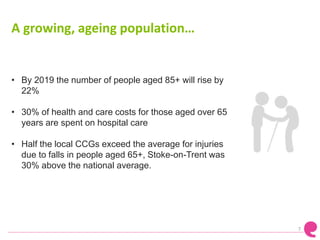
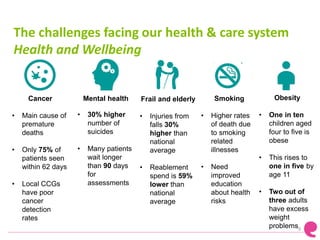
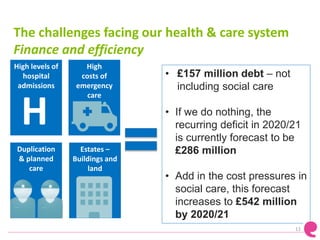
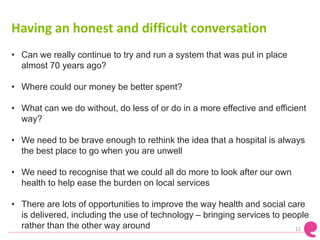
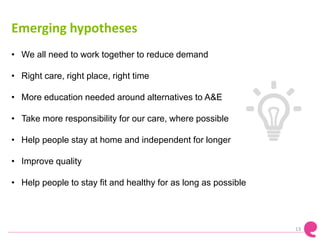
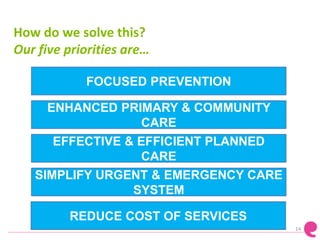
The document discusses challenges facing local health and social care services in Staffordshire and Stoke-on-Trent, including an aging population with complex needs, high costs, and quality issues. It outlines priorities to address these challenges through focused prevention, enhanced primary care, effective planned care, simplified urgent care, and reduced costs. New models of coordinated, community-based care are proposed to deliver more services outside hospitals and make the system more sustainable. Feedback from the public is sought to help inform future plans and decisions.