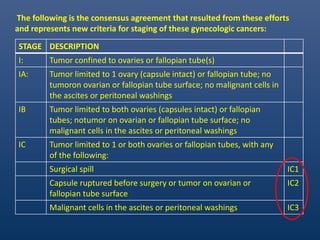
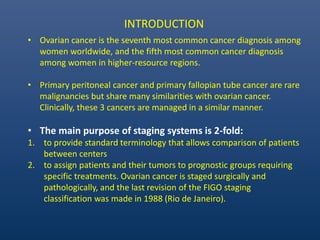
1. The document summarizes the revised FIGO staging system for ovarian, fallopian tube, and primary peritoneal cancers from 2012.
2. It outlines the stages from I to III, including substages, based on the extent of disease progression from the ovaries/fallopian tubes to the pelvis or further.
3. The revisions aimed to improve reproducibility and assign patients to prognostic groups for standardized treatment comparisons between centers.


![1. Ovarian cancer is not a homogeneous disease, but rather a group of
diseases—each with different morphology and biological behavior.
2. In the era of personalized cancer medicine, reproducible histopathologic
diagnosis of tumor cell type is a sine qua non for successful treatment. As
different tumor histotypes respond differently to chemotherapy.
Ovarian cancers differ primarily based on histologic type: 5 main types
a) high-grade serous carcinoma (HGSC [70%]);
b) endometrioid carcinoma (EC [10%]);
c) clear-cell carcinoma (CCC [10%]);
d) mucinous carcinoma(MC [3%]);
e) low-grade serous carcinoma (LGSC [b5%])](https://image.slidesharecdn.com/journalpresentation-150609183012-lva1-app6892/85/figo-ovary-staging-update-4-320.jpg)