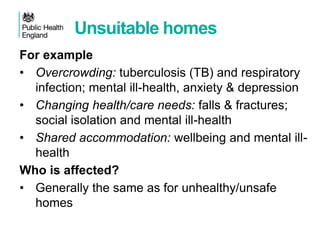
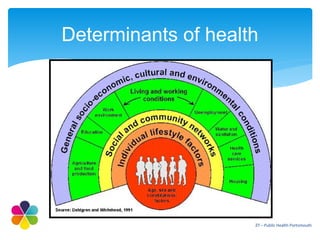
The document outlines discussions from a seminar on the relationship between housing and health, emphasizing the importance of social housing in improving health outcomes. It highlights various health indicators affected by housing conditions and proposes integrated approaches to tackle health inequalities through collaborative efforts between health and housing sectors. Case studies illustrate the practical application of these strategies in improving community wellbeing, particularly in deprived areas.