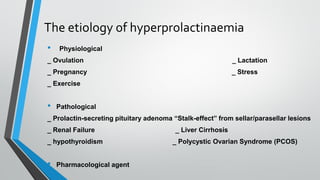
This document discusses causes and complications leading to hyperprolactinemia. It begins by introducing prolactin and its functions. Disturbances in prolactin regulation can cause hyperprolactinemia, which is a common problem. The most common causes are medications, sellar/parasellar masses (adenomas), physiological factors like pregnancy, and pathological factors like hypothyroidism. Treatment aims to reduce tumor size, resolve hyperprolactinemia symptoms, and prevent recurrence or progression through dopamine agonists, surgery, or radiotherapy.
![The etiology of hyperprolactinaemia
• Polycystic Ovarian Syndrome
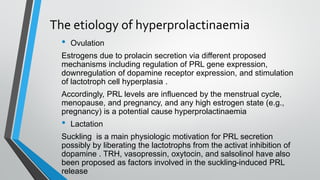
Hyperprolactinaemia has been reported in 7 to 52% of women with
polycystic ovarian syndrome
(PCOS) . Its pathogenesis has not been elucidated; oestrogen-
mediated stimulation of lactotrophs and relative dopamine
deficiency have been proposed . Given the presence of PRL
receptors in the adrenal gland [8], it has also been postulated that
hyperprolactinaemia stimulates adrenal androgen production
contributing to the hyperandrogenism of PCOS.](https://image.slidesharecdn.com/hyperprolactinom-210625134325/85/Hyperprolactinoma-17-320.jpg)