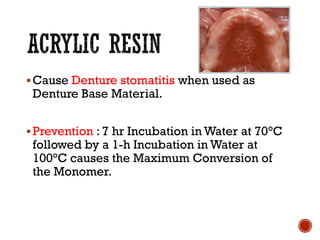
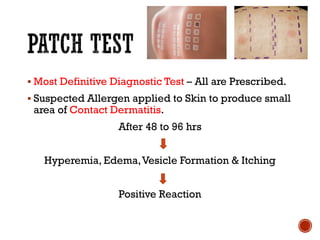
This document discusses hypersensitivity reactions and their classification. It begins by describing Type I reactions, which are immediate and antibody-mediated, including anaphylaxis and atopy. Type II are cytotoxic reactions mediated by IgG antibodies. Type III are immune complex diseases caused by antigen-antibody complexes. Type IV are delayed or cell-mediated hypersensitivity reactions. The document then discusses specific types of hypersensitivity reactions in more detail, including their mechanisms, clinical features, and importance in dentistry with certain materials, drugs, and allergens.