Genitourinary System Anatomy and Physiology..pptx
- 1. GENITOURINARY SYSTEM P R E S E N T E D B Y : PA L L AV I PAT H A N I A , P R O F E S S O R
- 2. INDEX S.NO. CONTENT 1. INTRODUCTION 2. DEFINITION 2. URINARY SYSTEM ORGANS 3. ANATOMY OF KIDNEY 4. ORGAN ASSOCIATED WITH THE KIDNEY 5. GROSS STRUCTURE OF KIDNEY 6. MICROSCOPIC STRUCTURE OF KIDNEY 7. MECHANISM OF KIDNEY 8. BLOOD SUPPLY OF KIDNEY
- 3. INDEX S.NO. CONTENT 10. NERVE SUPPLY AND LYMPHATIC DRAINAGE 11. THE URETERS 12. URINARY BLADDER 13. URETHRA 14. MICTURITION 15. FUNCTION OF KIDNEY 16. THE EFFECTS OF AGEING OF URINARY SYSTEM 17. Assessment of the urinary system 18. Renal system physical assesment 19. Radiographic studies 20. URINARY SYSTEM DISORDERS
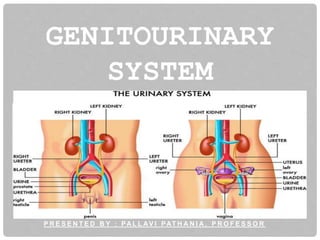
- 4. INTRODUCTION The urinary system, also known as the renal system. Urinary system, consists of: • The kidneys (two) • Ureters (two) • Bladder(one) • The urethra(one)
- 5. CONT.. • The function of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood PH. • The urinary system is the body's drainage system for the eventual removal of urine.
- 6. DEFINITION The system of organs comprising those concerned with the production and excretion of urine and those concerned with reproduction. Also known as genitourinary system, urogenital system, urogenital tract.
- 7. URINARY SYSTEM ORGANS URINARY SYSTEM CONSIST OF: Kidneys (2) Ureters (2) Urinary bladder Urethra
- 9. KIDNEY INTRODUCTION The human body normally has two pairs of kidneys, one on the left and one on the right. Kidney is a bean shaped structure with a convex and a concave border. The functional unit of kidney is nephron. The kidney produce urine that contains metabolic waste products, including the nitrogen compounds urea and uric acid, excess ions and some drugs.
- 10. LOCATION OF KIDNEYS LOCATION:- The kidney lies on the posterior abdominal wall, one on each side of the vertebral column, behind the peritoneum and below the diaphragm. Lateral to T12–L3 vertebrae. The right kidney being slightly lower and smaller than the left, and being placed slightly more to the middle than the left kidney.
- 11. CONT… STRUCTURE LENGTH: 11cm or 4.3 inch WIDTH: 6 cm THICK: 2.5-3 cm WEIGHT: Male:125 and 170 grams. Females:115 and 155 grams
- 12. ORGANS ASSOCIATED WITH THE KIDNEY RIGHT KIDNEY • Anteriorly: The duodenum, hepatic flexure of the colon & right lobe of the liver. • Posteriorly: Diaphragm, muscles of posterior abdominal wall. • Superiorly: The right adrenal gland.
- 13. ORGANS ASSOCIATED WITH THE KIDNEY LEFT KIDNEY • Anteriorly: The spleen & splenic vessels, jejunum splenic flexure of the colon, pancreas & stomach. • Posteriorly: Diaphragm, muscles of posterior abdominal wall. • Superiorly: The left adrenal gland.
- 14. GROSS STRUCTURE OF KIDNEY EXTENAL STRUCTURE Renal capsule Renal fascia Renal hilum INTERNAL STRUCTURE Renal cortex Renal medulla Renal pelvis
- 15. EXTERNAL STRUCTURE OF KIDNEY RENAL CAPSULE It is thin membrane sheath that covers the outer surface of each kidney. The capsule is composed of tough fibers, chiefly collagen and elastin(fibrous proteins) that helps to support kidney mass Protect the vital tissue from injury. RENAL FASCIA It is commonly known as Gerota's fascia. Is an connective tissue layer that helps adhere the kidney to surrounding structure.
- 16. CONT.. RENAL HILUM Is found at the medical concave surface Renal veins, renal artery and ureter are found in the hilum in anterior posterior order. Lymphatic and sympathetic nerves pass through the hilum
- 17. INTERNAL ANATOMY RENAL CORTEX • Outermost layer of kidney • Made up of 1.25, million of microscopic functional unit called nephron in each kidney. • Function: renal cortex produce erythropoietin.
- 18. INTERNAL ANATOMY RENAL MEDULLA Inner striated layer of kidney It contains renal pyramids that having striated cones. Base of each pyramid faces cortex while apex empty into the cup like cavity called calyx. Point of pyramid = Papilla Papilla nested in cup (minor calyx)8 – 18 Major calyx 2 – 3
- 19. CONT… RENAL COLUMNS Located between the pyramids Cortical tissue (cortex) RENAL PELVIS Funnel shaped structure at the beginning of ureter Calyx dumped into the renal pelvis
- 20. MICROSCOPIC STURCTURE OF KIDNEY The kidney is composed of about 1-2 millions functional units, the nephrons in each kidney, and a smaller number of collecting ducts. The collecting ducts transport urine through the pyramids to the calyces and renal pelvis. The collecting ducts are supported by a small amount of connective tissue, containing blood vessels, nerves and lymph vessels.
- 21. NEPHRONS NEPHRONS Functional units of kidney. Kidney contains about a million nephron. It is about 3cm long and 20nm in diameter. Nephrons are of two types: Cortical nephron Juxtamedullary nephron
- 22. NEPHRONS Nephrons consists of : Renal corpuscle • Glomerulus • Bowman’s capsule Renal tubule • Proximal convoluted tubule • Loop of henle • Distal convoluted tubule • Collecting ducts Renal blood vessels
- 23. RENAL CORPUSCLE Composed of a glomerulus and the Bowman's capsule. The renal corpuscle is the beginning of the nephron. It is the nephron's initial filtering component.
- 24. GLOMERULUS The glomerulus is surrounded by Bowman’s capsule. The glomerulus is a capillary tuft that receives its blood supply from an afferent arteriole of the renal circulation. It is a network of capillaries that performs the first step of filtering blood. The glomerular blood pressure provides the driving force for water and solutes to be filtered out of the blood and into the space made by Bowman's capsule.
- 25. CONT.. The remaining of the blood passes into the efferent arteriole. The diameter of efferent arterioles is smaller than that of afferent arterioles, increasing the hydrostatic pressure in the glomerulus.
- 26. CONT.. LAYERS OF GLOMERULUS:- Endothelial cells The endothelial cells of the glomerulus contain numerous pores. These pores are relatively large, they allow for the free filtration of fluid, plasma solutes and protein. Glomerulus basement membrane The Glomerulus basement membrane is a fusion of the endothelial cell and podocytes basal laminas
- 27. CONT.. Podocytes Podocytes line the other side of the glomerular basement membrane and form part of the lining of bowman’s space. Podocytes form a tight pedicels that control the filtration of protein.
- 28. BOWMAN'S CAPSULE The Bowman's capsule, also called the glomerular capsule. It surrounds the glomerulus. It is composed of a visceral inner layer formed by specialized cells called podocytes. Parietal outer layer composed of simple squamous epithelium. Fluids from blood in the glomerulus are filtered through the visceral layer of podocytes, resulting in the glomerular filtrate.
- 29. RENAL TUBULE Arises from glomerular capsule. Ends at tip of medullary pyramid. ~3 cm long. Four major regions Proximal convoluted tubule Loop of henle Distal convoluted tubule Collecting duct
- 30. PROXIMAL CONVOLUTED TUBULE (PCT) Filtered fluid collected by Bowman’s capsule enters into the PCT. It is called convoluted due to its tortuous path. Simple cuboidal cells form this tubule with prominent microvilli on the luminal surface, forming a brush border.
- 31. PROXIMAL CONVOLUTED TUBULE (PCT) • These microvilli create a large surface area to maximize the absorption and secretion of solutes (Na+, Cl–, glucose, etc.), the most essential function of this portion of the nephron.
- 32. LOOP OF HENLE U-shaped tube that consist of descending limb and ascending limb. Begin in the cortex, receiving filtrate from the PCT, extend into the medulla, and then return to the cortex to empty into the DCT.
- 33. LOOP OF HENLE The main function of the loop of henle is to reabsorb water from the urine The ascending limb Nacl into the surrounding tissue, not permeable to water Descending limb is permeable to water Water flows out of the filtrate in this area due to osmosis (high salt concentration all around).
- 34. DISTAL CONVOLUTED TUBULE (DCT) It is highly coiled part of nephron Variably active portion of the nephron. Receive , dilute fluid from the ascending limb of the loop of henle
- 35. COLLECTING DUCT Collecting duct is variably active portion of the nephron. It is lined by specialized cuboidal epithelial with very few microvilli. DCTs of several nephrons empty into a collecting duct. Passes into medulla. Several merge into papillary duct (~30 per papilla). Drain into minor calyx.
- 36. MECHANISM OF KIDNEY FORMATION OF URINE Formation of urine, which passes to bladder for storage prior to excretion. The kidneys filter unwanted substances from the blood and produce urine to excrete them.
- 37. STEPS OF URINE FORMATION There are three main steps of urine formation: I. Glomerular filtration- solute enter nephrons from the blood II. Reabsorption—some solutes are selectively reabsorbed by the blood III. Secretion-additional solutes are secreted for elimination
- 38. I. FILTRATION Blood is carried to glomerulus by the afferent arteriole. Pressure in the glomerulus are very high 65mmhg, as compared with normal 25mm Hg Solute are filtered through glomerulus wall into bowman’s capsule
- 39. GLOMERULAR FILTRATION RATE The amount of filtrate formed in all the renal corpuscles of both kidneys each minute is the glomerular filtration rate (GFR). In adults male :125 mL/min and 105 mL/min in females. Three mechanisms control GFR: 1. Renal auto regulation. 2. Neural regulation: By Sympathetic division- Vasoconstriction 3. Hormonal regulation: a. Angiotensin II: vasoconstrictor b. Atrial Natriuretic Peptide (ANP) :
- 40. WHAT MATERIAL ARE FILTERED Yes No Water Nacl Glucose Amino acid Urea H+ Minerals Plasma proteins Erythrocytes(WBC’s) Platelets (minerals that are not filtered are too big to get through the membranes)
- 41. II. REABSORPTION. Solutes and water are selectively reabsorbed into blood transport (both active and passive) out of the nephron, into the interstitial fluid, and back into blood Reabsorption occurs until a maximum amount (the threshold level) has been transported. About 85% of filtered water is reabsorbed.
- 42. REABSORPTION 1. Active transport of NaCl from the ascending limb of the loop of henle. 2. Osmosis of water from the descending loop of henle causes concentration of filtrate. 3. Further active transport of NaCl from ascending loop of henle does two things: a. Decrease filtrate solute concentration b. Increases strength of osmotic gradient to pull H20 from descending loop of henle Therefore, the loop of henle actually achieves very little concentration of filtrate
- 43. REABSORPTION The main function of the loop of henle is to build up solute concentration in the interstitial space Concentration gradient drive the osmosis of water from the collecting duct The bulk of water reabsorption occurs here Concentrated urine is produced Unfiltered proteins in the bloodstream also contribute to osmotic gradient that pulls H2o from nephrons
- 44. WHAT SOLUTES ARE ACTIVELY REABSORBED? Solute Location Sodium ions, Na+ Cl- and HCO3 - follow by charge attraction Proximal tubule Ascending loop of henle (NaCl) glucose Proximal tubule Amino acid Proximal tubule
- 45. III. SECRETION Occurs in the distal tubule. Waste solute move from blood into the nephron Nitrogen- containing wastes, excess H+ and K+
- 46. COMPOSITION OF URINE • Water (96 %), • urea (2 %), • uric acid, • creatinine, • ammonia, • sodium, • potassium, • chlorides, • phosphates, • sulphates and oxalates (2 %). • Urine production is decreased during sleep and exercise.
- 48. CONT..
- 49. WATER BALANCE AND URINE OUTPUT The source of body water is dietary food and fluid and small amount is formed by metabolic processes. Excretion of water take place in the form of faces, sweat and as the main constituent of urine. The balance between fluid intake and output is controlled by the kidneys. The minimum urinary output is about 500 ml per day. The excess amount produced is controlled by antidiuretic hormone (ADH) released into the blood by posterior lobe of pituitary gland.
- 50. WATER BALANCE
- 51. WATER BALANCE Sensory nerve cells in the hypothalamus (osmoreceptors) detect changes in the osmotic pressure of the blood. Nerve impulses from the osmoreceptors stimulate the posterior lobe of the pituitary gland to release ADH. When the osmotic pressure is raised, ADH output is increased and as a result, water reabsorption by the cells in distal convoluted tubules and collecting ducts is increased, reducing the blood osmotic pressure and ADH output.
- 52. WATER BALANCE When blood volume is increased, stretch receptors in the atria of the heart release atrial natriuretic hormone (ANP). This reduces reabsorption of sodium and water by PCT and collecting ducts, meaning that are more sodium and water are excreted. In turn this reduces blood volume
- 53. WATER BALANCE (atrial natriuretic hormone)
- 54. ELECTROLYTE BALANCE The changes in electrolytes concentration may occurs due to changes in: Body water content or Electrolyte levels Sodium and potassium concentration Sodium is the positively charged cation in ECF and potassium is negatively charged found most commonly in ICF. Sodium is a constituent of almost all foods and it is added to food during cooking. It is excreted mainly in urine & sweat. Sodium is the normal constituent of urine and amount excreted is regulated by aldosterone hormone, secreted by the adrenal cortex.
- 55. ELECTROLYTE BALANCE The cells of kidney are stimulated to produce renin enzyme by sympathetic stimulation, low blood volume or low blood pressure Renin converts the plasma angiotensinogen (liver)to angiotensin-I Angiotensin converting enzyme (ACE), formed in the lungs converts angiotensin-I into angiotensin-II which is a potent vasoconstrictor and increases the blood pressure. Water is reabsorbed with sodium and together they increase the blood volume and blood pressure.
- 56. ELECTROLYTE BALANCE When sodium reabsorption is increased, potassium excretion is increased, indirectly reducing intracellular potassium. Normally the renal mechanism maintains the concentration of sodium and potassium within the physiological limits. Sodium and potassium occur in high concentrations indigestive juices - sodium in gastric juice and potassium in pancreatic & intestinal juice. Normally these ions are reabsorbed by the colon but following acute & prolonged diarrhoea they may be excreted in large quantities with results in electrolyte imbalance.
- 58. RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM Stimuli that initiate the renin–angiotensin–aldosterone pathway include dehydration, Na+ deficiency or hemorrhage. These conditions cause a decrease in blood volume. Decreased blood volume leads to decreased blood pressure. Lowered blood pressure stimulates juxtaglomerular cells of kidney, to secrete the enzyme renin. The level of renin in blood increases. Renin converts angiotensinogen, plasma protein produced by the liver, into angiotensin 1. blood containing increased levels of angiotensin 1 circulates in the body.
- 59. RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM Angiotensin converting enzyme (ACE) in the lungs converts angiotensin 1 into angiotensin 2. Angiotensin 2 stimulates the adrenal cortex to secrete aldosterone. In the kidneys, aldosterone increases reabsorption of Na+ and water and increases secretion of K+ and H+ into the urine. With increased water reabsorption by the kidneys, blood volume increases. As blood volume increases, blood pressure increase to normal. Angiotensin-II also stimulate concentration of smooth muscle in the walls of arterioles. The resulting vasoconstriction of the arterioles increase blood pressure.
- 60. ACID –BASE BALANCE In order to maintain the normal pH of blood, the cells of PCT secrete hydrogen ions. In the filtrate they combine with buffers: Hydrogen ions + Bicarbonate = Carbonic acid (H++ HCO3--»H2C03) Hydrogen ions + Ammonia = Ammonium ions (H+ + NH3 --» NH+4) Hydrogen ions +Hydrogen phosphate = Dihydrogen phosphate (H+ + HPO23---» H2PO3-)
- 61. ACID –BASE BALANCE Carbonic acid is converted to carbon dioxide (CO2) and water(H2O), and the CO2 is reabsorbed maintaining the buffering capacity of the blood. Hydrogen ions are excreted in the urine as ammonium salts & hydrogen phosphate. The normal pH of urine varies from 4.5 to 8 depending on diet, time & variety of other factors.
- 62. BLOOD SUPPLY OF KIDNEY Arterial supply by Renal artery, branches of abdominal aorta Vein drain from kidney through renal vein to Inferior vena cava
- 63. BLOOD SUPPLY OF KIDNEY FLOW CHART
- 64. NERVE SUPPLY AND LYMPHATIC DRAINAGE NERVE SUPPLY- Renal plexus, an offshoot of coeliac plexus. It contains postganglionic fibers from the sympathetic nervous system (T10 to L1) which are Afferent nerves of kidney belong to segment T10-T12. LYMPHATIC DRAINAGE- Lymphatic drain into the lateral aortic lymph nodes which are located at level of origin of renal arteries.
- 65. THE URETERS
- 66. THE URETERS The ureters carry urine from the kidneys to urinary bladder. Length :25-30 cm long Diameter : 3mm. The ureters is continuous with funnel shaped renal pelvis.
- 67. THE URETERS It passes down through the abdominal cavity, behind the peritoneum in front of psoas muscle into pelvic cavity , and passes obliquely through the posterior wall of the bladder. This arrangement as urine accumulate and the pressure in the bladder rises, the ureters are compressed and the openings into the bladder are occluded
- 68. STRUCTURE OF URETERS Consists of 3 layers of tissue: An outer covering of fibrous tissue. A middle muscular layer consisting of interlacing smooth muscle fibres. An inner layer, the mucosa, composed of transitional epithelium.
- 69. FUNCTION Propel urine from the kidneys into the bladder by peristaltic contraction of the smooth muscle layer. Occurs several times per minute, increasing in frequency with the volume produced.
- 70. URINARY BLADDER
- 71. URINARY BLADDER A hollow, muscular, pear shaped organ for storage of urine. Can stored up to 500 ml of urine. Lies in the pelvic cavity. When distended, the bladder rises into the abdominal cavity. Voiding takes place by contractions of the bladder, which forces urine through the urethra and to the outside opening, the urinary meatus.
- 72. ORGAN ASSOCIATED TO URINARY BLADDER
- 73. SHAPE OF BLADDER An empty bladder is 4 sided pyramid in shape and has • 4 Angles- an apex, neck and 2 lateral angles • 4 surfaces • Base (posterior surface) • 2 Inferio-lateral surface • Superior surface When distended it is ovoid in shape
- 75. STRUCTURE The bladder wall is composed of three layers: • The outer layer of • loose connective tissue, containing blood lymphatic vessels and nerves. • The middle layer • smooth muscle fibers and elastic tissue , this is called the destrusor muscle and when it contracts, it empties the bladder. • The inner mucosa, • composed of transitional epithelium that readily permits distension of the bladder as it fills
- 76. INTERIOR OF BLADDER The mucous membrane is straw colored and is thrown into folds. when bladder is distended, these folds disappear The posterior wall shows a smooth triangular area called trigone. There are no mucous fold in this region. At the upper lateral angles of the trigone are the ureteric opening At its inferior angle is the internal urethral of orifice.
- 79. URETHRA • The urethra is canal extending from the neck of the bladder to the exterior, at the external urethral orifice. It is longer in the male than in the female.
- 80. FEMALE URETHRA 3 to 4 cm long External urethral orifice between vaginal orifice and clitoris Internal urethral sphincter detrusor muscle thickened, smooth muscle, involuntary control. External urethral sphincter skeletal muscle , voluntary control The mucosa is supported by loose fibroblastic connective tissue containing blood vessels and nerves
- 81. MALE URETHRA 18 cm long Internal urethral sphincter External urethral sphincter 3 regions Prostatic urethra During organism receives semens Membranous urethra passes through pelvic cavity Penile urethra
- 83. MICTURITION Micturition is a process by which urinary bladder empties when it becomes filled. When smooth muscle in the wall of the bladder stretches, the micturition reflex (urination) is triggered. Begins in 5 month of uterine life. Remain reflex up to 2-21/2 year of age. i. Filling of bladder- progressively till the tension of the wall rise above threshold. ii. Emptying of bladder-nervous reflex-micturition reflex that emptied the bladder or at least conscious desire of urination.
- 84. MICTURITION Urine produced in the kidneys travels down the ureters into the urinary bladder. The bladder expands like an elastic sac to hold more urine. As it reaches capacity, the process of micturition, or urination, begins. Involuntary muscle movements send signals to the nervous system, putting the decision to urinate under conscious control.
- 85. MICTURITION The internal urethral sphincter and the external urethral sphincter both provide muscle control for the flow of urine. The internal sphincter is involuntary. It surrounds the opening of the bladder to the urethra and relaxes to allow urine to pass. The external sphincter is voluntary. It surrounds the urethra outside the bladder and must be relaxed for urination to occur.
- 86. MICTURITION • The bladder is shaped like a pyramid when empty. It becomes more oval as it fills with urine and expands. A smooth muscle called the detrusor surrounds the bladder, and folds called rugae line the interior wall. These structures give the bladder elasticity and allow it to expand. The floor of the bladder includes a funnel-like region called the trigone, formed by the two ureteral orifices and the internal urethral sphincter. Urine flows into the bladder via the ureteral orifices and out through the internal sphincter.
- 87. MICTURITION Micturition, or urination, is the act of emptying the bladder. When the bladder is full of urine, stretch receptors in the bladder wall trigger the micturition reflex. The detrusor muscle that surrounds the bladder contracts. The internal urethral sphincter relaxes, allowing for urine to pass out of the bladder into the urethra. Both of these reactions are involuntary. The external urethral sphincter is voluntary. It must be relaxed for urine to flow through the urethra and outside the body.
- 88. MICTURITION The bladder expands as urine flows in from the ureters, but there is a limit to the volume it can contain. At about 200 ml of urine, the detrusor muscle begins to contract and the internal urethral sphincter muscle begins to relax. This sends signals through the nervous system and creates the “urge” to urinate. If this urge is ignored, continence may be threatened. At about 500 ml, detrusor muscle contractions begin to force open the internal urethral sphincter. Unless the external urethral sphincter is powerful enough to prevent it, micturition (urination) will occur involuntarily.
- 89. MICTURITION Smooth muscle stretch initiates the micturition reflex by activating stretch receptors in the bladder wall. This autonomic reflex causes the detrusor muscle to contract and the internal urethral sphincter muscle to relax, allowing urine to flow into the urethra. The stretch receptors also send a message to the thalamus and the cerebral cortex, giving voluntary control over the external urethral sphincter. We usually gain this control of urination between the ages of 2 and 3, as our brains develop.
- 91. FUNCTION OF KIDNEY Excretory function Homeostatic function Endocrine function Metabolic function
- 92. EXCRETORY FUNCTION • This include formation and excretion of urine. • The main step involved are – Glomerular filtration – Tubular reabsorption – Tubular secretion
- 93. HOMEOSTATIC FUNCTIONS OF URINARY SYSTEM 1. Regulate blood volume and blood pressure: • by adjusting volume of water lost in urine • releasing erythropoietin and renin 2. Regulate plasma ion concentrations: • sodium, potassium, and chloride ions (by controlling quantities lost in urine) • calcium ion levels
- 94. CONT.. 3. Help stabilize blood pH: by controlling loss of hydrogen ions and bicarbonate ions in urine 4. Conserve valuable nutrients: by preventing excretion while excreting organic waste products
- 95. ENDOCRINE FUNCTIONS… Kidneys have primary endocrine function since they produce hormones In addition, the kidneys are site of degradation for hormones such as insulin and aldosterone. In their primary endocrine function, the kidneys produce erythropoietin, renin and prostaglandin. Erythropoietin is secreted in response to a lowered oxygen content in the blood. It acts on bone marrow, stimulating the production of red blood cells.
- 96. CONT.. Renin -the primary stimuli for renin release include reduction of renal perfusion pressure and hyponatremia. Renin release is also influenced by angiotensin II and ADH. It is a key stimulus of aldosterone release. The effect of aldosterone is predominantly on the distal tubular network, effecting an increase in sodium reabsorption in exchange for potassium. The kidneys are primarily responsible for producing vitamin D3 from dihydroxycholecalciferol
- 97. THE EFFECTS OF AGEING ON URINARY SYSTEM The kidney have a substantial functional reserve; the loss of one kidney does not cause problems in an otherwise healthy individual. The number of nephrons declines with the age, glomerular filtration rate falls and the renal tubules function less efficiently; the kidneys become less able to concentrate urine.
- 98. THE EFFECTS OF AGEING OF URINARY SYSTEM Elimination of drugs also becomes less efficient with declining kidney function which may lead to accumulation and toxicity. The ability to inhibit contraction of detrusor muscle declines may result in urgent need to pass urine and urinary frequency . Nocturia becomes increasingly common in older adults Blood vessels supplying the kidney can become hardened. This causes kidney to filter blood more slowly. The bladder muscle weakened.
- 99. THE EFFECTS OF AGEING OF URINARY SYSTEM IN MALE • The urethra can become blocked by enlarged prostate gland. • such as leakage or urinary incontinence (not being able to hold your urine), or urinary retention (not being able to completely empty your bladder) IN FEMALE • The urethra can become partially or totally blocked. • This can be due to weakened muscles that can cause the bladder or vagina to fall out of position(prolapse).
- 101. INTAKE AND OUTPUT CHART
- 103. ANURIA
- 104. OLIGURIA
- 105. ASSESSMENT OF THE URINARY SYSTEM Safety considerations: • Perform hand hygiene. • Introduce yourself to patient. • Confirm patient ID using two patient identifiers (e.g., name and date of birth). • Explain process to patient. • Be organized and systematic in your assessment. • Use appropriate listening and questioning skills. • Listen and attend to patient cues. • Ensure patient’s privacy and dignity.
- 106. • Nursing Assessment • History of UTI and other disease, Age , Pain location, duration, fever, chills, hematuria, renal calculi, vaginal infections, discharge, contraceptive practices etc. • Assess for the following subjective and objective data: • Decreased urine output or oliguria (reduced urine volume) • Swelling or edema in the hands, feet, or face • Fatigue and weakness • Shortness of breath or difficulty breathing • Nausea, vomiting, or loss of appetite • Confusion or altered mental status • Abdominal pain or discomfort • High blood pressure • Irregular heart rhythm or palpitations • Signs of fluid overload
- 107. ASSESSMENT • Assessment and monitoring of renal function • Fluid and electrolyte balance management • Identification and treatment of the underlying cause • Prevention and management of complications (e.g., electrolyte imbalances, metabolic acidosis) • Monitoring and management of fluid overload or dehydration • Hemodynamic stability and blood pressure control • Education on self-care and compliance with treatment plans
- 108. PHYSICAL EXAMINATION • A careful history and assessment of symptoms will suggest whether a complete or limited examination is indicated, and also help direct the appropriate selection of subsequent diagnostic studies. • Inspection: A mass that is visible in the upper abdominal area may be difficult to palpate if soft, as with hydronephrosis. Fullness in the costovertebral angle may be consistent with cancer or perinephric infection. The presence and persistence of indentations in the skin from lying on wrinkled sheets suggest edema of the skin secondary to perinephric abscess. • Palpation: The kidneys lie rather high under the diaphragm and lower ribs and are therefore well protected from injury. Because of the position of the liver, the right kidney is lower than the left. The kidneys are difficult to palpate in men because of (1) resistance from abdominal muscle tone and (2) more fixed position than in women, moving only slightly with change of posture or respiration. The lower part of the right kidney can sometimes be felt, particularly in thin patients, but the left kidney usually cannot be felt unless it is enlarged or displaced. • The most successful method of renal palpation is carried out with the patient lying in the supine position on a hard surface (Figure 4–1). The kidney is lifted by one hand in the costovertebral angle (CVA). On deep inspiration, the kidney moves downward; the other hand is pushed firmly and deeply beneath the costal margin in an effort to trap the kidney. When successful, the anterior hand can palpate the size, shape, and consistency of the organ as it slips back into its normal position.
- 109. PHYSICAL EXAMINATION Method of palpation of the kidney. The posterior hand lifts the kidney upward. The anterior hand feels for the kidney. The patient then takes a deep breath; this causes the kidney to descend. As the patient inhales, the fingers of the anterior hand are plunged inward at the costal margin. If the kidney is mobile or enlarged, it can be felt between the two hands.
- 110. PHYSICAL EXAMINATION • Alternatively, the kidney may be palpated with the examiner standing behind the seated patient. At other times, if the patient is lying on one side, the uppermost kidney drops downward and medially, making it more accessible to palpation. Perlman and Williams (1976) described an effective method of identifying renal anomalies in newborns. The fingers are placed in the costovertebral angle, with the thumb anterior and performing the palpation. • An enlarged renal mass suggests compensatory hypertrophy (if the other kidney is absent or atrophic), hydronephrosis, tumor, cyst, or polycystic disease. However, a mass in this area may also represent a retroperitoneal tumor, spleen, lesion of the bowel (eg, tumor, abscess), lesion of the gallbladder, or pancreatic cyst. Tumors may have the consistency of normal tissue ... •
- 111. PHYSICAL EXAMINATION • Physical examination focuses on the costovertebral angle, abdomen, rectum, groin, and genitals. In women with urinary symptoms, pelvic examination is usually done. • Costovertebral angle • Pain elicited by blunt striking of the back, flanks, and angle formed by the 12th rib and lumbar spine with a fist (costovertebral tenderness) may indicate pyelonephritis, calculi, or urinary tract obstruction. • Abdomen • Visual fullness of the upper abdomen is an extremely rare and nonspecific finding of a kidney or abdominal mass. Dullness to percussion in the lower abdomen suggests bladder distention; normally, even a full bladder cannot be percussed above the symphysis pubis. Bladder palpation can be used to confirm distention and urinary retention. • Rectum • During digital rectal examination, prostatitis may be detected as a boggy, tender prostate. Focal nodules and less discrete hard areas must be distinguished from prostate cancer. The prostate may be symmetrically enlarged, rubbery, and nontender with benign prostatic hyperplasia.
- 112. PHYSICAL EXAMINATION • Groin and genitals • Inguinal and genital examination should be done with patients standing. Inguinal hernia or adenopathy may explain scrotal or groin pain. Gross asymmetry, swelling, erythema, or discoloration of the testes may indicate infection, torsion, tumor, or other mass. Horizontal testicular lie (bell-clapper deformity) indicates increased risk of testicular torsion. Elevation of one testis (normally the left is lower) may be a sign of testicular torsion. The penis is examined with and without retracting the foreskin. Inspection of the penis can detect • Hypospadias or epispadias in young boys • Peyronie disease in men • Priapism, ulcers, and discharge in either group • Palpation may reveal an inguinal hernia. Cremasteric reflex may be absent with testicular torsion. Location of masses in relation to the testis and the degree and location of tenderness may help differentiate among testicular masses (eg, spermatoceles, epididymitis, hydroceles, tumors). If swelling is present, the area can be transilluminated to help determine whether the swelling is cystic or solid. Fibrous plaques felt in the penile shaft are signs of Peyronie disease.
- 113. TESTICULAR AND SELF EXAMINATION • Urinalysis is critical for evaluating urologic disorders. Imaging tests (eg, ultrasonography, CT, MRI) are frequently required. For semen testing, see Sperm Disorders. • Bladder tumor antigen testing for transitional cell cancer of the urinary tract is more sensitive than urinary cytology in detecting low-grade cancer; it is not sensitive enough to replace endoscopic examination. Urine cytology is the best test to detect high-grade cancer. • Prostate-specific antigen (PSA) is a glycoprotein with unknown function produced by prostatic epithelial cells. Levels can be elevated in prostate cancer and in some common noncancerous disorders (eg, benign prostatic hyperplasia, infection, trauma). PSA is measured to detect recurrence of cancer after treatment; its widespread use for cancer screening is controversial.
- 114. DIGITAL RECTAL EXAMINATION A digital rectal exam (DRE) is a test that examines a person's lower rectum, pelvis, and lower belly. This test can help your doctor check for cancer and other health problems, including: •Prostate cancer in men •An abnormal mass in the anus or rectum •Uterine cancer or ovarian cancer in women, along with a vaginal examination Rectal bleeding or blood in the stool A change in bowel habits, Discharge or bleeding from the urethra, the tube that carries urine out of the body A change in how urine flows
- 115. DIGITAL RECTAL EXAMINATION The patient lies on the left side with the buttocks near the edge of the examining table or bedside with the right knee and hip in slight flexion. The proctologic (knee–chest or prone jackknife) position is the preferred position in which to examine the perineum and rectum properly.
- 116. URINALYSIS A urinalysis is a test of urine. It is often done to check for a urinary tract infections, kidney problems, or diabetes. if you are admitted to the hospital, before you have surgery, or if you are pregnant. It can also monitor some medical conditions and treatments.
- 117. RENAL ANGIOGRAPHY A renal artery angioplasty and stent is done to treat a narrowed renal artery. Using X-rays as a guide, a small plastic tube is put into the narrowed artery. A special balloon on the tube is blown up to open the narrowed part of the artery. An expandable tube called a stent is then put in to keep the artery open. The whole process normally takes between 30 and 90 minutes.
- 118. RENAL SCAN A cannula is placed in a vein in arm and will be administered with a small injection of a radioactive tracer is administered through the cannula. This injection allows the Kidneys and Bladder to be seen by the camera. Images are taken for a 30 minutes whilst lying under the camera. Diethylenetriamine penta acetate is a medicine that can bind to radioactive plutonium, americium, and curium to decrease the amount of time. it takes to get radioactive plutonium, americium, and curium out of the body.
- 119. RENAL CT SCAN
- 120. RENAL MRI
- 121. CYSTOSCOPY/ CYSTOMETROGRAM During a cystoscopy, a cystoscope is inserted through the urethra into the bladder.
- 122. CYSTOSCOPY/ CYSTOMETROGRAM During a ureteroscopy, a ureteroscope is inserted through the urethra and into the ureter
- 123. CYSTOSCOPY/ CYSTOMETROGRAM • Cystoscopy and ureteroscopy are common procedures performed by a urologist to look inside the urinary tract. • Cystoscopy is a procedure that uses a cystoscope to look inside the urethra and bladder. A cystoscope is a long, thin optical instrument with an eyepiece at one end, a rigid or flexible tube in the middle, and a tiny lens and light at the other end of the tube. A urologist fills the bladder with fluid and looks at detailed images of the urethra and bladder linings on a computer monitor. • Ureteroscopy is a procedure that uses a ureteroscope to look inside the ureters and kidneys. Like a cystoscope, a ureteroscope has an eyepiece at one end, a rigid or flexible tube in the middle, and a tiny lens and light at the other end of the tube. However, a ureteroscope is longer and thinner than a cystoscope so the urologist can see detailed images of the lining of the ureters and kidneys.
- 125. CYSTOSCOPY/ CYSTOMETROGRAM • During a cystoscopy, a urologist can see • stones—solid pieces of material in the bladder formed by high concentrations of minerals in the urine • abnormal tissue, tumors, or cancer in the urethra or bladder • stricture, a narrowing of the urethra—a possible sign of an enlarged prostate in men or of scar tissue in the urethra • secondary signs of obstruction (or blockage), such as an enlarged prostate gland • other congenital or acquired abnormalities such as duplicated ureters, ureterocele, or diverticulum • During a cystoscopy, a urologist can sometimes treat problems, such as bleeding in the bladder and blockage in the urethra. A urologist may also use a cystoscopy to • remove a stone in the bladder or urethra • remove or treat abnormal tissue and tumors • take a sample of the urethra or bladder tissue for a biopsy • inject material into the wall of the urethra to treat urinary leakage or prevent vesicoureteral reflux • inject medicines into the bladder to treat urinary leakage • obtain urine samples from the ureters • perform retrograde pyelography—an x-ray procedure in which a urologist injects a special dye into the urinary tract to create images of urinary flow, to show obstructions such as kidney stones and tumors • remove a stent that was placed in the ureter after a ureteroscopy with biopsy or stone removal
- 126. CONTRAST STUDIES IVP
- 127. CONTRAST STUDIES IVP • IVP uses contrast dye to make these organs show up well on x-ray images. In males, x-rays from an IVP can also show the prostate. The prostate is a gland in the male reproductive system. It lies just below the bladder and makes the fluid part of semen. • During an IVP, contrast dye is injected into a vein using an intravenous (IV) line. The dye travels through your bloodstream to your kidneys, which filter it out. The dye collects in the organs of your urinary tract and makes them look bright white on the x-rays. This allows your health care provider to see blockages or other problems that affect your urinary organs. • IVP isn't commonly used anymore. Instead, providers usually order CT (computerized tomography) scans to see the urinary tract. CT scans can provide more information than x-rays from an IVP. But IVP may be useful in certain situations.
- 128. INDICATION • Pain in your side or back • Sharp pains in your abdomen (belly), side, groin or back • Blood in your urine • Cloudy or bad-smelling urine • Pain when urinating (peeing) • Needing to urinate frequently, or not being able to urinate • Nausea and vomiting • Swelling in your feet or legs • Fever and chills
- 129. STEPS • An IVP may be done in your provider's office or a hospital. The test is often done by a radiology technician (a health care professional who is trained to do x-ray exams). The procedure takes about an hour and generally includes these steps: • You'll usually remove your clothing and put on a gown. • You'll lie down on your back on an x-ray table. The technician will take an x-ray to make sure the machine is set right for you. • The technician will insert an IV into a vein in your arm or hand and inject the contrast dye. • Several x-rays will be taken to see how your kidneys filter the dye. You may be asked to move into different positions. • The technician may wrap a special belt tightly around your belly. This helps keep the contrast dye in your kidneys. After the belt is removed, more x-rays will be taken to show the dye passing from your kidneys through your ureters and into your bladder. • Before the IVP is finished, you'll be asked to use the bathroom or a bedpan to urinate. Then the last x-rays will be taken to see if any urine remains in your bladder. This shows how well your bladder works to empty urine. • After the test, drinking plenty of fluids will help flush the contrast dye out of your body.
- 130. LITHOTRIPSY
- 131. LITHOTRIPSY • Lithotripsy is a non-invasive procedure that uses high-energy shock waves or lasers to break down and eliminate bothersome stones in the kidney, quickly and effectively. During the procedure, a special machine called a lithotripter generates the shock waves that travel into your body and break apart the stones. • Pre Procedure • You must stop taking blood thinners 4 days prior to the procedure, as these can interfere with your blood’s ability to clot properly. • There are no food or dietary restrictions before the procedure.
- 132. LITHOTRIPSY • During Procedure • The procedure is completed in one sitting in a day, depending on the size and type of stones. The procedure usually takes about 30 to 90 minutes to perform. • You are settled comfortably in an area where your privacy is respected throughout the procedure. • Before the procedure, you will be asked to remove any jewellery or other objects that may interfere with the procedure. • You will be asked to change into a hospital gown and lie on a bed and positioned on a soft, transparent cushion-like apparatus attached to the bed. • Your vital parameters will be checked before the procedure. • During the procedure, high-energy shock waves will be transmitted through your body through the cushion-like apparatus, until they reach the kidney stones. A computerized USG machine is used to accurately locate the stone within the kidney. The shock waves are accurately targeted at the stones. The waves will break the stones into very small pieces that can easily be passed through your urinary system. • A constant tik-tik sound comes from the lithotripter. It is heard during the entire process. If the sound irritates you, you can ask for soft, rubber disposable earplugs available with the technician.
- 133. LITHOTRIPSY • Post Procedure • After the procedure, you will be required to spend about one hour in recovery/observation before being sent home. • During this time, some patients may experience bruising, soreness, giddiness and vomiting which will subside in some time. • You must drink plenty of water for several days after lithotripsy. This will help the kidneys flush out any remaining stone fragments. • Some patients may experience slight pain or a burning sensation during urination, for which antibiotics are prescribed. • A diet chart is given to you that needs to be adhered to, post the procedure.
- 135. RENAL/PROSTATE BIOPSY • Kidney biopsy is also called renal biopsy is a procedure during which a small piece of kidney tissue is removed and examined under microscope with a variety of stains to identify the underlying disease which is affecting the kidney function. The procedure of kidney biopsy is generally safe and can provide valuable information regarding the underlying kidney disease and helps in treatment. • Kidney biopsy is recommended in people with kidney disease. Based on the results of urine and blood tests nephrologist will advice the kidney biopsy. The most common reasons for kidney biopsy are as follows. More than one reason may be present in a given patient.Blood in the urine (called haematuria) • Protein in the urine (called proteinuria) • Problems with kidney function (if the kidneys function declines slowly or suddenly and the cause is not clear)
- 136. RENAL/PROSTATE BIOPSY • Procedure for kidney biopsy • During the procedure patient will lie on his abdomen with back facing the roof and will be awake. For patients who are renal transplant recipient’s biopsy is done with patient lying on back. Kidney biopsy procedure included following stepsUsing an ultrasound machine probe, size of the kidneys and position of the kidneys are assessed first and then a site is identified to insert the kidney biopsy needle • Skin over the back where the site of entry is marked is cleaned with antiseptic • A local anaesthetic medication is injected with a syringe with needle at the site of entry to numb the area • Using the ultrasound probe as a guide, a biopsy needle (a spring-loaded instrument) is inserted and sample of kidney is collected • Patient is asked to hold the breath while collecting the sample and patient hears a pop sound or sharp clicking sound or feel some pressure • Biopsy needle maybe inserted few times to get adequate sample • Once the procedure is completed a bandage is placed over the biopsy site
- 137. RENAL/PROSTATE BIOPSY • Post procedure care • Patient is admitted in hospital over night after the biopsy to monitor for complications. Immediately after the procedure biopsy site is compressed and patient lies on his back. His pulse rate and blood pressure are monitored every 30 minutes for 6 hours. Patient is given transparent containers to collect urine each time he passes so that if any bleeding happens will be identified. After 6 hours patient can move in bed to sides but strict bed rest is advised overnight. Next day morning his blood pressure and pulse rate is checked and if there is no complication (like blood in urine) patient is discharged.
- 138. PROSTATE BIOPSY The prostate is a small, walnut-shaped gland in men that produces fluid that nourishes and transports sperm. A prostate biopsy is a procedure to remove samples of suspicious tissue from the prostate. It is performed by an urologist, who is a doctor specialized in the urinary system and men’s sex organs.
- 139. PROSTATE BIOPSY • A prostate biopsy is usually performed on Day ward. Procedures may vary depending on your condition and your doctor practices. • During a prostate biopsy, a fine needle is used to collect a number of tissue samples from your prostate gland. Generally, doctors collect prostate biopsy samples through the wall of the rectum. This is called a trans-rectal prostate biopsy. Less often, the prostate is accessed through the tip of the penis (urethra), or through the space between the anus and scrotum (perineum). • For a trans-rectal prostate biopsy, your doctor will start by having you lie on your side, with your knees pulled up to your chest. • After cleaning the biopsy area and applying numbing gel, your doctor will gently insert a thin ultrasound probe into your rectum. Trans-rectal ultrasonography is used to create images of your prostate using sound waves. Your doctor will use the image to identify the area that needs to be numbed with an anesthetic injection, if one is used. It’s also used to guide the prostate biopsy device into place. • Once the biopsy device is into the right place in the prostate, your doctor will retrieve thin, cylindrical sections of tissue with a hollow, spring-propelled needle. The procedure typically causes a very brief, uncomfortable sensation each time the fine needle takes a sample. Your doctor may target a suspicious area to biopsy, or may take samples from several places in your prostate. In most cases, doctor will take 10 to 12 tissue samples or more if necessary. The entire procedure usually takes about 20 to 30 minutes. • Tissue samples from the prostate biopsy are sent to a specialized pathology laboratory and examined under a microscope for cell abnormalities that are a sign of prostate cancer. If cancer is present, it is evaluated to determine how quickly it is likely to grow and spread and to determine your best treatment options.
- 140. PROSTATE BIOPSY • After a prostate biopsy, you’ll probably need to continue taking an antibiotic for a few days. You may feel slight soreness and have some light bleeding from your rectum. You may have blood in your urine or stools for a few days. You may also notice that your semen has a pinkish tint caused by a small amount of blood in your semen. This can last for more than a month. • Call your doctor or come to the hospital if you have: • Prolonged or heavy bleeding • Pain that gets worse • Swelling near the biopsy area • Difficulty urinating
- 141. URODYNAMIC TESTING An urodynamic study is an examination and assessment of a patient's bladder muscles and the sphincter to determine whether or not they are functioning and contracting correctly. An urodynamic study will measure the pressure in the bladder while water flows through and out of the bladder.
- 143. GONORRHEA TEST Caused by bacteria Neisseria gonorrhoeae gonorrhea is common and can be cured. It is the second most commonly communicable disease An estimated 820,000 new infections each year in US.
- 144. CATHETERIZATION CARE • A Foley catheter is a rubber tube inserted into your bladder. Once the catheter is in your bladder, a small balloon is inflated at the tip of the tube to hold the catheter in place. The purpose of the catheter is to drain urine from your bladder. • The size of a urinary catheter is based on the French (Fr) scale, which reflects the internal diameter of the tube. Recommended catheter size is 12 to 16 Fr for females, and 14 to 16 Fr for males. Smaller sizes are used for infants and children. The balloon size also varies with catheters: smaller for children (3 ml) and larger for continuous bladder irrigation (30 ml). The size of the catheter is usually printed on the side of the catheter port.
- 145. CATHETERIZATION CARE • Female patient: On back with knees flexed and thighs relaxed so that hips rotate to expose perineal area. Alternatively, if patient cannot abduct leg at the hip, patient can be side-lying with upper leg flexed at knee and hip, supported by pillows. • Male patient: Supine with legs extended and slightly apart.
- 146. CATHETERIZATION CARE • In most cases, a urinary catheter is used in people who are unable to pass urine naturally because of an illness or injury. Common medical conditions requiring for urinary catheterisation include: • Urinary incontinence: difficulty controlling when to urinate or leakage of urine, caused by bladder weakness or a medical condition, including multiple sclerosis or an injury in the spinal cord. To learn more about urinary incontinence, causes and treatment, check out our dedicated article here. • Urinary retention: difficulty emptying the bladder when urinating. This can happen as a result of another medical condition such as benign prostatic hyperplasia (BPH), prostatitis (inflammation of the prostate gland), a kidney stone obstructing the urinary tract, damage to the nerve after a stroke, or a complication from diabetes called diabetic peripheral neuropathy. Some medications can also cause the side effects of urinary retention. • Before or after a surgery, most often surgery of the prostate or genitals. • In some instances, urinary catheters are used when conducting diagnostic tests.
- 147. CATHETERIZATION CARE • There are three primary types of urinary catheters: indwelling, external, and intermittent catheters. A doctor or nurse would assess and recommend the type of urinary catheter, as well as the size, based on the patient’s medical condition, weight, age, and gender. • Indwelling catheter, commonly referred to as Foley catheter – this type of catheter remains in place for an extended period that could range from days to up to 12 weeks. It is held in place with a water-filled balloon inside the patient’s bladder. Foley catheter is typically inserted through the urethra. In some cases, it is inserted through a hole in the abdomen, and referred to as a suprapubic catheter. • Intermittent catheter, also called short term catheter, or in and out catheter – it is used temporarily to empty the bladder once, then removed. Intermittent catheterisation needs to be done several times a day, at a designated interval or when there is a need to pass urine. Traditional intermittent catheters can be washed and reused. Disposable intermittent catheters are designed for one time use and discarded. • External catheter – this type of catheter is often used for male patients with urinary incontinence rather than urinary retention.
- 148. CATHETERIZATION CARE
- 149. CATHETERIZATION CARE • Urinary catheterisation process differs for different types of catheters. Indwelling or Foley catheters are usually inserted by healthcare professionals, such as nurses in clinics and hospitals. Daily care can be done at home by caregivers. Patients who use urinary catheters permanently will also need professional help to remove and replace catheters at least once every 2 months. • Intermittent urinary catheterisation however can be done at home by a caregiver or self-administered by the patient. As complex as it sounds, most patients and caregivers report being able to carry out intermittent catheterisation with ease and without discomfort after a few times. • Below is a general description of the catheterisation process. • For an indwelling or Foley catheter, the healthcare professional typically will: • Perform hand hygiene • If possible, place the patient on their back with knees bent and hips flexed. • Use sterile gloves and other sterile materials to expose the urethra and insert the lubricated catheter into the urethral opening until urine begins to flow. • Inject sterile water to inflate the catheter inside the bladder. • Attach the other end of the catheter tube to a drainage bag.
- 150. CATHETERIZATION CARE • For intermittent catheterisation, a nurse often instructs the caregiver or the patient to carry out the process. If the patients are able to administer the catheter themselves, the procedure is known as self-catheterisation or clean intermittent catheterisation. 1. Hand hygiene: Wash hands thoroughly before the procedure and do not touch anything but the catheter. You can use clean gloves. 2. Positioning: Have the patient lie on their back with knees bent and hips flexed, or get in a comfortable sitting or standing position and use a mirror to guide yourself for self-catheterisation. Special mirrors that can be attached to the leg are available for this purpose, allowing patients to conduct self-catheterisation without having to hold on to the mirror. 3. Insertion: Apply firm but gentle pressure to insert the lubricated end of the catheter into the urethra. Then carefully guide the catheter up into the urethra until it gets to the bladder and urine begins to flow out. 4. Urine collection and removal: Insert another two inches and allow the urine to flow out into a collection container then carefully and slowly remove the catheter. •
- 151. CATHETERIZATION CARE
- 152. BLADDER IRRIGATION • Bladder irrigation is a procedure used to flush sterile fluid through your catheter and into your bladder. Bladder irrigation helps remove and prevent blood clots in your bladder. • The blood clots stop urine from flowing through your catheter. The urine collects in your bladder and causes pain that gets worse as your bladder fills. • Bladder irrigation may be needed after bladder or prostate surgery. • Chemotherapy and radiation can also cause blood clots in your bladder.
- 155. ARTICLES • Disposable gloves • b)Mackintosh • c)Three way retention catheter • d)Sterile drainage tubing and bag in place • e)Sterile antiseptic swab • f)Sterile receptacle • g)Sterile irrigation solution warmed or at room temperature. • h)Normal saline • i)Distilled water • j)Solution as prescribed by physician • k)Infusion tubing l)IV Stand m)Kidney tray n) paper bag •
- 156. PROCEDURE • 1. Check the physicians order for amount and strength of irrigating fluid andreason for irrigation. • • 2. Preparatory phase :a) Explain the procedure and purpose to the client to reduce anxiety. b) Provide privacy and drape the client. c) Empty, measure and record the amount and appearance of urine present inthe urinary bag. • 3. Prepare the equipments: a) Wash hands to reduce transmission of microorganism. b) Connect the irrigation infusion tubing to the irrigating solution and flushthe tubing with solution to remove air. c) Connect the irrigation tubing to the input port of the 3-way catheter.Connect the drainage bag and tubing to the urinary drainage port if notalready in place. • 4 Irrigate bladder • Intermittent irrigation . Instill the prescribed amount of irrigant. If specific amount is not ordered,fill up to 150ml of irrigant. Clamp the irrigant tubing to prevent further filling of irrigant. •
- 157. PROCEDURE • If physician has ordered the irritant to remain in the bladder for a measured length of time, clamp the drainage tube and wait for the prescribed length of time. Open the drainage tube (the clamp) and monitor the drainage bag. • Continuous bladder irrigation. Adjust the clamp on the irrigation tube to allow the prescribed rate of irrigation to flow into the catheter and bladder. Monitor the color, clarity, debris and volume as it flows back into the drainage bag. • Tape the catheter securely on the thigh to prevent catheter from dislodging. • • Assess the patient’s condition and tolerance of procedure. • Discard all used disposable articles, clean and replace reusable articles. • • Wash hands to prevent cross infection. Record the procedure. •
- 159. AMBULATION • Ensure patient does not feel dizzy or lightheaded and is tolerating the the upright position. • Instruct the patient to sit on side of the bedfirst,prior to ambulation. • Ensure proper footwear is on patient and let patient know how far you will be ambulating, proper footwear is non slip or slip resistantfootwear. • Check physician`s orders for any activityrestrictions related to treatment or surgical procedures. • Apply gait belt snugly around the patient`s waistif required. • Assist patient by standing in front of the patient ,grasping each side of gait belt, keep back straightand knees bent. • While holding the belt, gently rock back and forththree time ,one third time ,pull patient into a stand position.
- 160. AMBULATION • Once patient is standing and feels stable move to the unaffected side and grasp the gait belt in the middle of the back with the other handhold the patient hand closest to you. • If the patient does not require a gait belt place hand closest to the patient around the upper arm and hold the patient`s hand with your other hand. • Before stepping away from the bed, ask the patient if they feel dizzy or lightheaded if they do sit patient back down on the bed. • If the patient feel stable begin walking matching your step to the patient, instruct patient is look ahead and lift each foot off the ground. • To help a patient back to bed have patient a stand with back of knees touching the bed grasp the gait belt and help patient into a sitting position keeping your back straight and knees bent. • When the patient is finished ambulating, remove gait belt and settle patient into bed or chair. • Wash hands.
- 161. EXERCISES
- 165. GLOMERULONEPHRITIS(GN) DEFINITION:- Glomerulonephritis is a kidney condition that involves damage/ inflammation to the glomeruli. CAUSES:-Streptococcal infection of the throat and the skin(impetigo) Immune diseases, diabetes, high blood pressure endocarditis viral infection like HIV. SYMPTOMS:-Flank pain , foamy urine , cola colour or diluted ice tea color urine, haematuria, fluid retention, oliguria, dysuria, HTN. DIAGNOSTIC EVALUATION: History collection, physical examination ,urinalysis, biopsy intravenous pyelogram , blood test , USG TREATMENT: Diuretics(frusemide), immunosuppressant , antihypertensive drugs, Dialysis
- 166. URINARY INCONTINENCE DEFINITION • Incontinence is involuntary loss of urine from the bladder. CAUSES :- • D-delirium, I-infection, A-atrophic vaginitis, P-pharmaceuticals, P- psychological disorder, E- endocrine disorder, R-restricted mobility SYMPTOMS:- • Stress incontinence occurs when :chough, sneeze, laughing, standing in prolonged time • Urge incontinence occurs: frequent urination, in a day and at night, Sudden urination and urinary urgency • Overflow incontinence occurs: bladder never feels empty, urine dribbles even after voiding TREATMENT: Anticholinergic( medication to calm an overactive bladder ) Antidepressant, pelvic floor exercise , bladder training. kegel exercise
- 167. URINARY RETENTION DEFINITION • Inability to void even when the urge to void is present. CAUSES:- • Tumor, interference with the sphincter muscles during surgery, side effect of medications SYMPTOMS:- • Frequency of urination, voiding small amounts, pain, palpation of a distended bladder above the symphysis pubis TREATMENT:- Analgesic, colinergic medication, urinary catheter, surgery may be performed to remove any obstruction .
- 168. URINARY TRACT INFECTIONS (UTI) DEFINITION • UTI is a bacterial infection in part of a urinary tract. When it affects the lower urinary track it is known as simple cystits (bladder infection).when it affects the upper urinary tract it is known as pyelonephritis(kidney infection). CAUSES: • Urine is excellent medium for microorganism growth • Escherichia coli. • Females more anatomically vulnerable • Older males with prostatic hypertrophy and retention of urine prone to UTI
- 169. UTI CYSTITIS—signs and symptoms • Pain in lower abdomen, dysuria, frequency, urgency, inflammation of bladder wall irritated by urine, systemic signs of infection PYELONEPHRITIS—signs and symptoms • Signs of cystitis, Dull aching pain in lower back that results from renal capsule stretching, cloudy urine with unusual odor DIAGNOSTIC EVALUATION:- • History collection, physical examination, • Urinalysis indicates bacteria (+100,000/ml), pyuria, microscopic hematuria TREATMENT • Antibiotics (Bactrim),Increase fluid intake, Especially cranberry juice.
- 170. URINARY TRACT OBSTRUCTIONS: UROLITHIASIS DEFINITION: • Urolithiasis refers to stones (calculi) in the urinary tract stones are formed in the urinary tract when urinary concentrations of substance such as calcium oxalate, calcium phosphate, and uric acid increase. CAUSES:- • Chronic dehydration, poor fluid intake, infection, urinary stasis, inflammatory bowel disease, medication- antacids, acetazolamide vitamin-d.
- 171. URINARY TRACT OBSTRUCTIONS: UROLITHIASIS SIGN AND SYMPTOMS:- • Pain : “renal colic” it consists of intense spasms in back and groin, hematuria, edema, dysuria, nausea, vomiting, diarrhea, abdominal discomfort, chills and fever. DIAGNOSTIC EVALUATION: • History taking, physical examination, urinalysis, blood studies, stone chemistry radiographic studies TREATMENT • Small stones eventually passed out • Larger stones: Extracorporeal shock-wave lithotripsy (ESWL) • Some drugs can partially dissolve
- 172. NEPHROTIC SYNDROME DEFINITION • Nephrotic syndrome is a clinical disorder characterized by marked increase of protein in the urine (proteinuria),decrease in albumin in blood (hypo-albuminemia), edema, and excess lipids in the blood (hyperlipidemia). ETIOLOGY • Physiologic changes of the glomeruli interfere with selective permeability, CLINICAL MANIFESTATIONS • Proteinuria; hypo-albuminemia, Generalized edema, Anorexia, Fatigue, Oliguria
- 173. NEPHROTIC SYNDROME DIAGNOSTIC EVALUATION • History taking, physical examination, urinalysis, blood studies. TREATMENT • Treatment of causative glomerular disease, diuretics and angiotensin converting enzymes inhibitors to control proteinuria, corticosteroids and immunosuppressant's. • General management of edema: sodium and fluid restriction.
- 174. ACUTE RENAL FAILURE DEFINITION • Acute renal failure is a sudden and almost complete loss of kidney function caused by failure of renal circulation or by glomerular or tubular dysfunction. ETIOLOGY • Pre renal: hemorrhage, renal loses, anaphylaxis. • Intra renal: prolonged renal ischemia, nephrotoxic agent, heavy metals. • Post renal: renal calculi, tumors, blood clots
- 175. ACUTE RENAL FAILURE SYMPTOMS • Nausea, weight loss, pale urine, hematuria, nocturnal urination, pain back and side, Poor skin turgor, Urine output less than 400 mL/24 hours TREATMENT • Pharmacological management: Diuretics, Antibiotics • Administer fluids, Dialysis • Diet: High in carbohydrates; low in protein, potassium, and sodium
- 176. CHRONIC RENAL FAILURE DEFINITION • Chronic renal failure also known as chronic kidney disease, this is present when GFR has fallen to around 20% of normal. ETIOLOGY • Hemorrhage, renal loses, anaphylaxis, prolonged renal ischemia, nephrotoxic agent, heavy metals.
- 177. CHRONIC RENAL FAILURE SYMPTOMS • Headache, Lethargy, Anorexia, Pruritus, Anuria, Muscle cramps or twitching, Dusky yellow-tan or gray skin color, Disorientation and mental lapses, Anemia TREATMENT: • Dialysis, Renal transplant, Medications to treat symptoms • Diet: High in calories; restricted protein, potassium, and sodium, Restricted fluids
- 179. ASSIGNMENT • Draw a diagram of kidney • Draw a diagram of bladder • Write the process of Urine formation • Write a note on micturition
- 180. SUMMARY • The organs of the urinary system include the kidneys, ureters, bladder, and urethra. • The kidneys remove metabolic waste products from the blood and secret erythropoietin and renin. • Urine travel through the ureters to bladder • Stretching of the bladder triggers micturition reflex. • Urine travels from the bladder through the urethra to outside world.
- 181. CONCLUSION • Urinary system is helps to extract excess mineral or vitamins. • Urinary system is maintain the acid base (pH) balance. • Remove waste products and drugs from the body. • Balance the body’s fluids. • Control production of red blood cells. • The urinary system filters waste and extra fluid from the blood stream.
- 182. RECAPTUALIZATION Question. Define kidney Answer. The kidneys are a pair of excretory organs situated on the posterior abdominal wall, one on the vertebral column, behind the peritoneum. Question. What is the functional unit of kidney? Answer. Nephron
- 183. RECAPTUALIZATION Question. Explain the composition of urine? Answer . Water (96 %),urea (2 %), uric acid, creatinine, ammonia, sodium, potassium, chlorides, phosphates, sulphates and oxalates (2 %).
- 184. RECAPTUALIZATION Question. What is nephrotic syndrome? Answer. Nephrotic syndrome is a clinical disorder characterized by marked increase of protein in the urine (proteinuria),decrease in albumin in blood (hypoalbuminemia), edema, and excess lipids in the blood (hyperlipidemia).
- 185. BIBLIOGRAPHY BOOK REFERENCE:- Wilson and Ross. Anatomy and Physiology in Health and Illness 12th edition (International Edition) Anne Waugh Allison Grant. ELSEVIER INTERNET REFERENCE: https://www.healthengine.com https://www.donatingplasma.org https://www.slideshare.net https://en.m.Wikipedia.org
- 186. •Thank you
