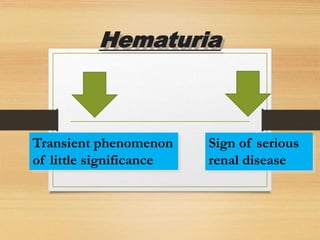
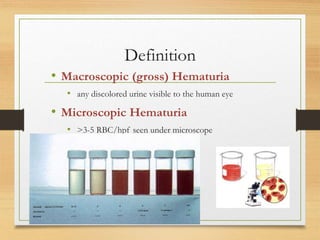
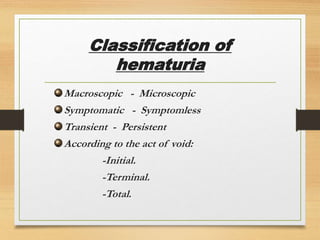
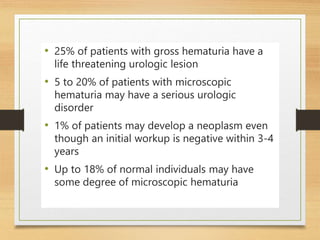
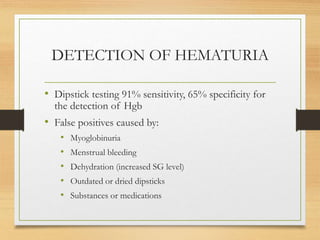
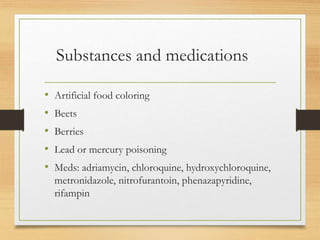
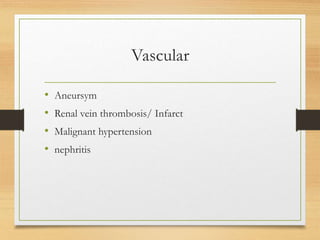
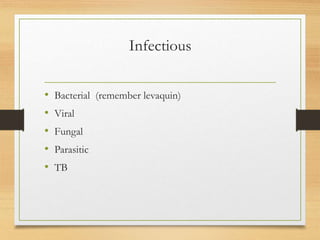
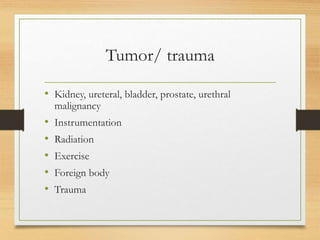
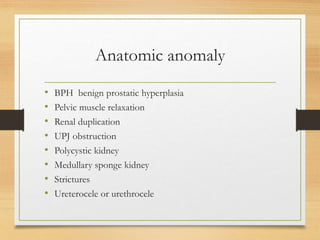
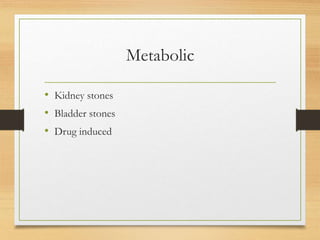
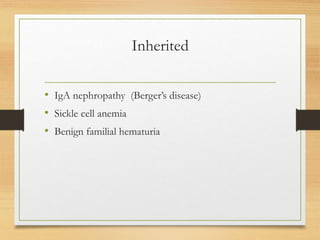
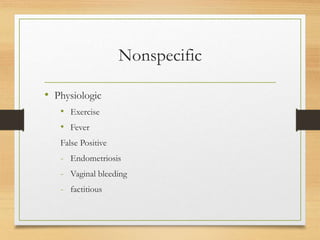
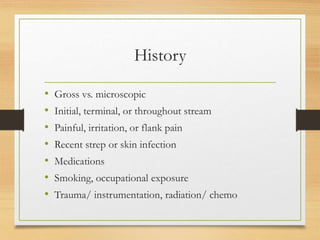
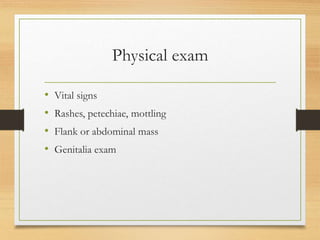
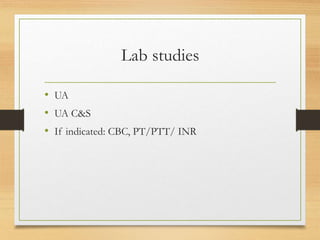
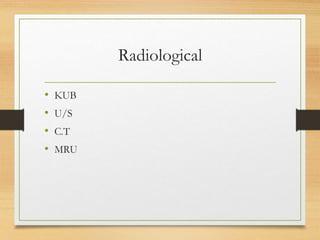
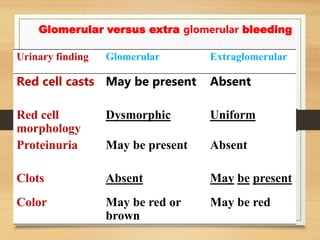
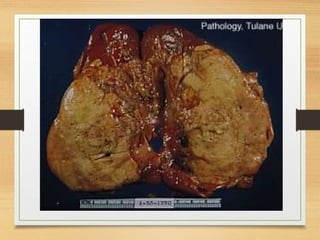
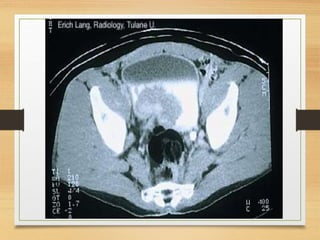
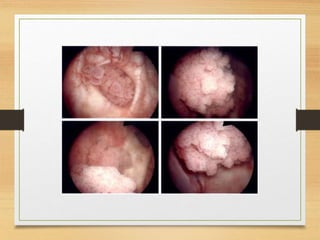
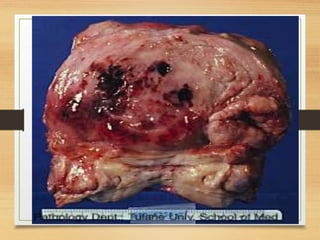
This document discusses hematuria, or blood in the urine. It defines macroscopic and microscopic hematuria and describes how hematuria can be classified. Common causes of hematuria are discussed, including stones, infections, tumors, trauma, vascular issues, anatomical anomalies, and inherited conditions. Evaluation of hematuria involves urine analysis, urine culture, imaging like ultrasound or CT, and possible cystoscopy. Follow up is usually needed due to risk of underlying malignancy. Four case examples are presented.