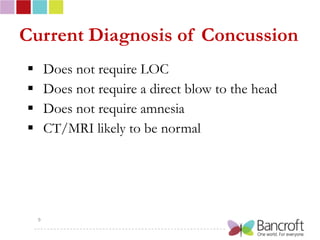
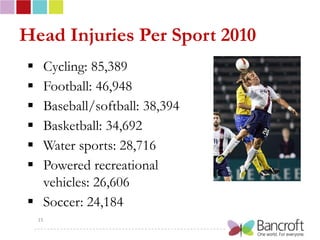
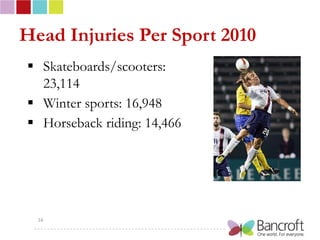
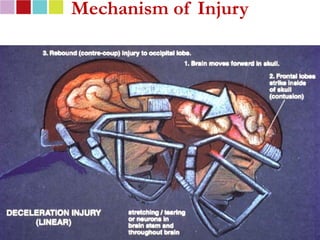
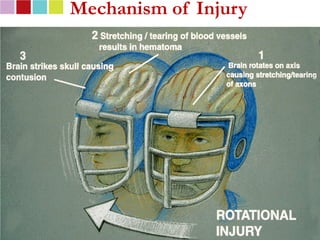
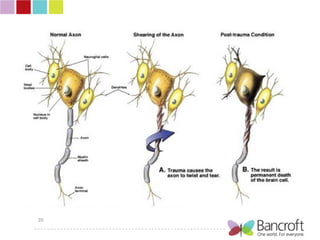
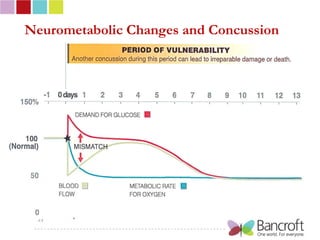
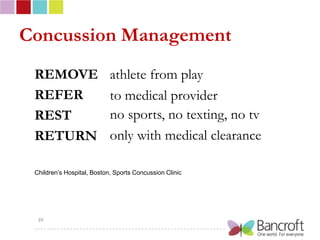
The document discusses the increasing prevalence and risks associated with sports-related concussions, highlighting that over 3.8 million concussions occur annually in the U.S. and particularly among high school athletes. It outlines the nature of concussions, their symptoms, potential long-term effects such as chronic traumatic encephalopathy, and emphasizes the importance of recovery protocols and prevention strategies. The document also provides resources for further education and management of concussions in sports.