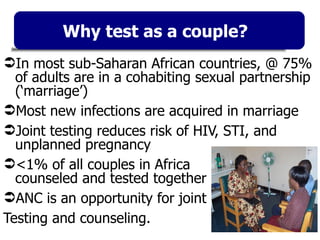
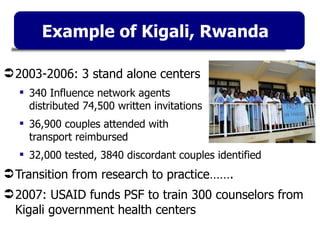
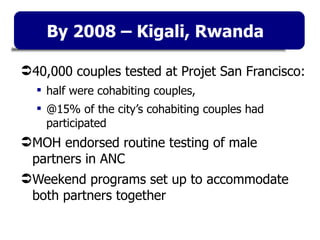
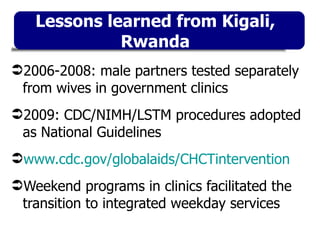
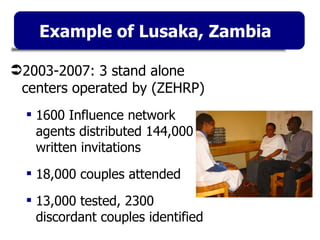
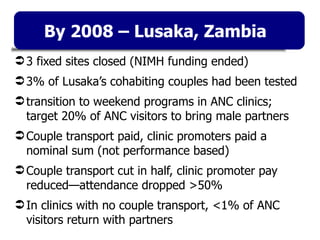
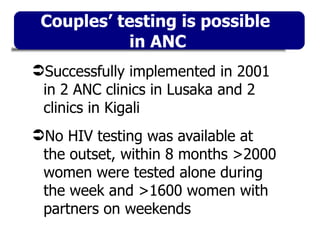
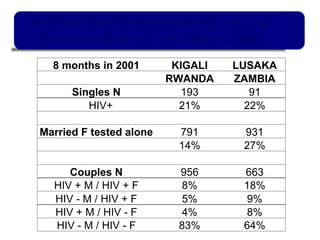
- The document discusses strategies for HIV testing of couples in sub-Saharan Africa, where most new infections occur within marriages. It highlights examples from Rwanda and Zambia where stand-alone and integrated testing of couples at antenatal clinics identified thousands of discordant couples.
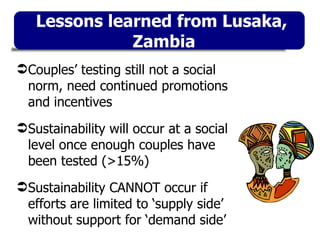
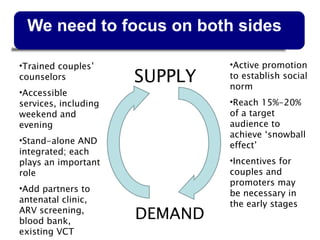
- Sustaining couples testing requires addressing both supply of testing services and demand through community promotion to establish it as a social norm. It takes testing 15-20% of target couples to achieve this. Incentives for transport and clinic promoters may be initially needed.