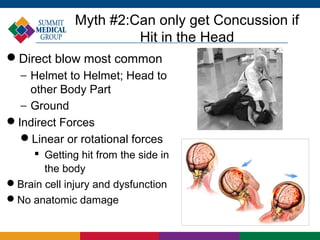
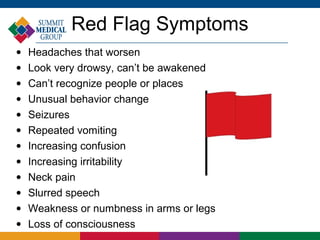
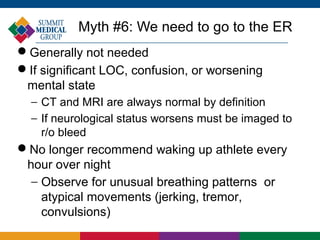
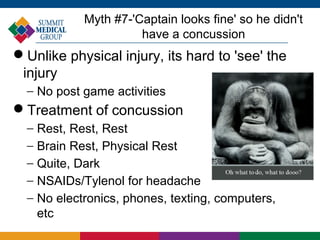
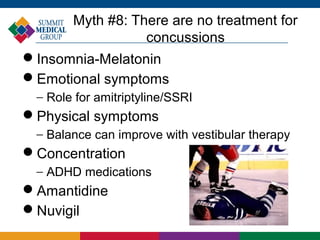
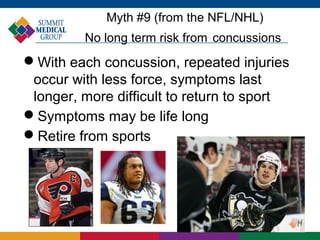
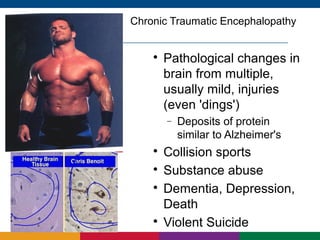
The document discusses sports concussions, emphasizing that they are a significant issue affecting athletes of all ages and not just football players. It debunks several myths surrounding concussions, such as the need for loss of consciousness for diagnosis and the nature of recovery, highlighting the importance of proper assessment and management. The article stresses that each concussion is unique and stresses the need for awareness in sports to prevent long-term consequences, such as chronic traumatic encephalopathy.