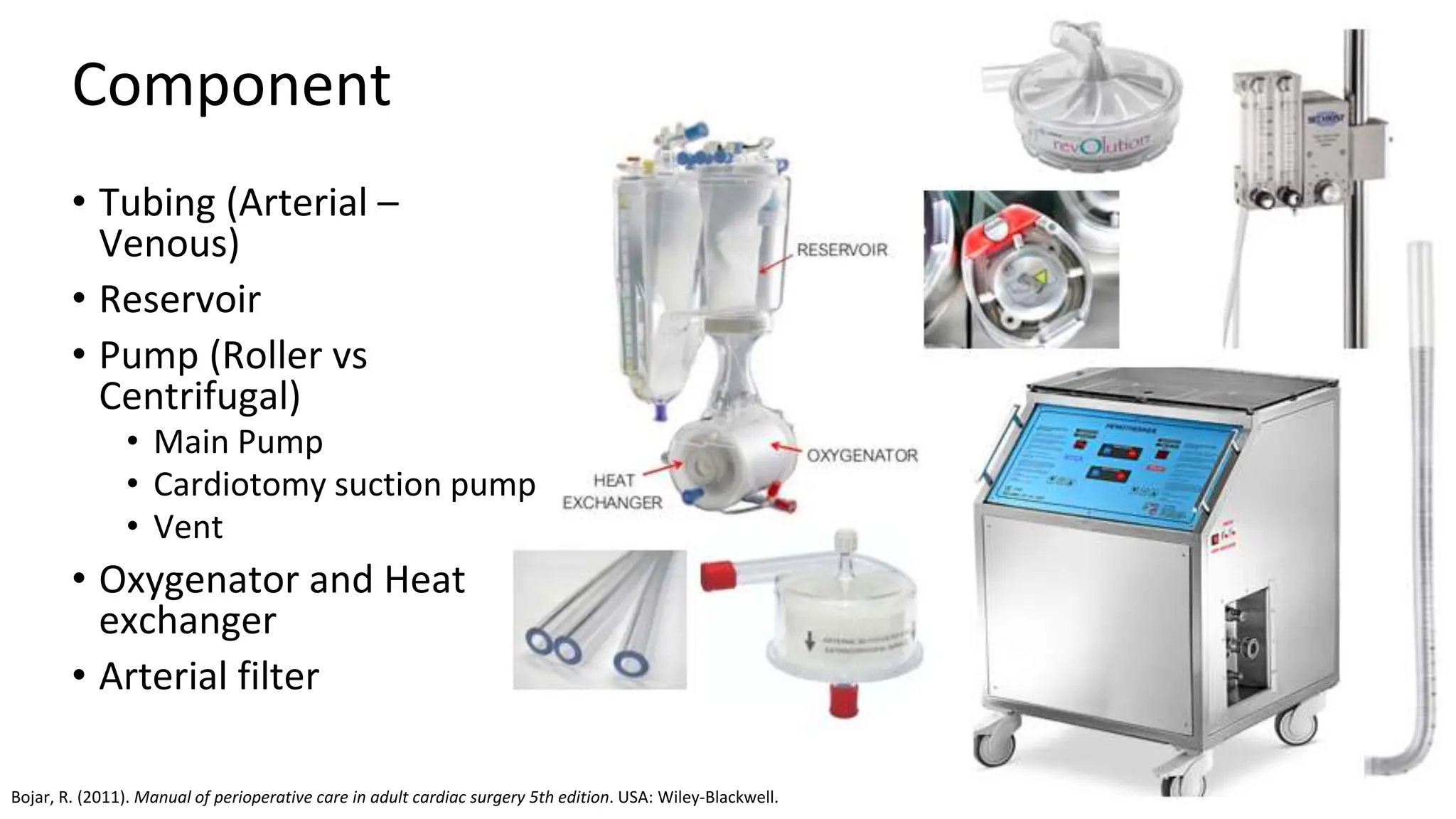
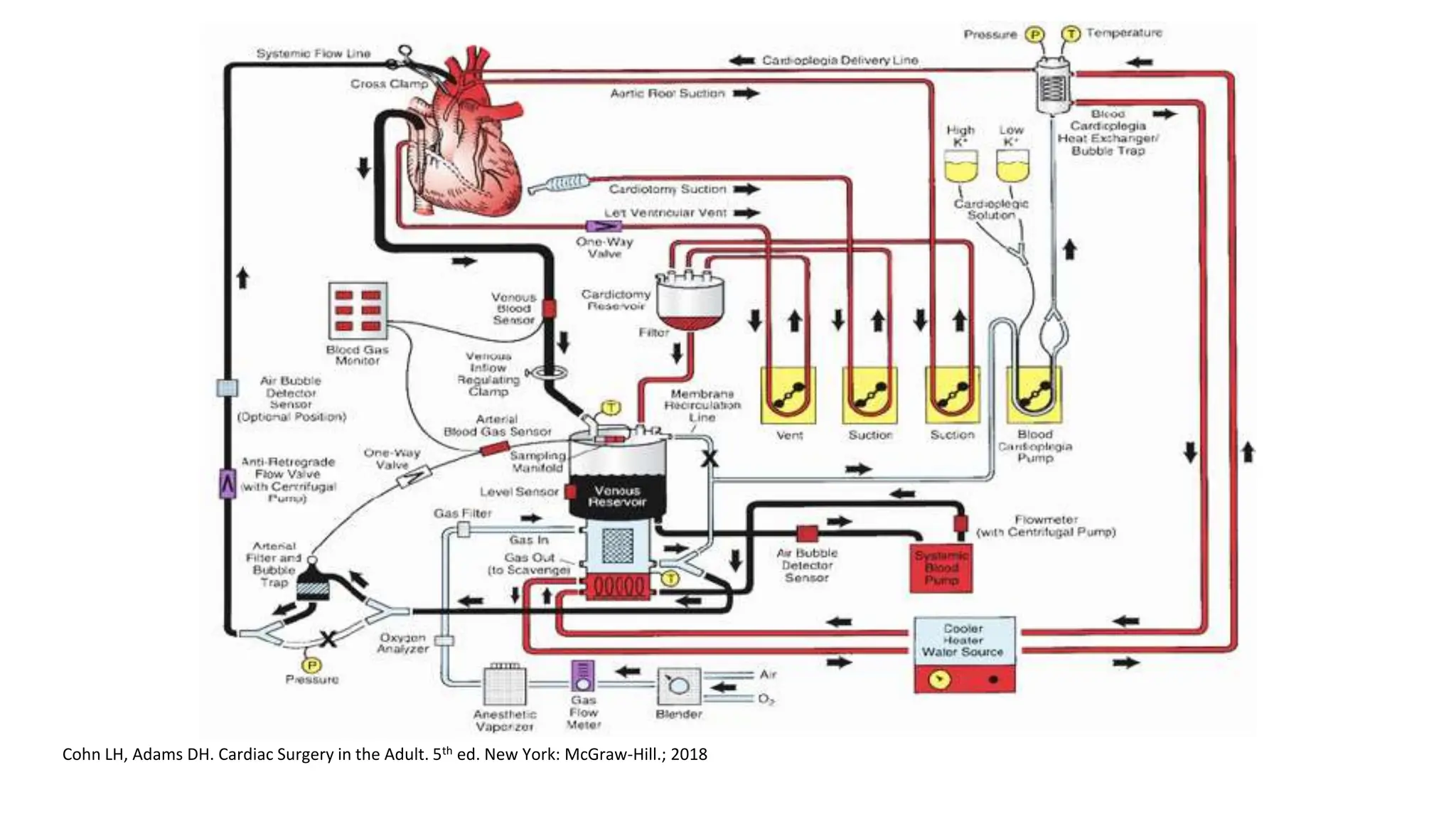
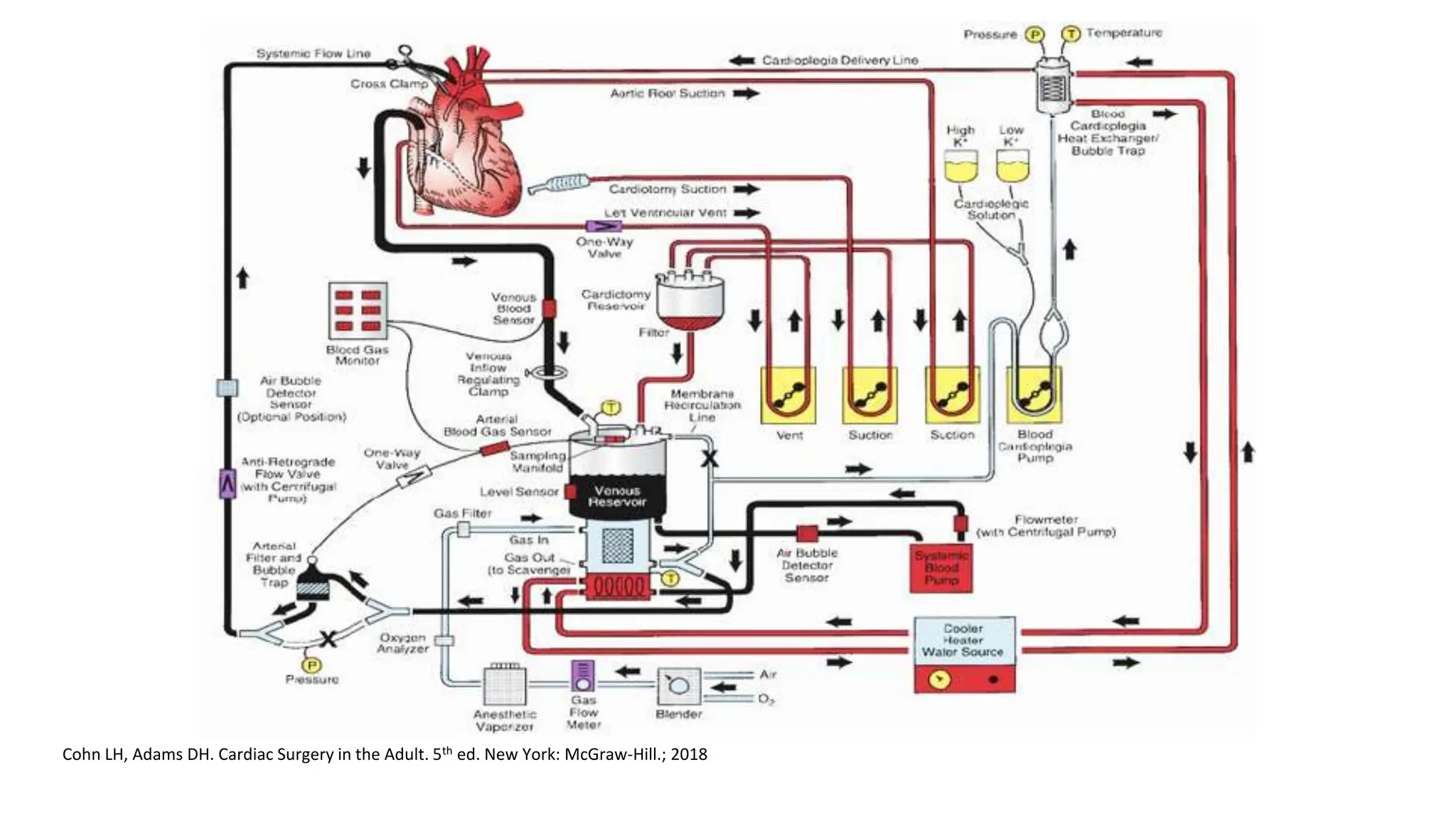
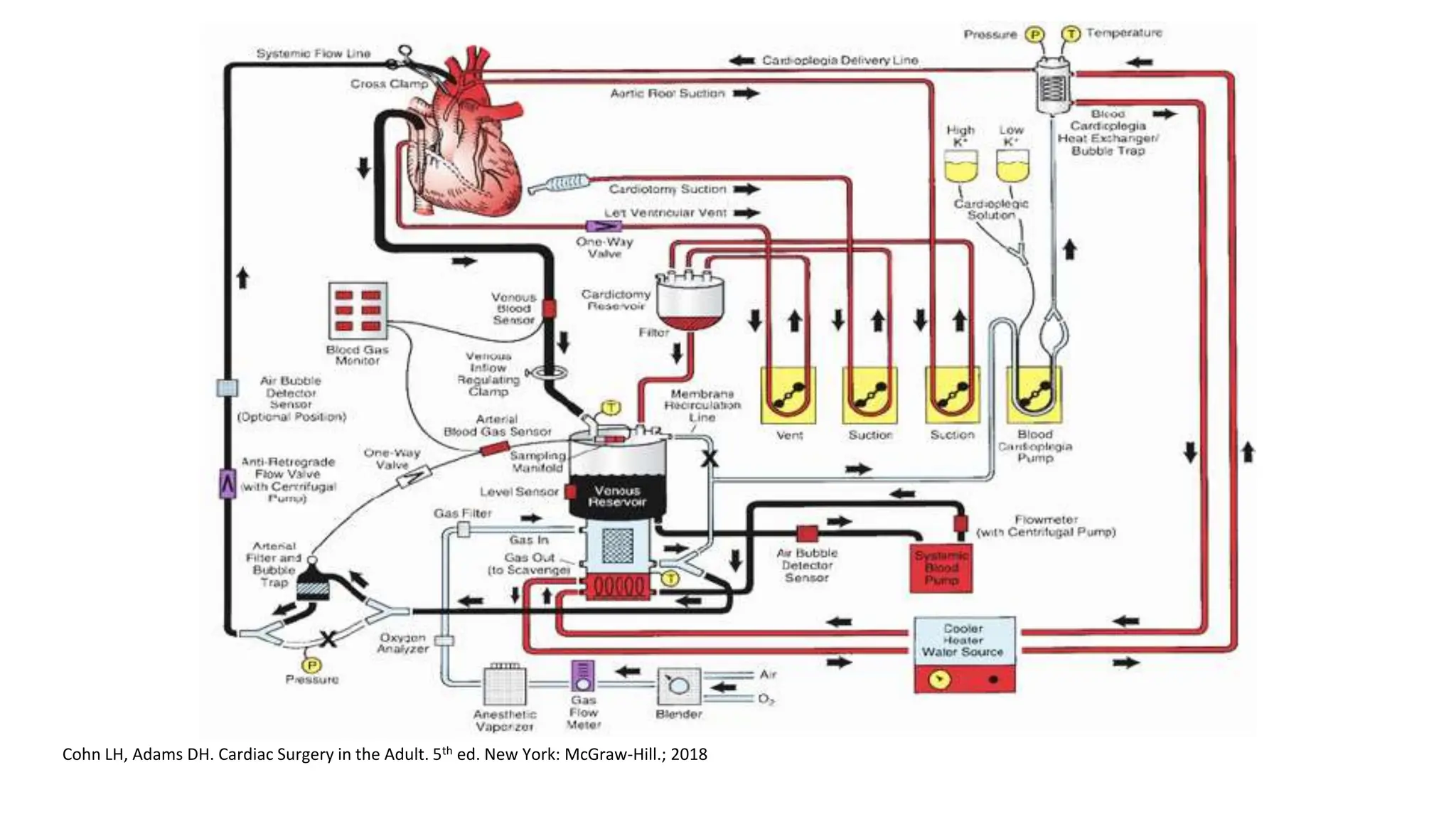
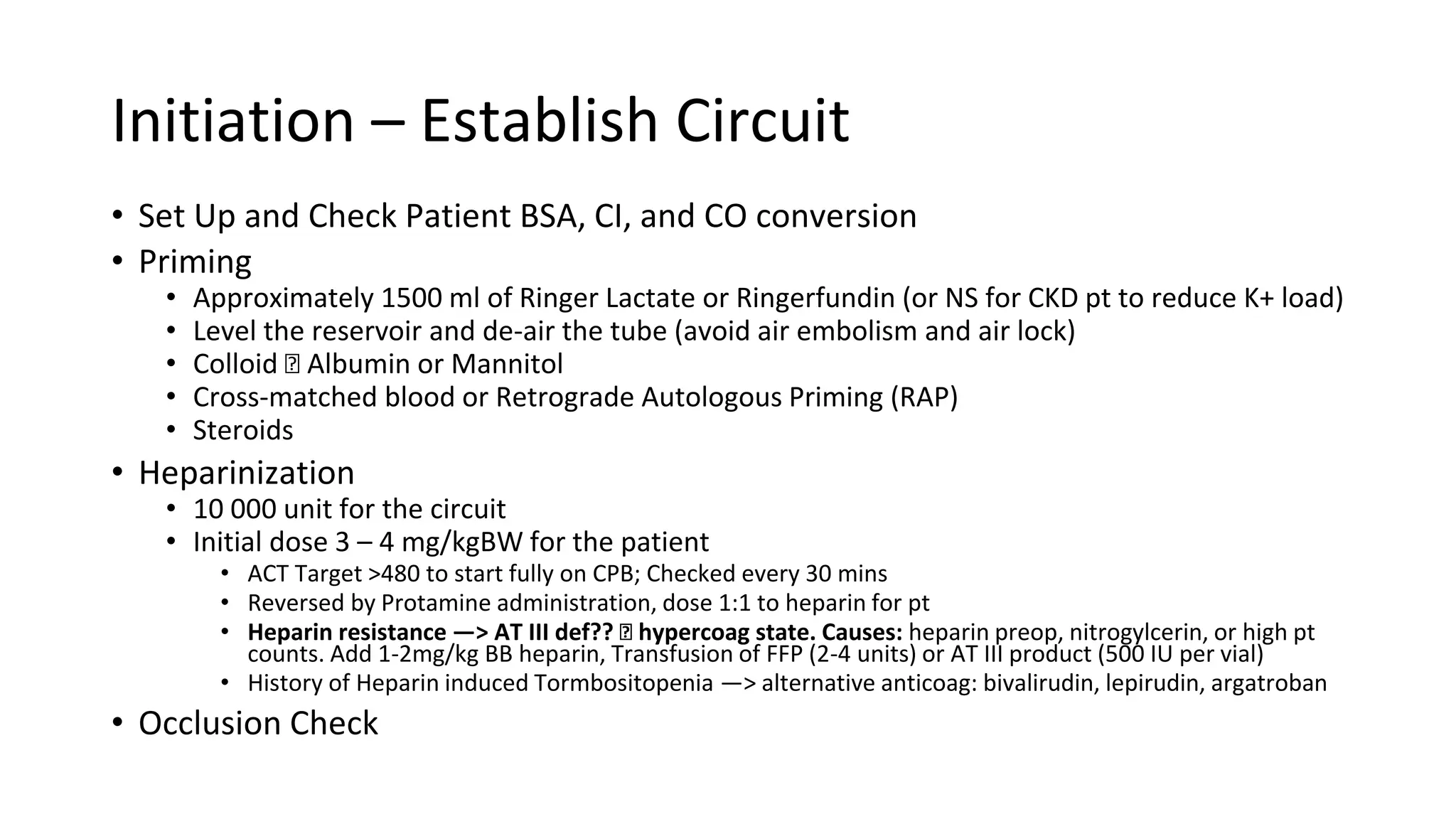
1. Set up the circuit and prime it with electrolyte solution, colloid, and heparin.
2. Administer heparin to fully anticoagulate the patient and reach the target ACT.
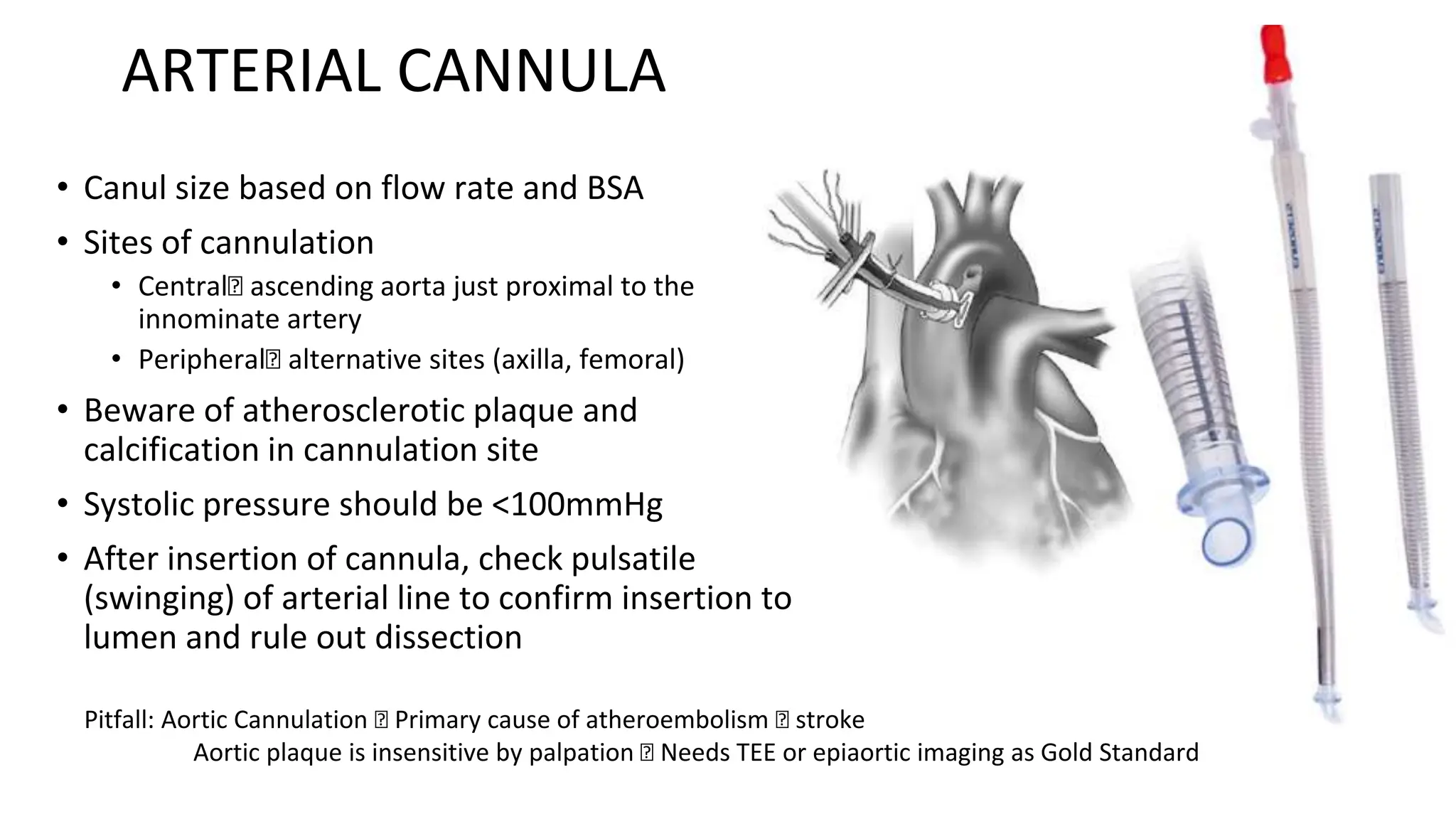
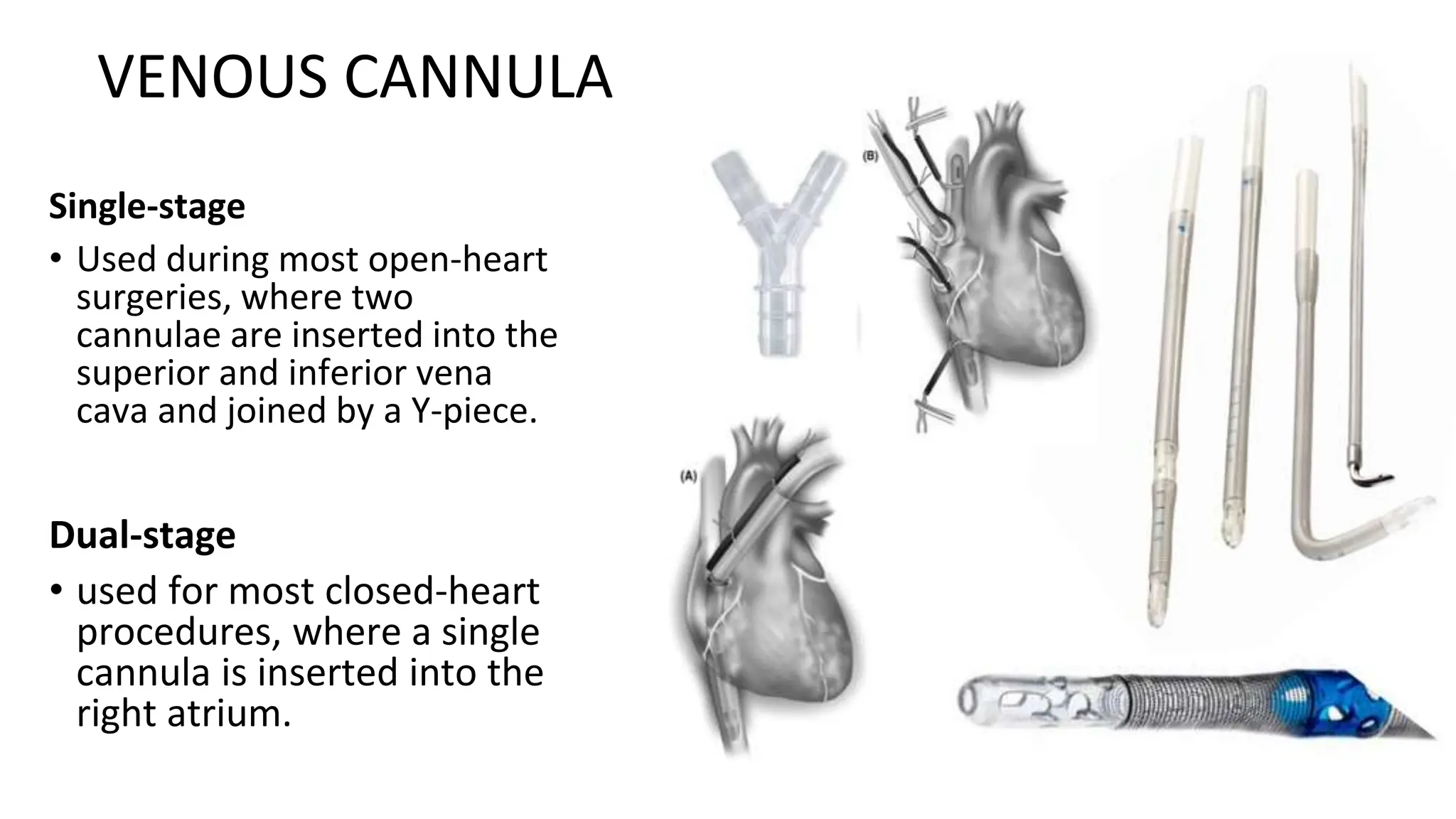
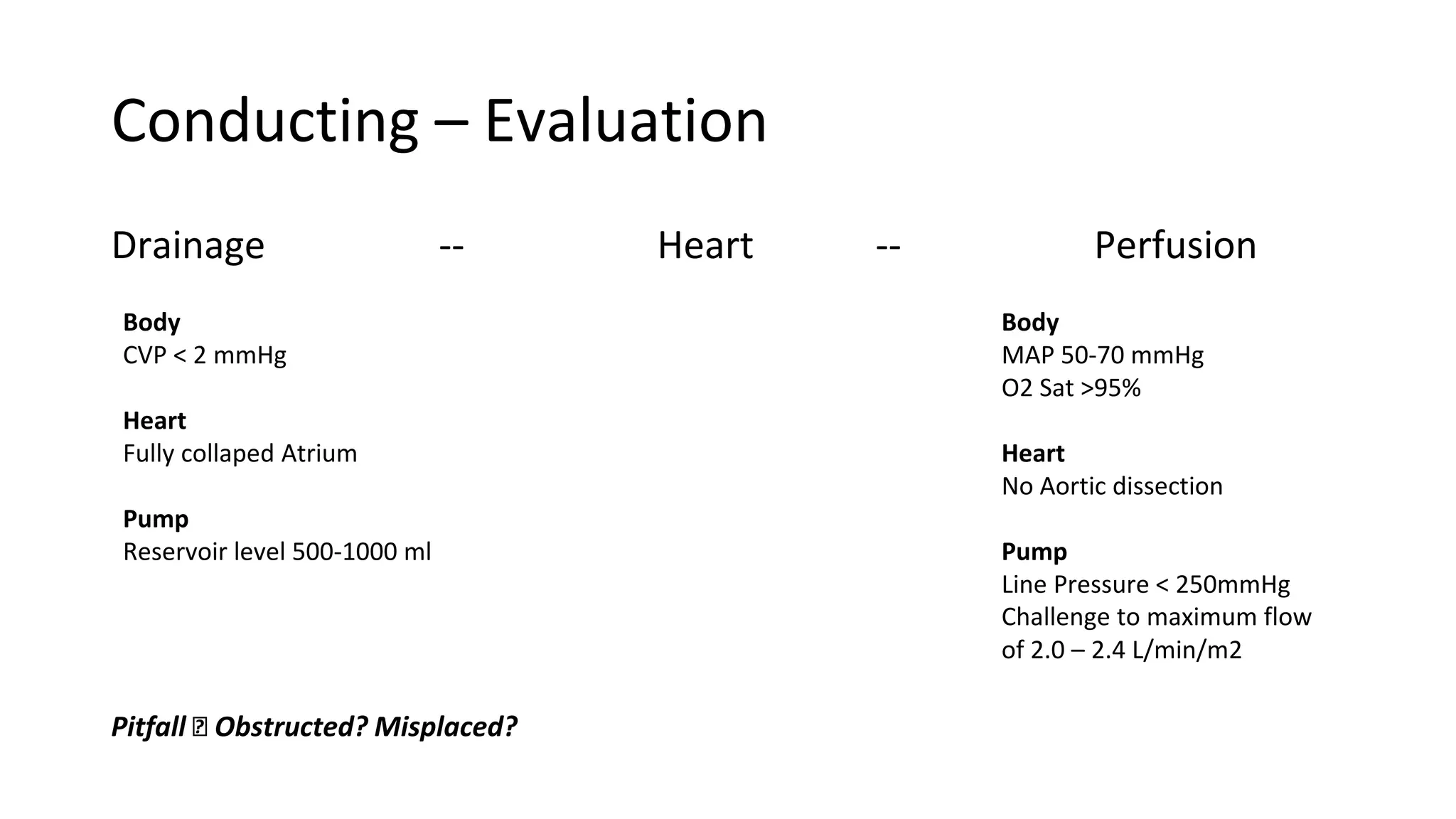
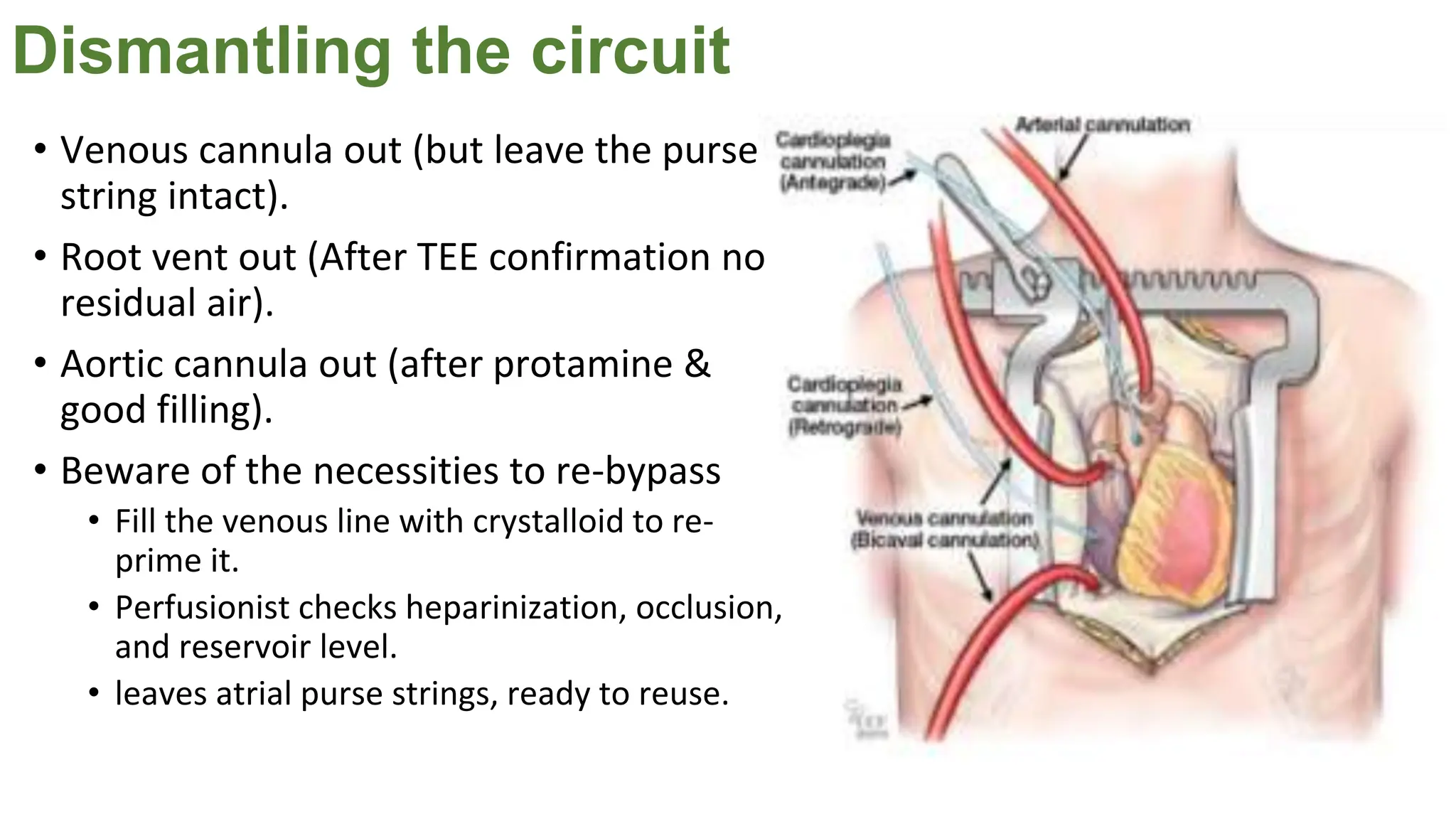
3. Cannulate the arteries and veins to establish bypass between the pump oxygenator and heart-lung machine.
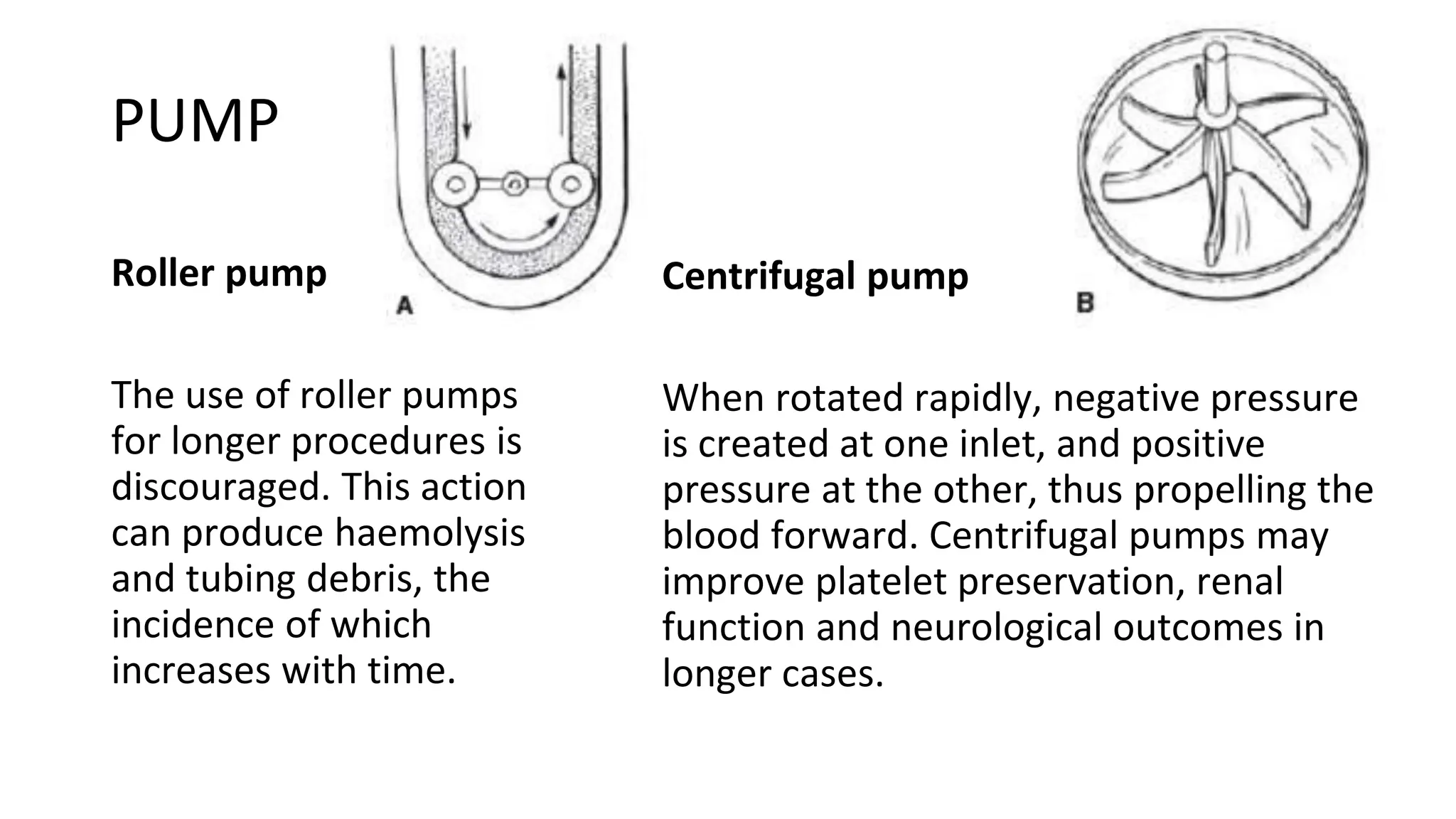
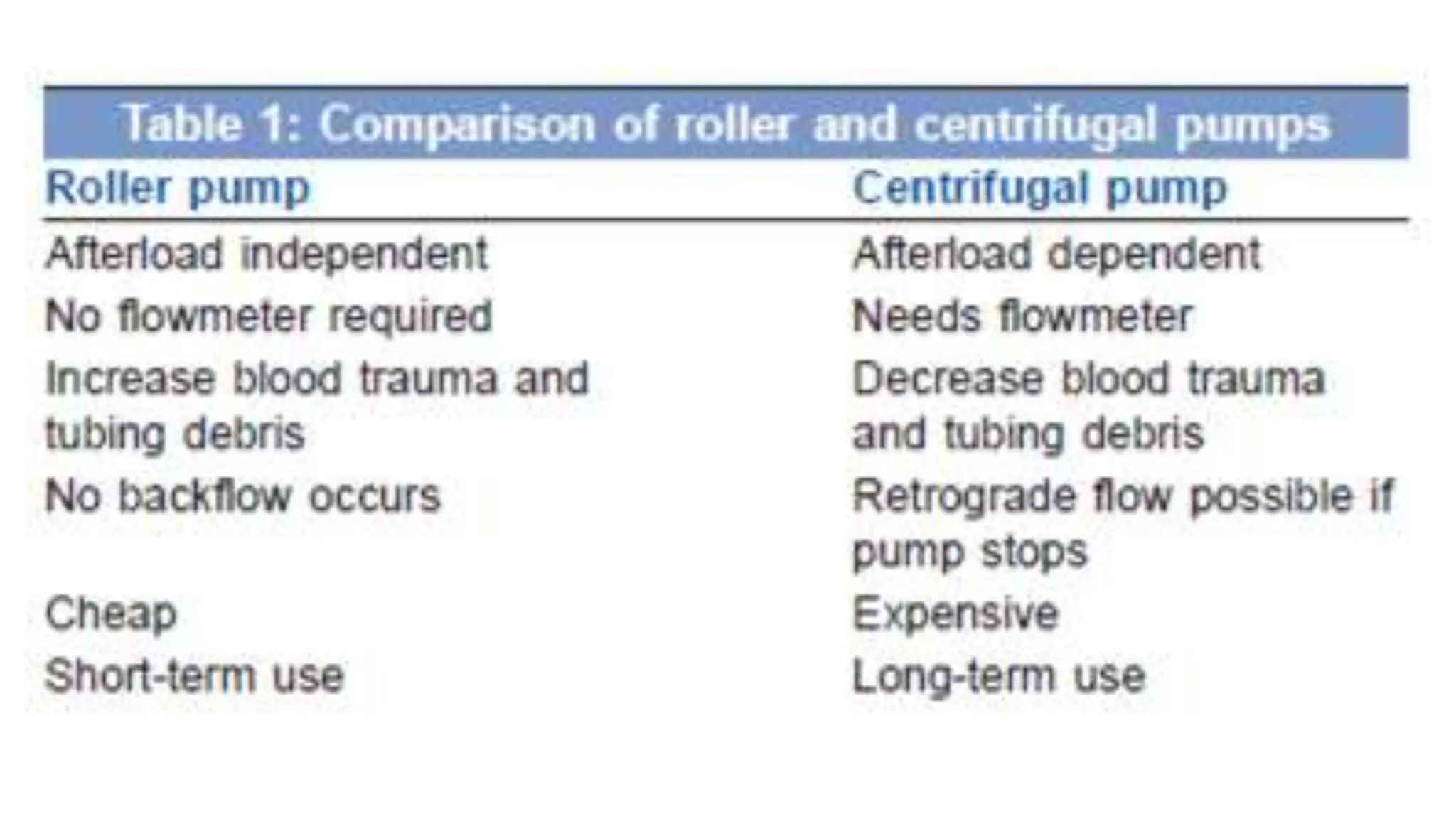
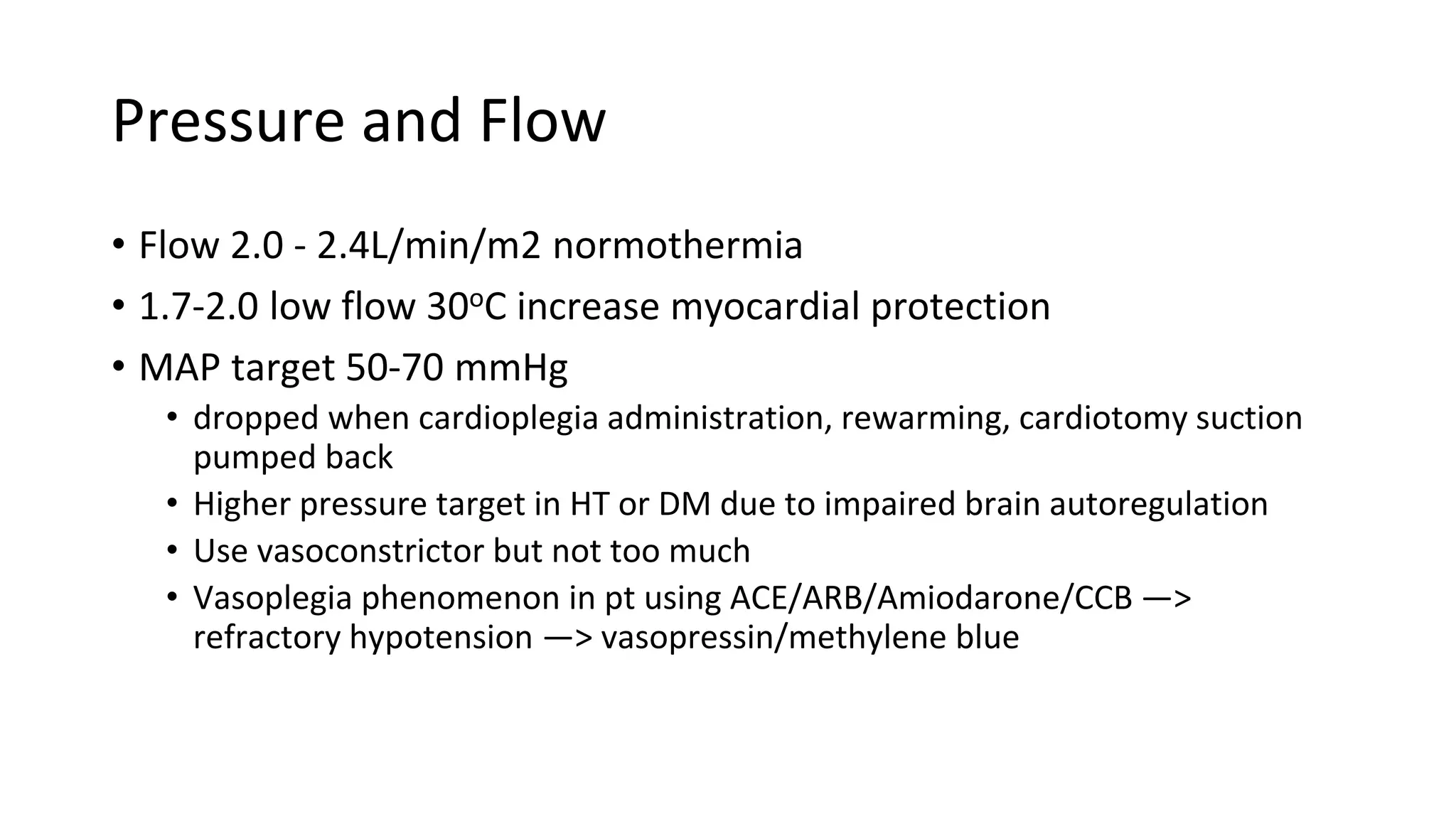
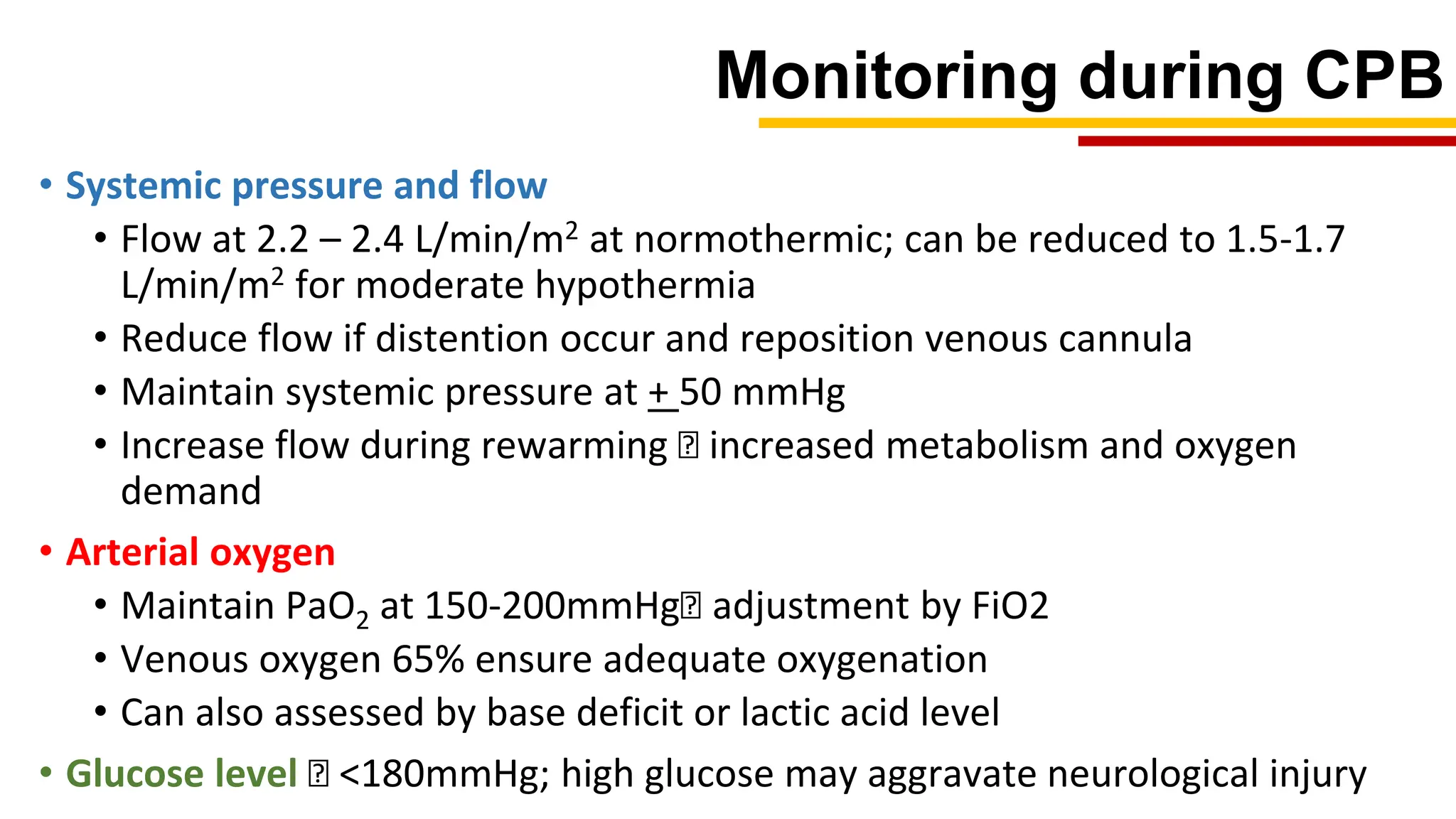
4. Slow the heart and commence cardiopulmonary bypass to oxygenate the blood and allow surgical intervention on the arrested heart.

























![References
• Bojar RM. Manual Perioperative Care in Adult Cardiac Surgery. 5th ed. Oxford: Blackwell Publishing; 2011
• Sarkar M, Prabhu V. Basics of cardiopulmonary bypass. Indian J Anaesth 2017;61:760-7.
• Mavroudis C, Backer C. Pediatric Cardiac Surgery. 4th ed. Oxford: Blackwell Publishing.; 2013
• Gravlee, G., Davis, R., Hammon, J. and Kussman, B. (2016). Cardiopulmonary bypass and mechanical
circulatory support. Philadelphia: Wolters Kluwer.
• Cohn LH, Adams DH. Cardiac Surgery in the Adult. 5th ed. New York: McGraw-Hill.; 2018
• Kouchokos NT, Blackstone EH, Hanley FL, Kirklin JK. Kirklin Barrat-Boyes Cardiac Surgery. 4th ed.
Philadelphia: Elsevier Saunders; 2013.
• Machin D, Allsager C. Principles of cardiopulmonary bypass. Continuing Education in Anaesthesia Critical
Care & Pain. 2006;6(5):176-81.
• Ismail A, Ohri S, Miskolczi S. Three-Minute Review: Essentials of Cardiopulmonary Bypass. May 2018.
doi:10.25373/ctsnet.6205661.
• Ismail A, Miskolczi SY. Cardiopulmonary Bypass. [Updated 2019 Feb 24]. In: StatPearls [Internet].
Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK482190/](https://image.slidesharecdn.com/cardiopulmonarybypass-240306112355-096847b4/75/Cardio-Pulmonary-Bypass-A-Brief-Overview-48-2048.jpg)