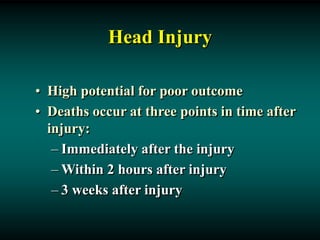
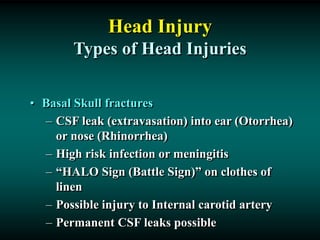
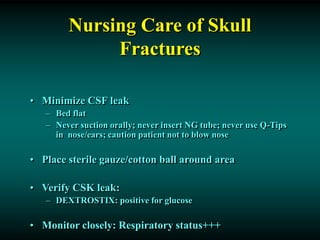
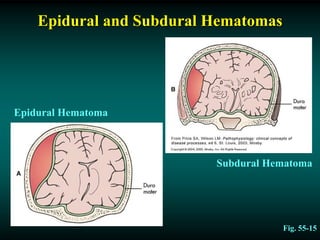
Head injuries can range from minor scalp lacerations to major trauma involving the brain. Common causes include motor vehicle accidents, falls, and assaults. Complications may include epidural or subdural hematomas. Diagnosis involves a CT or MRI scan. Nursing management focuses on maintaining adequate cerebral perfusion, preventing infection and secondary injury, and maximizing recovery of cognitive and physical function.