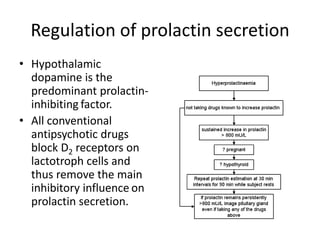
Hyperprolactinaemia, or elevated prolactin levels, is a common side effect of antipsychotic treatment. It is defined as a sustained prolactin level above the normal laboratory range, though there is variability in measurement. Many people with hyperprolactinaemia are asymptomatic and remain undiagnosed. All antipsychotics block dopamine receptors and remove the inhibitory influence on prolactin secretion, leading to symptoms like breast enlargement. Long-term risks include a small increased risk of breast cancer and osteoporosis, as evidenced by one study finding antipsychotic users were three times more likely to experience hip fractures.