Cardiopulmonary Bypass Machine: A Comprehensive Guide for Medical Students and Professionals
Overview:
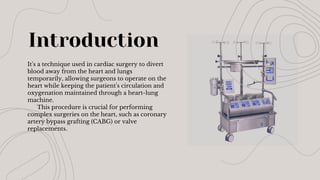
The Cardiopulmonary Bypass (CPB) Machine, commonly referred to as the Heart-Lung Machine, is a life-saving device used in cardiac surgeries. It temporarily replaces the functions of the heart and lungs, ensuring continuous circulation and oxygenation of the blood while the heart is stopped. This allows surgeons to perform delicate and complex procedures like open-heart surgery, valve replacement, and coronary artery bypass grafting (CABG) with precision and safety.
Key Topics Covered in This Presentation:
>History of CPB
>Components of CPB
>Working Mechanism
>Indications for CPB
>Monitoring During CPB
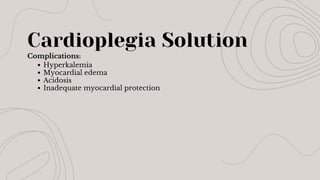
>Complications & Risks
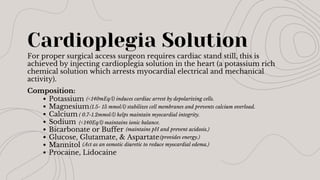
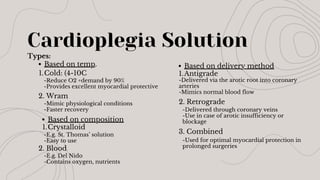
>Cardioplegia Solution
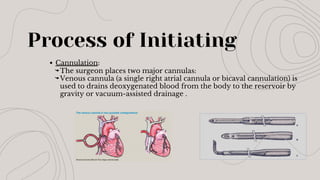
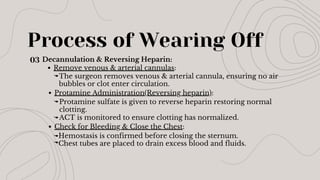
>Initiation & Weaning Process
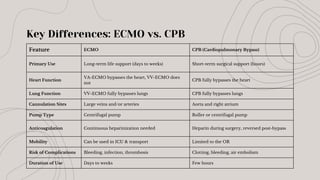
>Comparison Between CPB & ECMO
>Understanding the Cardiopulmonary Bypass Machine:
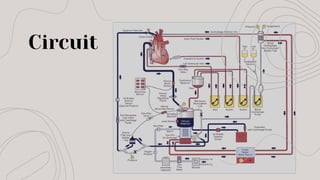
How CPB Works
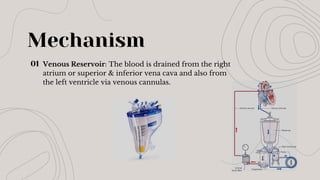
Venous Drainage
Oxygenation & CO₂ Removal
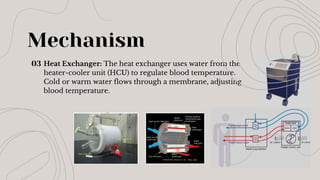
Temperature Control
Pump Circulation
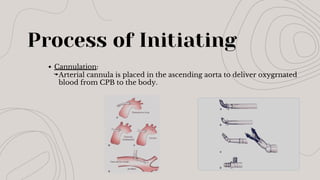
Arterial Return
Cardioplegia Administration
>Why CPB Is Important in Cardiac Surgery
>Potential Complications & Risks of CPB
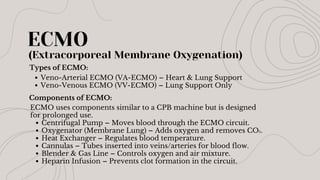
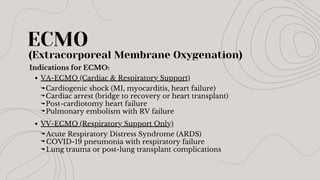
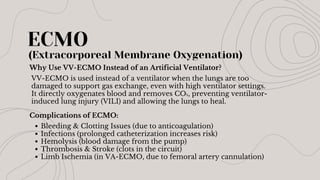
>Comparison: CPB vs. ECMO (Extracorporeal Membrane Oxygenation)
Final Thoughts
The Cardiopulmonary Bypass Machine is one of the most significant innovations in modern cardiovascular medicine.
By allowing open-heart surgeries to be performed safely, it has saved millions of lives and continues to evolve with advanced perfusion technologies.
This detailed presentation is designed for:
📌 Medical students learning about cardiac surgery techniques.
📌 Surgical technologists & perfusionists working with heart-lung machines.
📌 Cardiologists & anesthesiologists seeking a refresher on CPB principles.
📌 Researchers & healthcare professionals exploring advancements in extracorporeal circulation.
💾 Download now to gain valuable insights into one of the most essential technologies in cardiac surgery!
By H. Hoda (BSc. OT Technologist)