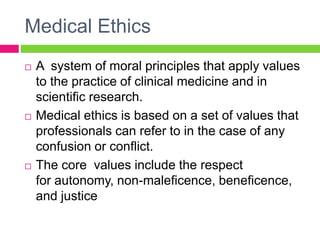
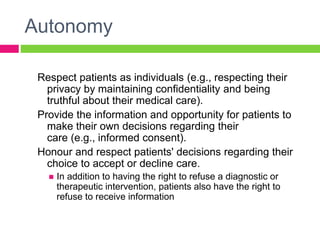
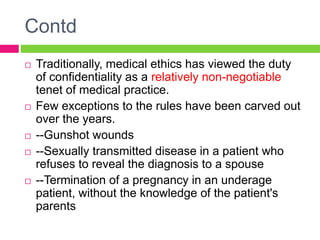
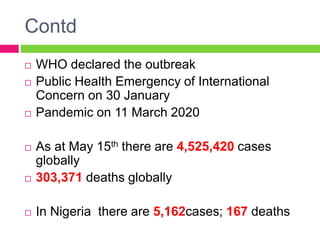
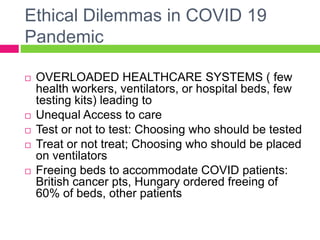
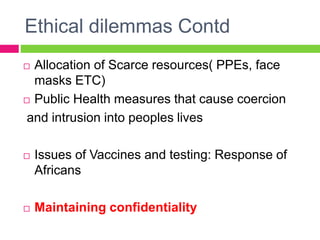
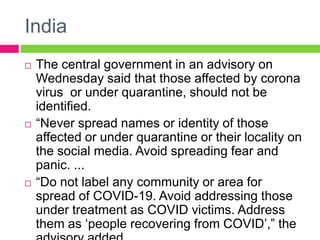
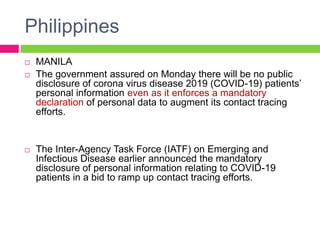
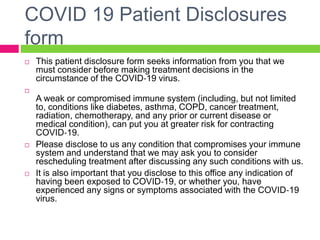
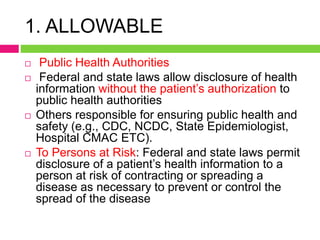
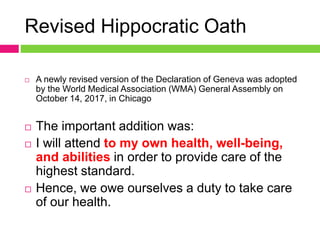
The document discusses medical ethics and disclosure principles in the context of the COVID-19 pandemic, emphasizing core values like autonomy, beneficence, and confidentiality. It highlights ethical dilemmas faced during the pandemic, such as resource allocation and maintaining patient privacy while ensuring public health. Furthermore, it outlines guidelines for disclosure related to infectious diseases, emphasizing the need for regulated approaches to information sharing and public health education.