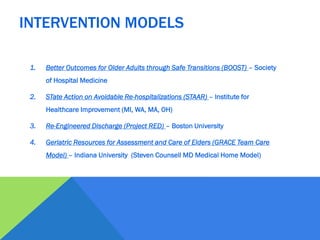
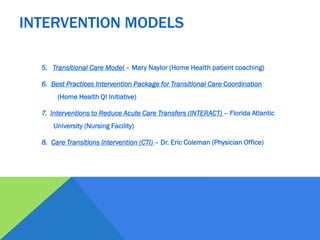
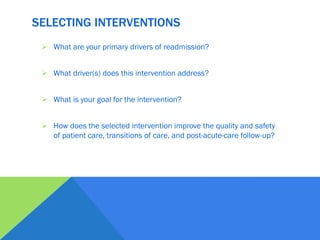
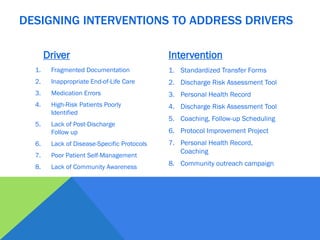
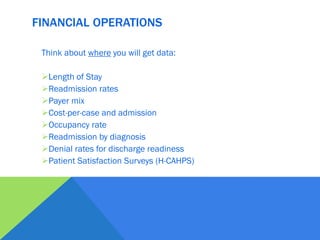
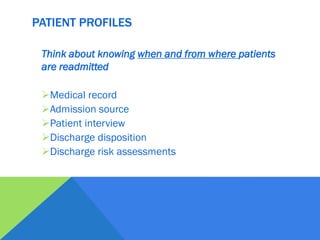
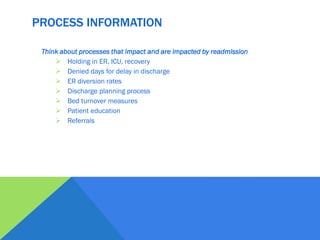
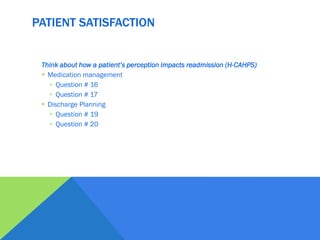
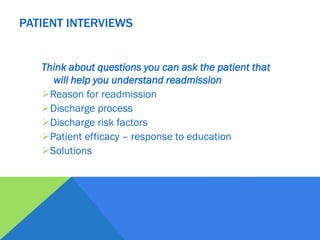
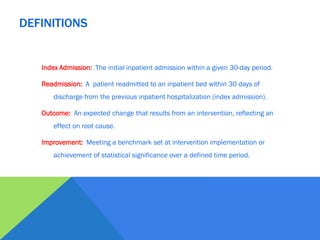
This document discusses strategies for reducing avoidable hospital readmissions. It begins by posing key questions around barriers to care transitions and potential interventions. It then lists common drivers of readmissions such as fragmented care, medication issues, and lack of follow up. The document outlines various evidence-based intervention models and provides a template for selecting interventions that address specific drivers. It emphasizes the importance of monitoring progress through data collection and engaging stakeholders. Finally, it stresses that reducing readmissions requires collaboration across providers.