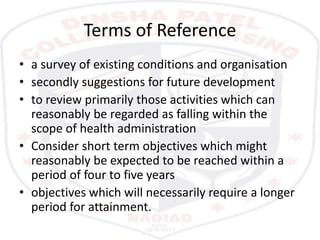
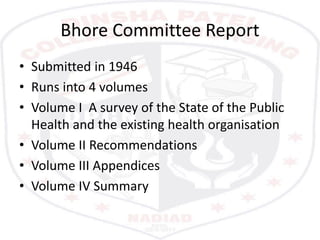
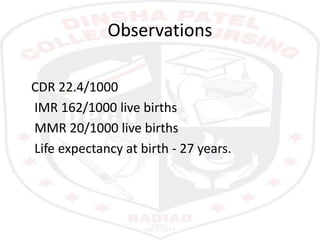
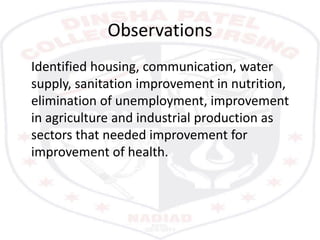
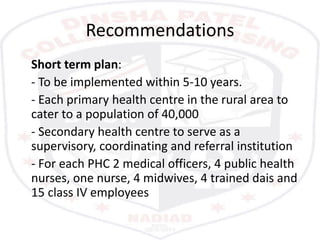
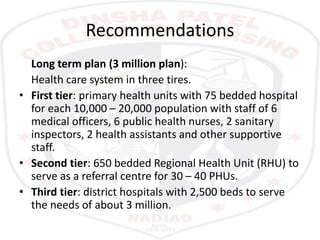
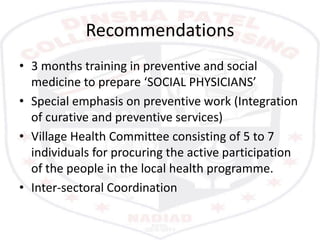
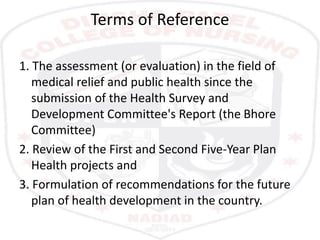
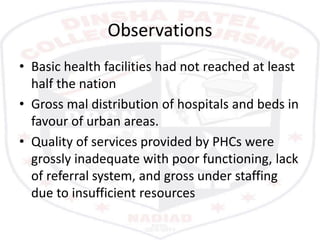
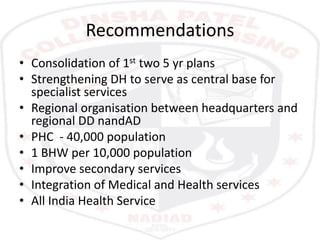
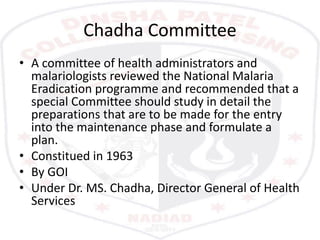
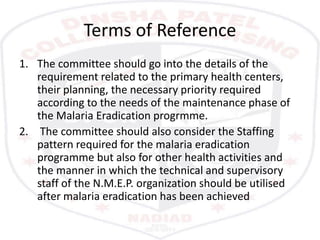
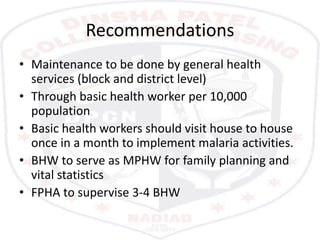
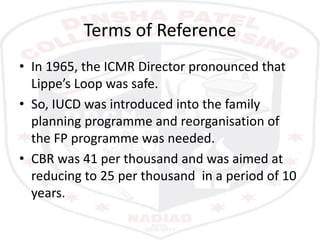
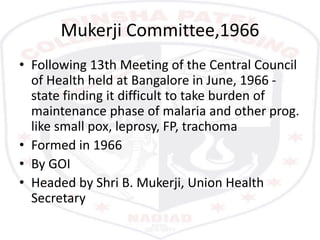
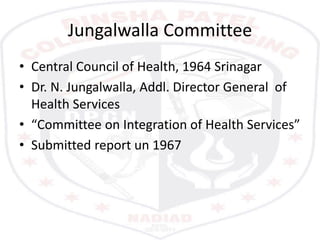
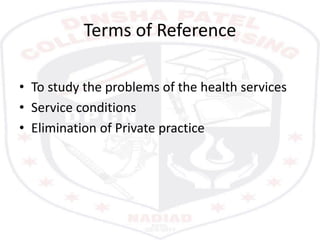
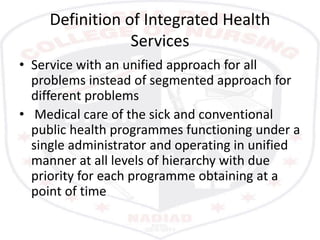
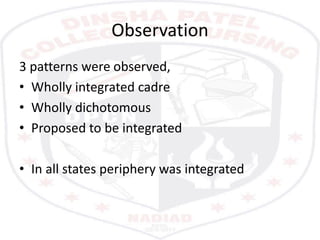
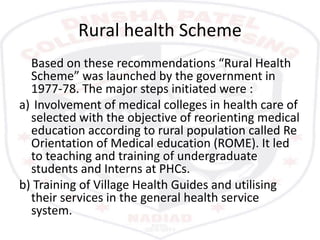
The Bhore Committee report from 1946 made several observations about India's poor health indicators at the time and made recommendations for improving health infrastructure. It proposed a three-tiered primary, secondary, and tertiary health system. Subsequent committees like the Mudaliar Committee and Mukerji Committee reviewed progress and recommended strengthening primary health centers and integrating health programs. The Chadha Committee focused on integrating malaria control into general health services after eradication. The Jungalwalla Committee studied problems with the health services and recommended full integration of medical care and public health programs under single administration.