This presentation focuses on Acute Myeloid Leukemia (AML) with a special emphasis on the diagnostic aspects relevant to medical laboratory students.
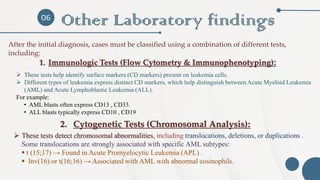
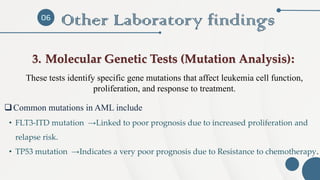
It provides a clear and concise overview of the disease's pathogenesis, risk factors, and initial clinical signs, along with a detailed review of the laboratory tests used in diagnosis, including complete blood count (CBC), peripheral blood smear, flow cytometry, and cytogenetic and molecular testing. The role of laboratory investigations in identifying genetic mutations and their impact on treatment planning is also highlighted.