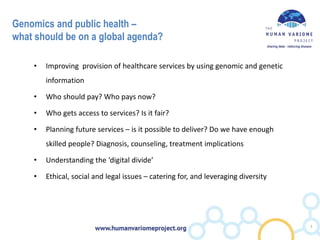
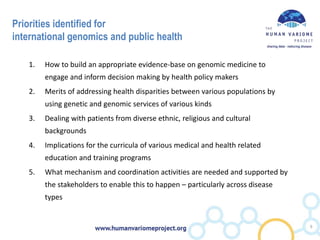
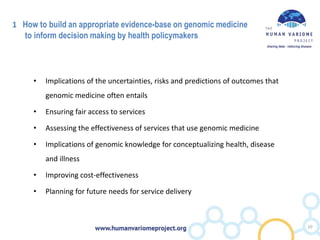
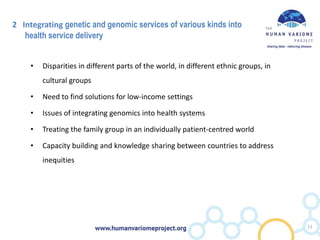
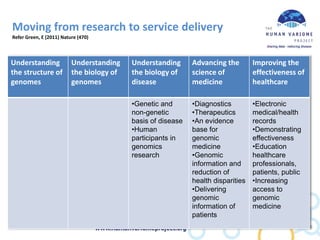
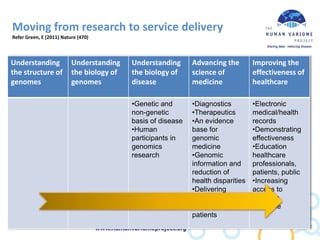
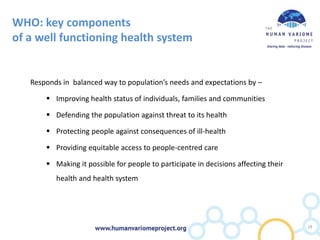
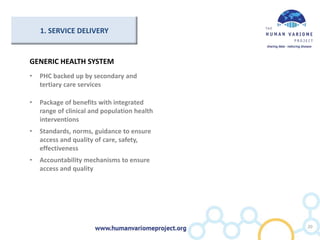
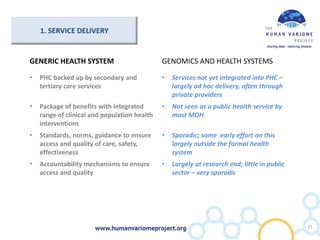
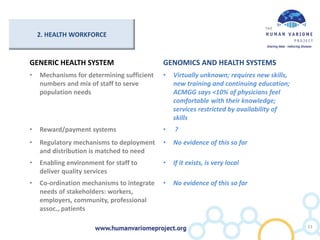
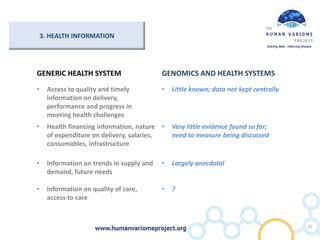
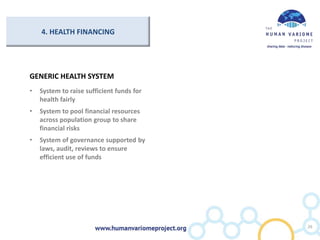
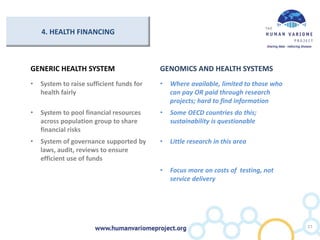
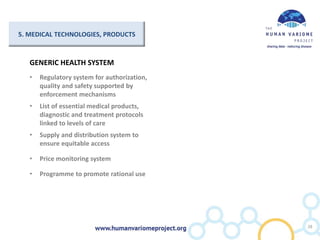
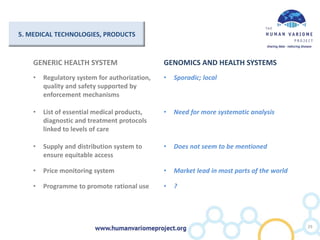
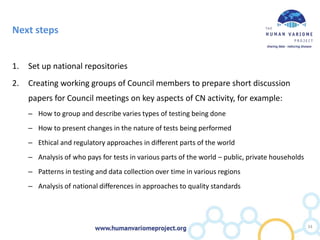
This document discusses challenges for low and middle income countries regarding human genomics and public health in a global context. It notes that while genomics activity is increasing in about 50 countries, it remains fragmented without systematic monitoring or links to health policymakers. Five priorities for international genomics are identified: building an evidence base for genomic medicine, addressing health disparities, managing diverse patient populations, implications for medical education, and coordination across diseases. The document argues for greater global collaboration to improve access, establish standards, and promote equity and justice.