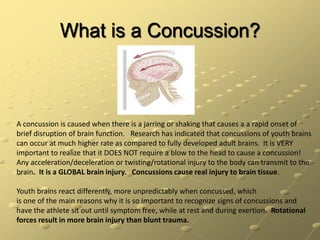
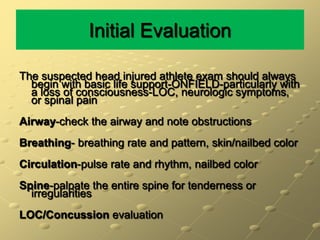
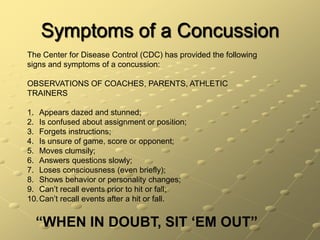
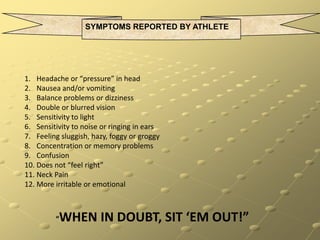
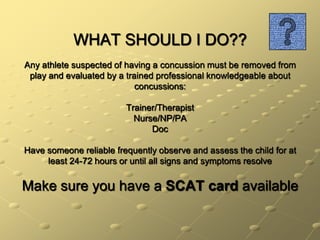
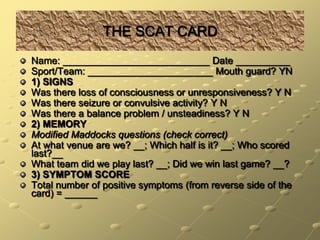
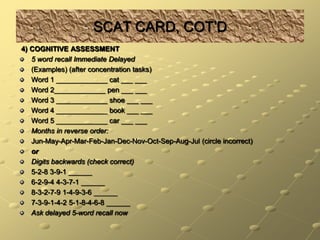
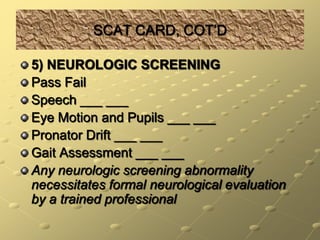
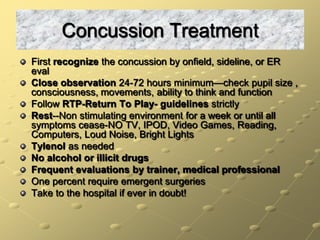
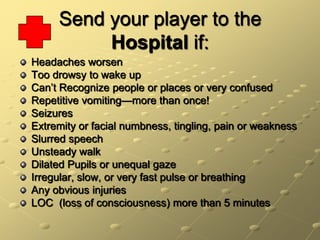
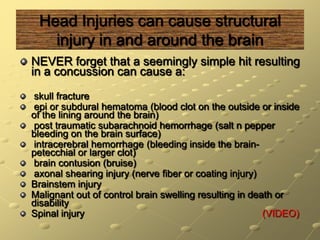
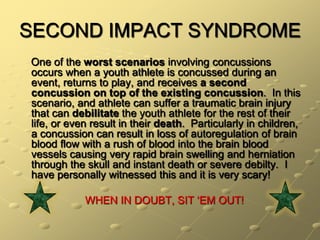
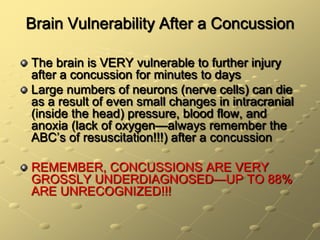
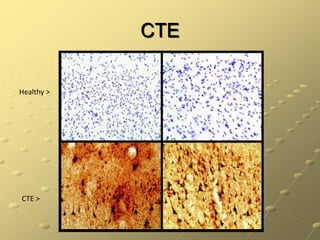
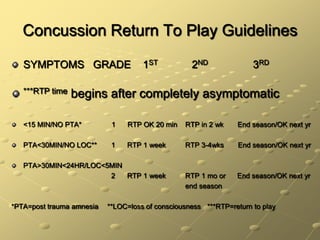
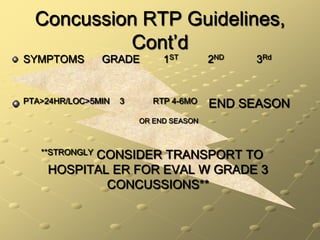
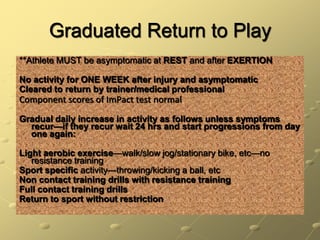
This document provides information about concussions in football, including definitions, symptoms, treatment guidelines, and long-term effects. It defines a concussion as a brief disruption of brain function caused by a blow or jarring motion to the head. Symptoms may include headaches, dizziness, memory problems, and more. The document outlines return to play guidelines and emphasizes the importance of not returning to play until fully recovered to avoid second impact syndrome, which can have severe consequences. It also discusses potential long-term effects of repeated concussions like chronic traumatic encephalopathy.