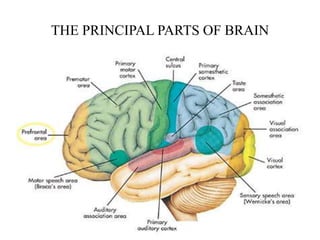
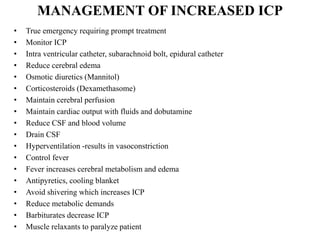
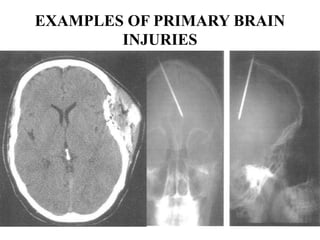
This document provides information about neurological nursing related to increased intracranial pressure and head injuries. It discusses the anatomy and physiology of the brain, types of head injuries including primary and secondary injuries, complications such as hematomas, and management of increased ICP. Nursing assessments, diagnoses, and interventions are also reviewed, including monitoring for signs of increased ICP, maintaining airway and breathing, preventing injury, and using the Glasgow Coma Scale to assess level of consciousness.