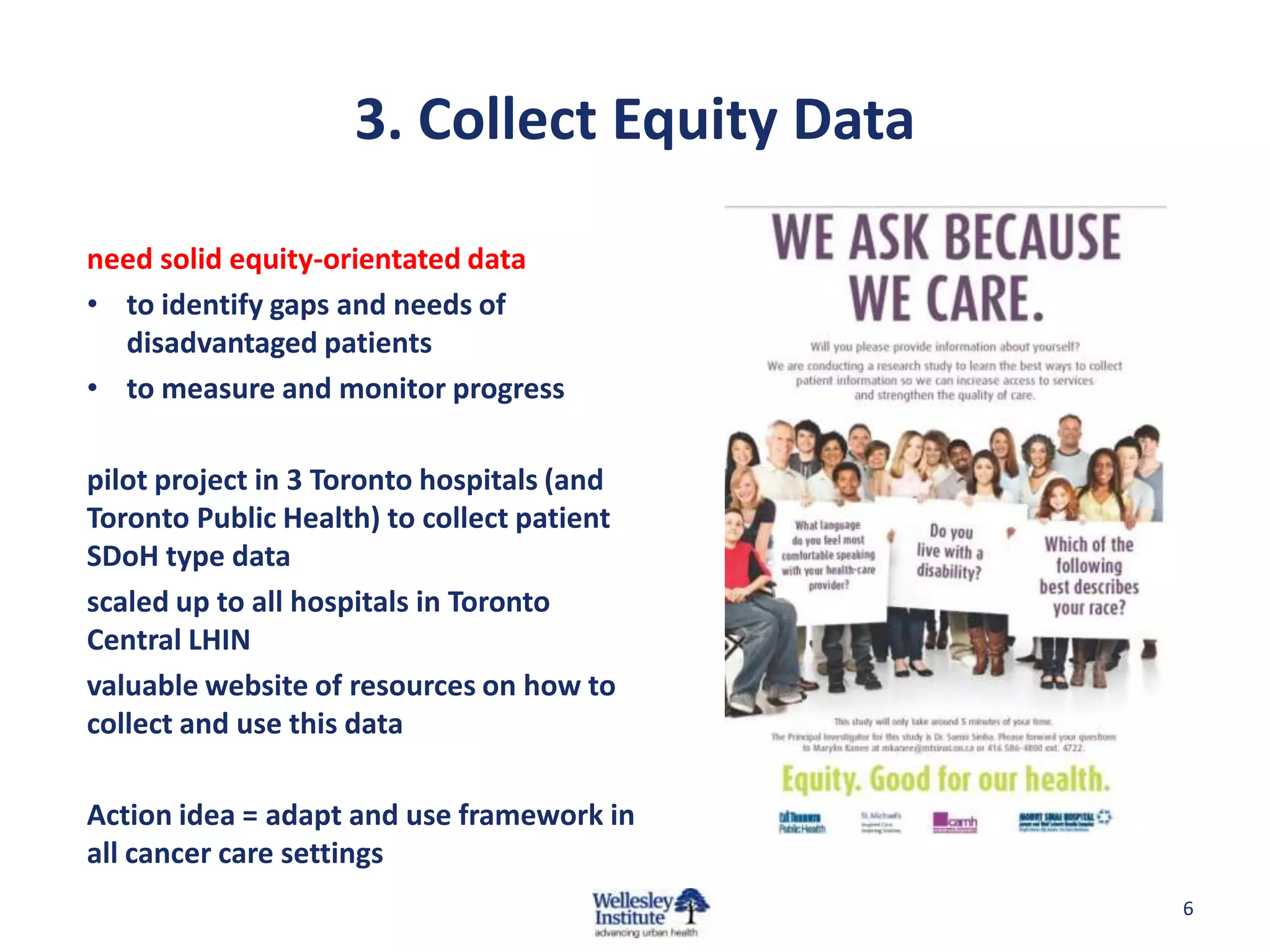
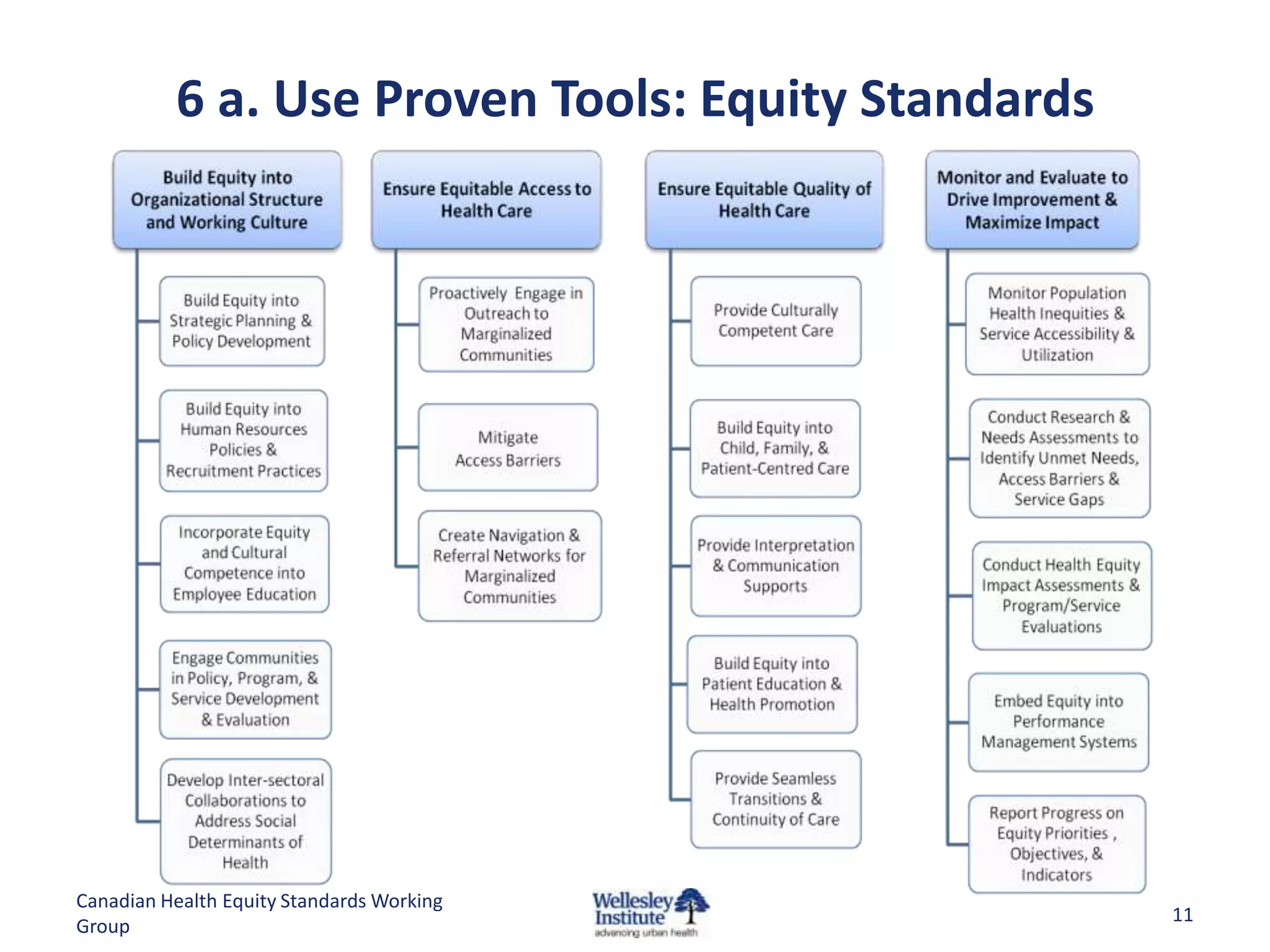
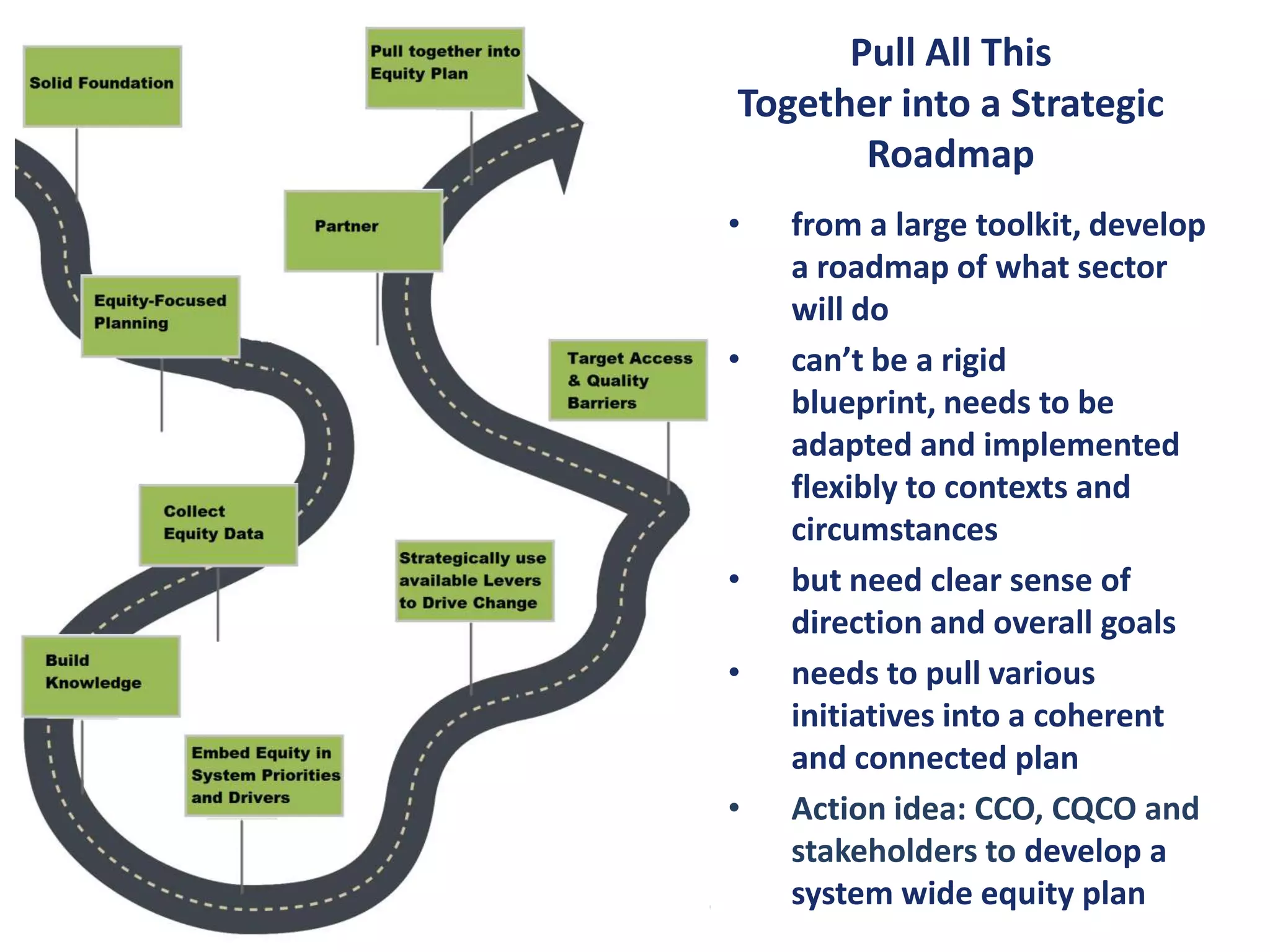
The document outlines an equity toolkit aimed at improving cancer care for disadvantaged populations by addressing social determinants of health and identifying barriers throughout the cancer care journey. It recommends solutions such as equity-focused planning, data collection, and community partnerships to enhance access and quality of care for underserved groups. The toolkit emphasizes the necessity of embedding equity into health care systems, programs, and performance management to ensure comprehensive and culturally competent cancer care.